Osseous Metaplasia of Juvenile Polyp
Vinitkumar Deshmukh1, Abhijit Jagdale2, Rahul Dhake3, Deepak Naik4
1 Senior Registrar, Department of Surgery, BJGMC and Sassoon Hospital, Pune, Maharashtra, India.
2 Assistant Professor, Department of Surgery, BJGMC and Sassoon Hospital, Pune, Maharashtra, India.
3 Consultant Pathologist, Department of Pathology, Inlaks and Budhrani Hospital, Pune, Maharashtra, India.
4 Consultant Surgeon, Department of Surgery, Inlaks and Budhrani Hospital, Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Abhijit Jagdale, Sn-19, Gondhale Nagar, Hadapsar, Pune-411028, Maharashtra, India.
E-mail: abhijitjagdale111285@gmail.com
Bone formation in the gastrointestinal tract is very uncommon. We came across a case of 12-year-old boy with rectal bleeding because of rectal polyp. Snare resection of that polyp was done, and pathology report was suggestive of juvenile polyp with osseous metaplasia. There are only 6-7 similar cases which were reported worldwide. There is striking similarity in presentation and histopathological findings of these patients. This study also tries to throw some light on possible pathological mechanism of osseous metaplasia.
Histopathology, Inflammation, Stem cell
Case Report
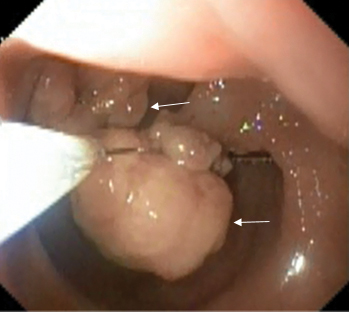
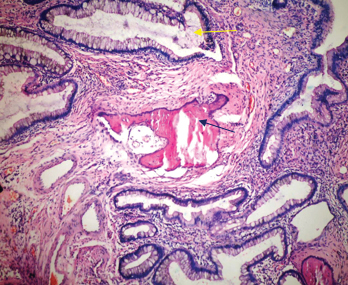
A 12-year-old boy presented to general surgery OPD with complaints of recurrent painless bleeding per rectum for 7-8 months especially after hard stools. His other elder sibling was normal with no similar complains. Haematological investigations were suggestive of mild anaemia. Colonoscopy was performed and was suggestive of two pedunculated polyps in the rectum 8-10 cm from the anal verge side by side [Table/Fig-1]. Snare polypectomy was performed. Gross specimen measured 1×2×2 cm and 0.5×1×1 cm in size. Histopathologically, it was juvenile polyp with hamartomatous tissue and multiple cystic dilated glands. To our surprise there were 4-5 islands of osseous metaplasia separated from glandular tissue by fibrous connective tissue [Table/Fig-2]. Osseous metaplasia was present in both polyps. Inflammatory cell infiltrate was present throughout the fibrous stroma. There was no evidence of atypia or malignancy. Patient recovered well and discharged with oral dose of liquid haematinics preparation. He was devoid of any complaints after one month. Follow up colonoscopy was advised after six months.
Colonoscopy view of polyps (white arrow).
Haematoxylin and eosin staining showing juvenile hamartomatous polyp with osseous metaplasia (black arrow), yellow arrow showing gland (10X).
Discussion
Patient discussed in present case report presented with painless bleeding per rectum for which colonoscopy was done. Hyperplastic polyps, inflammatory polyps, hamartomatous polyp like Peutz-Jeghers syndrome, rarely neoplastic polyps associated with adenomatous polyposis coli, hereditary nonpolyposis colon cancer can present with the similar complaints [1]. Being the most common polyp of paediatric age group and rectum as the most common location, we suspected the type of polyp in current patient as juvenile polyp which was confirmed on histopathology [2,3]. Colonoscopy and if needed, then endoscopic intervention are the standard treatment for bleeding per rectum. In the present case, rectal polyp was found as the main reason for bleeding per rectum.
