Anaesthetic Management of a Patient with a Mobile Pedunculated Oropharyngeal Mass
Julie C R Misquith1, Karl Nicholas SA Ribeiro1
1 Assistant Professor, Department of Anaesthesiology, Kasturba Medical College, Mangalore, Karnataka, India.
2 Assistant Professor, Department of Anaesthesiology, Father Muller Medical College, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Karl Nicholas SA Ribeiro, 303, Embassy Court Apartments, Balmatta New Road, Mangalore-575001, Karnataka, India.
E-mail: juliemisquith@yahoo.com
As an anaesthesiologist, who faces several challenges in the Operating Room (OR), difficult intubation seems to be the most arduous. Anticipated difficult intubation if not planned well can be both cumbersome and disastrous. We describe the successful management of a case of anticipated difficult intubation due to a rare oropharyngeal mass, which was mobile and moved with respiration, arising from the left lateral wall of oropharynx. We used the technique of awake Fibreoptic Intubation (FOI) for intubating the trachea with dexmedetomidine infusion for sedation. Clinical findings and radiological imaging was used for assessment of difficult airway. Managing a case of difficult airway is highly individualised and meticulous planning is required in anticipated cases. A difficult airway complicates up to one tenths of cases of elective general anaesthesia. Such situations can be anticipated and tackled by fibreoptic flexible bronchoscopy assisted tracheal intubation.
Dexmedetomidine, Difficult airway, Fibreoptic intubation, Oral mass
Introduction
A 54-year-old male complained of difficulty and pain while swallowing, since two months. The patient had a sliding feeling in his throat with bouts of cough, whenever he swallowed and could ease his discomfort by manually facilitating the mass out of the way with his fingers while eating. Examination of the oral cavity and throat revealed a pendulous mobile mass arising from the lateral wall of oropharynx measuring around 6×4 cm. The patient was posted for an excision biopsy of the oropharyngeal mass and the plan was to remove it transorally under general anaesthesia.
Evaluation of patients was done, which included a detailed history, routine laboratory investigations and an all system workup. He had a haemoglobin value of 11.7 gm/100 mL, White Blood Cell (WBC) count of 9100 cells/cubic millimeters, a platelet count of 1.59 lacs/mL, serum electrolytes were within normal range with a sodium level of 137 mEq/L, and potassium level of 4.1 mEq/L, urea of 21 mg/dL, creatinine of 0.8 mg/dL, random blood glucose of 75 mg/dL, liver function tests were within normal range with a prothrombin time of 18 seconds and an INR value of 0.9.
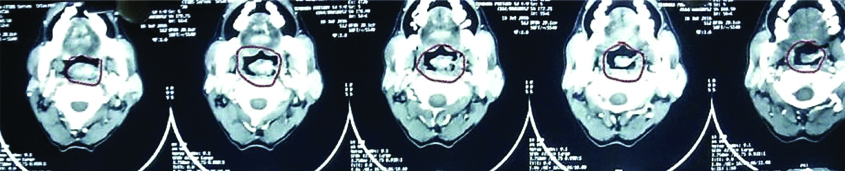
The Contrast Enhanced Computed Tomography (CECT) report suggested a heterogeneously enhancing mass in the lateral wall of the oropharynx with internal vascularity most likely a malignancy. The clinical findings and radiological imaging was used for assessment of difficult airway [Table/Fig-1]. The patient was deemed fit for surgery by a combined team of specialists that included the anaesthesiologist, the internal medicine physician and the ENT surgeon who were involved in the management and workup of this patient. The procedure was explained to the patient and written informed consent was taken. Preoperative fasting guidelines were followed.
CECT image of neck showing oropharyngeal mass arising from lateral wall of pharynx.
On arrival to the preoperative holding room, an appropriate sized intravenous cannula was secured and ringer lactate fluid was started. The patient’s nasal cavity was anaesthetised with nasal pledgets soaked with 4% lignocaine, 4 mL of 4% lignocaine nebulisation was also given to facilitate anaesthesia of the lower airways 20 minutes prior to the start of surgery. 2% lignocaine viscous gargle was given just before shifting to the OR.
