Rectal Necrosis: A Rare Complication of Palliative Radiotherapy for Sacral Spine Metastasis
Seyed Jalal Eshagh Hosseini1, Adnan Tizmaghz2, Bahram Andalib3, Ghazaal Shabestanipour4
1 Assistant Professor, Department of Surgery, Qom University of Medical Sciences, Qom, Iran.
2 Assistant Professor, Department of Surgery, Iran University of Medical Sciences, Tehran, Iran.
3 Clinical Oncologist, Department of Oncology, Alborz University of Medical Sciences, Karaj, Alborz, Iran.
4 General Physician, Department of Surgery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Adnan Tizmaghz, Iran University of Medical Sciences, Shahid Hemmat Highway, Tehran-1449614535, Iran.
E-mail: adnan_ti@yahoo.com
Radiation proctocolitis is a common side effect of radiation therapy. In rare cases, chronic radiation injury can be severe enough to cause rectal necrosis. In this study, a case of rectal necrosis after sacral spine radiotherapy was presented. Anterior rectal wall necrosis and rectovaginal fistula is thought to be rare, severe and challenging rectal long-term complication of the previous sacral spine irradiation. Although, rectovaginal fistula which resulted in intractable rectal bleeding seems to be a rare side-effect of radiotherapy, physicians must not forget about this complication, as it can be fatal in patients who often have been cured of cancer.
Bone metastasis, Complication, Radiation, Rectal bleeding
Case Report
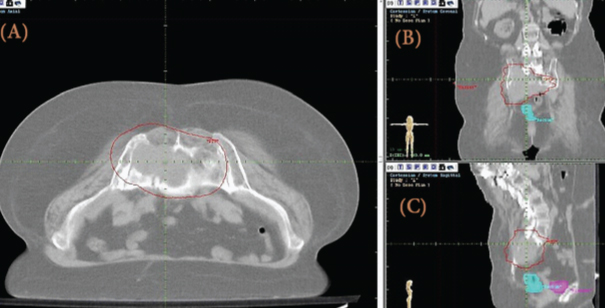
A 61-year-old woman presented to the Oncology outpatient department with occasional slight blood-stained stool, associated with mild to moderate anal pain for since 25 days. Her symptoms have been constant and gradually worsening in intensity. She had the personal history of the left breast cancer diagnosed two years ago, for which the patient was treated with left breast lumpectomy plus whole breast radiation and hormonal therapy. Sacral spine metastasis was detected seven months after primary diagnosis, in follow-up [Table/Fig-1].
A) Spine transverse; B) coronal; and C) sagittal CT-scan simulation site for targeted large lytic lesion of sacral vertebrae of 8.6×5.6×6.7 cm in size involving S1, S2, and S3 vertebra, extending to the neural foramina of the involved vertebra.
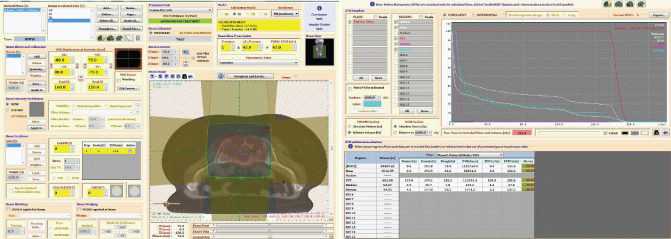
The patient had undergone treatment with high-dose extended field Three-Dimensional Conformal Radiation Therapy (3DCRT) of the sacral spine with a total dose of 60 Gy (6000 rads) in 24 fractions [Table/Fig-2]. There was no significant adverse effect during the acute phase except mild acute cystitis and mild proctitis.
3DCRT plan of the A) sacral spine and B) dose-volume histograms.
During the initial 18 months of three-dimensional radiation treatment planning apart from mild itching in her anus, she was otherwise symptom-free.