Epithelial metaplasia is an adaptive process resulting from the transformation of one type of epithelium into another type with a different structure and function [4]. Juvenile polyps are relatively common under 10 years of age (up to 2%) and occur most commonly at rectosigmoid region and presenting as recurrent bleeding per rectum. These are non neoplastic hamartomatous polyp and consist of dilated cystic spaces, inflammation, increased vascularity and areas of tissue destruction. Usually these polyps are 1-3 cm in size, smooth, red and tend to bleed easily [5].
There are only few cases reported in literature with osseous metaplasia in juvenile polyps given in [Table/Fig-3]. Surprisingly only one patient was female, others were male [6-11]. Todd I, studied 25 patients with juvenile polyp where 15 patients were male, and 10 patients were female [12]. This shows that there is male preponderance. All patients were below 15 years of age. Polyps were located in rectum with variable distance from anal verge. On histopathology, inflammatory infiltrate was the strikingly common feature of all specimens [6-11].
Comparison of present case with other reports on osseous metaplasia of juvenile polyp published in literature.
| Reported by | Location and gross morphology | Age/sex | Prominent histopathological findings | Presentation |
|---|
| Current patient, India, 2017 | Pedunculated polyps 2 in number, 8-10 cm from the anal verge in rectum, side by side, largest 1×2×2 cm | 12/M | 4-5 islands of osseous metaplasia Inflammatory cell infiltrate throughout fibrous stroma | Rectal bleeding for 7-8 months |
| Marks MM and Atkinson KG, Kansas, USA 1964 [6] | Rectal polyps, 2 in number, on posterior wall, 7 cm above anal verge, largest measuring 2×1×0.7 cm | 10/M | Marked infection and inflammation, one polyp showed bone tissue | Painless rectal bleeding since 6 months |
| Ahmed R et al., Pakistan, 2009 [7] | Solitary polypoidal lesion in upper rectum, 1×0.6 cm without stalk | 15/M | Ulcerated surface. composed of cystic and dilated crypts filled with neutrophils and inspissated mucin, Foci of osseous metaplasia, lamina propria with inflammatory infiltrate | Bleeding per rectum since 3 months |
| Garg M et al., India, 2013 [8] | Rectal polyp, mass protruding from anus. Solitary polypoidal 1.5×1×0.5 cm | 6/M | Lamina propria infiltrated by mixed acute and chronic inflammatory cell infiltrate along with granulation tissue, dilated crypts filled with mucinous material, bony trabeculae | Mass protruding from anus, blood mixed with stools since 5 months |
| Bhattacharya N and Sarkar T, India 2013 [9] | Rectal polyp, 1 cm in size, 5 cm away from anal verge | 14/M | Ulcerated, with granulation tissue, oedema and a mixed inflammatory cell infiltrate, bony trabeculae in lamina propria | Rectal bleed since 1 month |
| Haynes HR et al., UK 2017 [10] | Single pedunculated polyp 1.5 cm in maximum diameter in the rectosigmoid colon | 6/M | Areas of mucosal ulceration, dilated colonic crypts and a chronic inflammatory cell infiltrate, polyp stalk showed metaplastic ossification. | Rectal bleed since 1 year |
| Bhat V et al., [11] | Upper rectum | 5/F | Extravasated mucin and mixed inflammatory cell infiltrate | Rectal bleeding |
There are two theories for the metaplastic conversion of normal epithelium. According to first theory, inflamed tissue changes differentiation of the stem cells to metaplastic epithelium. Second theory says chronic inflammation leads to tissue inflammation and stem cell failure. This event induces recruitment of the bone marrow stem cells into the tissue stem cell niche. Factors secreted by inflammatory infiltrate alters bone marrow niche environment which leads to metaplastic differentiation of bone marrow stem cell [4].