In the OR, intravenous fluid infusions were continued. Monitors were connected which included five lead Electrocardiography (ECG), Non Invasive Blood Pressure (NIBP) monitoring and pulse oximetry for oxygen saturation monitoring. He was premedicated with 2 μg/kg fentanyl and 0.02 mg/kg midazolam and an infusion of dexmedetomidine 1 μg/kg/min loading dose was started over 20 minutes. Nasal cannula was put on the patient with oxygen flow at the rate of 5 L/minute. In the meantime, a transtracheal airway block with 2 mL of lignocaine was given after aspiration of air from trachea with a 26G needle connected to a syringe and a superior laryngeal nerve block was also given with 1 mL drug injected on either side. All the local anaesthetic doses were calculated bearing in mind levels of toxicity and rates of absorption.
Once patient was satisfactorily comfortable, flexible fibreoptic bronchoscope was introduced through the nasal route. On approaching the post pharyngeal wall, visibility of the glottic aperture was getting obscured with movement of the mass with respiration. As seen in [Table/Fig-2], during inspiration the mass moved forward and it moved behind as seen in [Table/Fig-3]. However, successful intubation was done by careful maneuvering of the scope around the mass and a 7.5 mm cuffed Ring Adair Elwyn (RAE) tube was passed through the trachea and was fixed after confirmation by the flexible fibreoptic bronchoscope and by the tracing of End Tidal Carbon Dioxide (EtCO2) on the monitor.
Oropharyngeal mass during inspiration.

Oropharyngeal mass during expiration.

Induction was then proceeded with propofol 2 mg/kg and neuromuscular blockade was achieved with rocuronium 1 mg/kg. Anaesthesia was maintained with N2O, O2, isoflurane 1% and intermittent doses of vecuronium as per requirement.
Surgery was performed by a transoral approach, and after the mass was excised the endotracheal tube was easily visualised as seen in [Table/Fig-4]. Surgery was uneventful and the patient was extubated at the end of the procedure after neuromuscular blockade reversal with neostigmine 0.05 mg/kg and 0.01 mg/kg glycopyrrolate. After recovery from anaesthesia he was shifted to the post anaesthesia care unit. Postoperatively, analgesia was provided with intravenous opioids. He was discharged on fourth day post surgery. The mass was sent for biopsy and the lesion was diagnosed to be a malignant spindle cell carcinoma, which is a variant of squamous cell carcinoma.
Discussion
Up to one tenths of cases of elective general anaesthesia are complicated by difficult airways. Such situations can be anticipated and tackled by fibreoptic flexible bronchoscopy assisted tracheal intubation. Patients with oral cavity mass may present to the anaesthesiologist for various diagnostic or definitive procedures. These patients may be challenging not only in view of their inherent airway problems due to tumour mass but the mass may also be associated with bleeding on touch, friability and other comorbid conditions. Pedunculated mass arising from the lateral pharyngeal wall is rare and only a few cases have been reported so far [1-3]. Anaesthetic concerns include possibility of trauma due to the growth and bleeding and also the risk of airway obstruction upon induction of general anaesthesia [4].
In a closed claims analysis, executed by the American Society of Anaesthesiologists (ASA), difficult tracheal intubation accounted for approximately 17% of adverse respiratory events for surgical patients [5]. In a recent study of 152 difficult airway cases, several factors that predicted airway difficulty were identified due to head and neck pathology [6]. These included oral cancerous tumours, history of radiotherapy and masses in supraglottic/glottic sites. Awake FOI was performed successfully in 68 (44.7%) cases [6]. The other most common airway techniques were induction with mask ventilation, followed by direct laryngoscopy (25%) and a dilator cricothyroidotomy technique (28.9%). Awake tracheostomy was performed in 1.3% of subjects.