She was in her usual state of health until 25 days ago when a slight blood-stained stool developed. The physical examination was unremarkable except for mild perineal dermatitis and vaginal discharge. So, the patient admitted for further diagnostic workup. The last pelvic Computed Tomography (CT) scan revealed that lytic lesion of sacral vertebrae involving S1, S2, and S3 vertebra, extending to the neural foramina of the involved vertebra [Table/Fig-1]. Colonoscopy on this admission revealed few rectal angioectasia and multiple irregular necrotic ulcers distributing circumferentially in 15-35 cm from the anal verge. Examination under anaesthesia confirmed a large anterior rectal ulcer about 9 cm from the anal verge. Biopsies were taken and histology revealed an ischemic colitis with coagulation necrosis in the area of the rectal ulcer. Serum tumour markers {Cancer Antigen (CA) 19-9, CA 15-3, Carcinoembryonic Antigen (CEA)} were within normal limits. The patient had undergone medical treatment with Asacol {anti-inflammatory- 5-Aminosalicylic Acid (5-ASA) preparations}, Sucralfate (protective barrier and promote epithelial healing), Metronidazole (Antibiotic) and a Hydrocortisone (anti-inflammatory-steroid preparations) enema. However, the patient has continued having rectal bleeding and significant drop in haematocrit was occurred. At this point, the patient underwent surgical removal of affected rectum and distal sigmoid colon due to intractable bleeding. During surgery, severe adhesions between uterus and rectum and fistulisation of rectum to uterus with full thickness necrosis extending from recto-sigmoid junction to the dentate line were found. Excision of the rectum and sigmoid colon with anastomosis of descending colon and anus were performed. Rectal specimen revealed transmural necrosis with extensive mucosal ulceration.
Following the surgery rectal bleeding was stopped and patient postoperative period was uneventful and she was discharged home on the seventh day.
Discussion
Acute radiation proctocolitis is a common side effect of radiation therapy, occurring in 50-75% of patients receiving radiation to the pelvis [1]. Chronic radiation proctocolitis is an indolent process that can arise in approximately 5-15% of patients who had pelvic radiation therapy and typically become evident any time up to two years after the cessation of therapy, although onset of clinical manifestations may be delayed beyond two years and in some cases have occurred decades later [2]. In this case, chronic radiation injury becomes evident after 18 months. On rare occasions, chronic radiation injury can be severe enough to cause rectal wall perforation or necrosis. In most cases, injury occurs in patients who have received at least 4500 cGy [3]. Similarly, present patient has received 6000 cGy in her in their pelvic radiation course. So far, there have been few cases of radiation induced rectal necrosis recognised and diagnosed whom were almost always treated with concurrent radiosensitive agents with or without bevacizumab [4,5]. In contrast to these reports, our patient had not been given any concomitant radiosensitising agent. Hence, anterior rectal necrosis still remains poorly defined and is an underestimated problem in oncology. This abnormality is thought to be late severe and challenging rectal effect of the previous pelvis irradiation.
Risk factors for acute radiation proctocolitis include conditions that may limit splanchnic perfusion such as hypertension, diabetes mellitus, coronary artery disease, heavy smoking and restricted mobility of the small intestine due to adhesions [6]. Thus, diabetic cancer patients treated with radiation therapy have improved outcomes if they take metformin to control their diabetes [7].
Also, injury can be potentiated by concomitant administration of chemotherapeutic agents such as gemcitabine, 5-fluorouracil, doxorubicin, dactinomycin and methotrexate that act as radiation sensitizers [8]. The Multi-Leaf Collimators (MLC) is important tool used on linear accelerator that could significantly minimise damage to surrounding healthy tissue by reducing the out-of-field dose due to a reduction in scatter from the primary and secondary collimator, transmission through the collimator and head leakage [9].
Rectal epithelium’s capacity for regeneration could help the mucosal radiation injury to repair without any intervention after the cessation of radiation therapy [10].
In contrast, chronic radiation proctitis is characterised by a progressive occlusive vasculitis that leads to chronic ischaemia and fibrosis that affects all layers of the rectal wall, rather than the mucosa alone. These changes can lead to strictures, abscesses, and fistulas, which are responsible for the clinical manifestations of chronic radiation proctitis [11].
Although, rectal bleeding is most often the presenting symptom of chronic proctitis in the setting of prior radiation, similar to present patient, it should not be assumed that this is the sole cause. In fact, endoscopic findings reveal that one third of diagnoses in this setting were unrelated to the previous radiotherapy and significant neoplasia was noted in 12% [12].
Patients with more severe acute radiation proctocolitis seem to be prone to chronic proctocolitis. However, the lack of early complications does not guarantee the lack of late chronic radiation-induced injury [13].
Because clinical symptoms alone are unreliable for the diagnosis of radiation proctitis, endoscopic evaluation is mandatory with any new onset of hematochezia after prior radiation therapy [14].
Conclusion
Although late rectal necrosis following pelvic radiation seems to be an extremely rare, physicians must keep in mind about this complication, as it can be fatal in patients who often have been cured of cancer. Late rectal wall necrosis and radiation fistula should be considered in the differential diagnosis if the patient received pelvic radiation doses greater than 4500 cGy. The clinical and endoscopic evaluation of rectal wall necrosis is not always conclusive. However, endoscopic evaluation and biopsy are necessary for diagnosis, especially for those with history of repeated and prolonged symptoms. Surgery is a viable diagnostic and therapeutic option in patients with persistent symptoms and equivocal endoscopic findings.