It is reported and proved in rat model experiments that adenocarcinoma can produce osseous tissue in the stroma. In the cell line and carcinogenesis experiment, it is thought that the osseous tissue may have been produced by mesenchymal cells rather than epithelial cells, and mesenchymal cells may be affected to produce osseous tissue by some factor, probably from transformed epithelial cells such as carcinoma cells [13].
Conclusion
Chronic inflammation is the constant feature of the juvenile rectal polyps associated with osseous metaplasia. Chronic inflammation can cause osseous metaplasia in some patients of juvenile polyp.
[1]. AkA VK, Aster JC, Robbins and Cotran Pathologic Basic of Disease. 9th ed. R. Turner J, editor 2015 PhiladelphiaElsevier:804-12. [Google Scholar]
[2]. Poddar U, Thapa BR, Vaiphei K, Singh K, Colonic polyps: experience of 236 Indian childrenAmerican Journal Gastroenterology 1998 93(4):619-22.10.1111/j.1572-0241.1998.176_b.x9576458 [Google Scholar] [CrossRef] [PubMed]
[3]. Pillai RB, Tolia V, Colonic polyps in children: frequently multiple and recurrentClinical Pediatrics 1998 37(4):253-57.10.1177/0009922898037004069564575 [Google Scholar] [CrossRef] [PubMed]
[4]. Herfs M, Hubert P, Delvenne P, Epithelial metaplasia: adult stem cell reprogramming and (pre) neoplastic transformation mediated by inflammation?Trends in Molecular Medicine 2009 15(6):245-53.10.1016/j.molmed.2009.04.00219457719 [Google Scholar] [CrossRef] [PubMed]
[5]. Pohl J, Solitary juvenile polypVideo Journal and Encyclopedia of GI Endoscopy 2013 1(2):41010.1016/S2212-0971(13)70183-3 [Google Scholar] [CrossRef]
[6]. Marks MM, Atkinson KG, Heterotopic bone in a juvenile rectal polypDiseases of the Colon & Rectum 1964 7(5):345-47.10.1007/BF0261683814176152 [Google Scholar] [CrossRef] [PubMed]
[7]. Ahmed R, Ahmad Z, Qureshi A, Osseous metaplasia in a juvenile retention polyp: a case reportBMJ Case Reports 2009 2009:pii bcr032009165010.1136/bcr.03.2009.165021686978 [Google Scholar] [CrossRef] [PubMed]
[8]. Garg M, Kaur J, Bindroo S, Sharma A, Mahajan NC, Metaplastic ossification in a juvenile rectal polyp: a rare histological findingJ Clin Diagn Res 2013 7(5):90810.7860/JCDR/2013/5403.297223814740 [Google Scholar] [CrossRef] [PubMed]
[9]. Bhattacharya N, Sarkar T, Osseous metaplasia in a juvenile polyp: a rare case report in IndiaJ Clin Diagn Res 2013 7(9):200410.7860/JCDR/2013/5789.338524179923 [Google Scholar] [CrossRef] [PubMed]
[10]. Haynes HR, Wiskin AE, Basude D, Gradhand E, Osseous Metaplasia in a juvenile rectal polypJournal of Pediatric Gastroenterology and Nutrition 2017 :2810.1097/MPG.000000000000153728141681 [Google Scholar] [CrossRef] [PubMed]
[11]. Bhat V, Roopa A, Shariff S, Juvenile rectal polyp with osseous metaplasia-a rare case with review of literatureInt J Health Sci Res 2012 2(8):114-16. [Google Scholar]
[12]. Todd I, Juvenile polypsProc R Soc Med 1963 56:969-70.10.1177/003591576305601110 [Google Scholar] [CrossRef]
[13]. Nerita T, Ohnuma H, Yokoyama S, Peutz-Jeghers syndrome with osseous metaplasia of the intestinal polypsPathology International 1995 45(5):388-92.10.1111/j.1440-1827.1995.tb03473.x7647936 [Google Scholar] [CrossRef] [PubMed]