All patients undergoing anaesthesia should have a complete history and anaesthesia focused physical examination, including assessment of the airway and factors that may influence airway management. One goal of this evaluation is to predict the degree of difficulty with ventilation and intubation. On the basis of the intubation difficulty scale, the present patient scored 2, based on the use of alternate technique that is fiberscope attempt at intubation and modified Cormack Lehan grade of incomplete glottic visualisation which did not actually fulfill many criteria of difficult intubation [7]. However, on oral examination, a mass was visualised and history of sliding feeling from patient and mobility with respiration alerted us on the possibility of an anticipated difficult airway. A FOI with a flexible fibreoptic bronchoscope is the gold standard for an anticipated difficult intubation, especially when complicated with a compromised airway [8-10]. In the present case, we were aware of the potential airway difficulty, and so supraglottic airway devices such as Laryngeal Mask Airway (LMA) and i-gel, bougie and cricothyrotomy set (with ENT surgeons on standby) were set up apart from emergency tracheostomy. We performed intubation with the patient consciously sedated using flexible fibreoptic bronchoscope. A nasotracheal intubation was done with caution as there was slight obstruction of the nasopharynx confirmed on CT [Table/Fig-2]. Using dexmedetomidine as infusion for sedation, we were able to maintain spontaneous breathing in present patient, enabling us to safely secure the airway without compromise. We relied on the advantages of the levering flexible fiberscope, as it improves the direct vision of the larynx and we could visualise the mass and carefully maneuver the scope without touching it. This case also emphasises the requirement for an ENT surgeon being immediately available to safely secure the airway in such a setting, which is highly beneficial. Other techniques that could have been used in case flexible fibreoptic bronchoscopy is not available are retromolar intubation or a submental intubation.
Visualisation of Endotracheal (ET) tube after excision of the mass.

Conclusion
From this report we conclude that, although, flexible fibreoptic bronchoscopy is gold standard in the management of difficult airways, no technique is obsolete in the management of anticipated difficult airways. The cases should be individualised and the best possible technique chosen if newer or modern aids are not available.
[1]. Shah KM, Twin pedunculated intraoral submucosal lipomaBMJ Case Rep 2013 p ii:bcr201300977410.1136/bcr-2013-00977423632621 [Google Scholar] [CrossRef] [PubMed]
[2]. Dai XM, Li YS, Liu H, Liu L, Giant pedunculated fibrolipoma arising from right facial and cervical regionJ Oral Maxillofac Surg 2009 67:1323-26.10.1016/j.joms.2008.12.03719446225 [Google Scholar] [CrossRef] [PubMed]
[3]. Persaud RA, Kotnis R, Ong CC, Bowdler DA, A rare case of a pedunculated lipoma in the pharynxEmerg Med J 2002 19:27510.1136/emj.19.3.27511971855 [Google Scholar] [CrossRef] [PubMed]
[4]. Garg R, Darlong V, Pandey R, Punj J, Anaesthesia for oncological ENT surgeries: reviewThe internet Journal of Anaesthesiology 2008 20(1)10.5580/2432 [Google Scholar] [CrossRef]
[5]. Caplan RA, Posner KL, Ward RJ, Cheney FW, Adverse respiratory events in anaesthesia: a closed claims analysisAnaesthesiology 1990 72:828-33.10.1097/00000542-199005000-000102339799 [Google Scholar] [CrossRef] [PubMed]
[6]. Iseli TA, Iseli CE, Golden JB, Jones VL, Boudreaux AM, Boyce JR, Outcomes of intubation in difficult airways due to head and neck pathologyEar Nose Throat J 2012 91(3):E1-E5.10.1177/01455613120910031322430340 [Google Scholar] [CrossRef] [PubMed]
[7]. Adnet F, Borron SW, Racine SX, Clemessy JL, Fournier JL, Plaisance P, Lapandry C, The Intubation Difficulty Scale (IDS): proposal and evaluation of a new score characterizing the complexity of endotracheal intubationAnaesthesiology 1997 87:1290-97.10.1097/00000542-199712000-000059416711 [Google Scholar] [CrossRef] [PubMed]
[8]. Thierbach AR, Werner C, Infraglottic airway devices and techniquesBest Pract Res Clin Anaesthesiol 2005 19:595-609.10.1016/j.bpa.2005.06.00116408536 [Google Scholar] [CrossRef] [PubMed]
[9]. Dabbagh A, Mobasseri N, Elyasi H, Gharaei B, Fathololumi M, Ghasemi M, A rapidly enlarging neck mass: the role of the sitting position in fibreoptic bronchoscopy for difficult intubationAnaesth Analg 2008 107:1627-29.10.1213/ane.0b013e318184f82518931222 [Google Scholar] [CrossRef] [PubMed]
[10]. Ovassapian A, Fibreoptic endoscopy and the difficult airway 1996 2nd edPhiladelphia, PALippincott-Raven Press [Google Scholar]