[1]. Do NL, Nagle D, Poylin VY, Radiation proctitis: current strategies in managementGastroenterology Research and Practice 2011 2011:91794110.1155/2011/91794122144997 [Google Scholar] [CrossRef] [PubMed]
[2]. Wu X-r, Liu X-l, Katz S, Shen B, Pathogenesis, diagnosis, and management of ulcerative proctitis, chronic radiation proctopathy, and diversion proctitisInflammatory Bowel Diseases 2014 21(3):703-15.10.1097/MIB.000000000000022725687266 [Google Scholar] [CrossRef] [PubMed]
[3]. Grodsky MB, Sidani SM, Radiation proctopathyClinics in Colon and Rectal Surgery 2015 28(2):10310.1055/s-0035-154733726034407 [Google Scholar] [CrossRef] [PubMed]
[4]. Okuda T, Tsuji H, Kitagawa S, Yamada S, A case report of rectal perforation associated with bevacizumab treatment after carbon ion radiotherapy for recurrent rectal cancerInternational Cancer Conference Journal 2013 2(4):220-23.10.1007/s13691-013-0095-9 [Google Scholar] [CrossRef]
[5]. Birgisson H, Påhlman L, Gunnarsson U, Glimelius B, Late adverse effects of radiation therapy for rectal cancer- A systematic overviewActa Oncologica 2007 46(4):504-16.10.1080/0284186070134867017497318 [Google Scholar] [CrossRef] [PubMed]
[6]. Lilla C, Ambrosone CB, Kropp S, Helmbold I, Schmezer P, von Fournier D, Predictive factors for late normal tissue complications following radiotherapy for breast cancerBreast Cancer Research and Treatment 2007 106(1):143-50.10.1007/s10549-006-9480-917221151 [Google Scholar] [CrossRef] [PubMed]
[7]. Koritzinsky M, Metformin: A novel biological modifier of tumour response to radiation therapyInternational Journal of Radiation Oncology Biology Physics 2015 93(2):454-64.10.1016/j.ijrobp.2015.06.00326383681 [Google Scholar] [CrossRef] [PubMed]
[8]. Citrin DE, Mitchell JB, Altering the response to radiation: Sensitizers and protectorsSeminars in Oncology 2014 Elsevier10.1053/j.seminoncol.2014.09.01325499642 [Google Scholar] [CrossRef] [PubMed]
[9]. Zelefsky MJ, Levin EJ, Hunt M, Yamada Y, Shippy AM, Jackson A, Incidence of late rectal and urinary toxicities after three-dimensional conformal radiotherapy and intensity-modulated radiotherapy for localized prostate cancerInternational Journal of Radiation Oncology Biology Physics 2008 70(4):1124-29.10.1016/j.ijrobp.2007.11.04418313526 [Google Scholar] [CrossRef] [PubMed]
[10]. Hauer-Jensen M, Denham JW, Andreyev HJN, Radiation enteropathy-pathogenesis, treatment and preventionNature Reviews Gastroenterology and Hepatology 2014 11(8):470-79.10.1038/nrgastro.2014.4624686268 [Google Scholar] [CrossRef] [PubMed]
[11]. Lordick F, Geinitz H, Theisen J, Sendler A, Sarbia M, Increased risk of ischemic bowel complications during treatment with bevacizumab after pelvic irradiation: report of three casesInternational Journal of Radiation Oncology Biology Physics 2006 64(5):1295-98.10.1016/j.ijrobp.2005.12.00416503384 [Google Scholar] [CrossRef] [PubMed]
[12]. Andreyev HJN, Vlavianos P, Blake P, Dearnaley D, Norman AR, Tait D, Gastrointestinal symptoms after pelvic radiotherapy: Role for the gastroenterologist?International Journal of Radiation Oncology Biology Physics 2005 62(5):1464-71.10.1016/j.ijrobp.2004.12.08715927411 [Google Scholar] [CrossRef] [PubMed]
[13]. Kennedy GD, Heise CP, Radiation colitis and proctitisClinics in Colon and Rectal Surgery 2007 20(1):6410.1055/s-2007-97020220011363 [Google Scholar] [CrossRef] [PubMed]
[14]. Weiner JP, Wong AT, Schwartz D, Martinez M, Aytaman A, Schreiber D, Endoscopic and non-endoscopic approaches for the management of radiation-induced rectal bleedingWorld Journal of Gastroenterology 2016 22(31):697210.3748/wjg.v22.i31.697227610010 [Google Scholar] [CrossRef] [PubMed]