Coronary artery bypass graft surgery surgery is one of the most commonly performed surgical procedures for patients of CAD. Beating heart CABG preferred over on bypass pump and cardioplegia, as it reduces perioperative morbidity and mortality. Anaesthetic induction techniques for cardiovascular surgery are based on considering haemodynamic stability, amelioration of stress response to intubation and maintain balance between myocardial oxygen demand and supply [1-3]. Tachycardia and hypertension during laryngoscopy and intubation poses problem in many patients of ischaemic heart disease with poor left ventricular function. No single anaesthetic agent is suitable for all patients as all of them have its advantages and disadvantages. Various techniques for induction of anaesthesia with agents such as etomidate, thiopentone, propofol, ketamine and midazolam have been used [4-6]. Various studies have shown the stable cardiovascular profile of etomidate, midazolam, thiopentone and propofol in patients with good ventricular function [7-10].
Etomidate is a carboxylated imidazole containing compound that is chemically unrelated to any other drug used for the intravenous induction of anaesthesia [11,12]. It acts on GABA receptor to produce hypnosis. Its haemodynamic stability may be due to its unique lack of effect on the sympathetic nervous system. It may causes short term reversible adrenocortical suppression by dose dependent inhibition [13,14]. Midazolam is a water soluble benzodiazepine with an imidazole ring in its structure that accounts for stability in aqueous solutions and rapid metabolism [15]. Its amnestic effects are more potent than its sedative effects. Fentanyl is a potent, synthetic opioid analgesic with a rapid onset and short duration of action. It is a strong agonist at the μ-opioid receptors. Intravenous fentanyl is often used for anaesthesia, analgesia and for sedation in combination with a benzodiazepine such as midazolam. Therefore, we aimed to compare the effects of etomidate with midazolam and fentanyl as inducing agents in patients undergoing off-pump CABG surgery.
Materials and Methods
This prospective study was carried out at cardiothoracic and vascular surgery department, KGMU Lucknow, between March 2014, August 2015. After getting approval from Institutional Ethical Committee of the medical university, a written and informed consent was obtained from all patients before enrolling them for study.
Total 60 patients with 40 to 80 year age and ASA grading I to IV were included in this study. Patient with SBP <90 and >200 mmHg, heart rate <45 and >130 beats/minutes and ejection fraction <45% were excluded from study. Patients were divided in two groups (n=30 each) by using a computer generated random number table. Group I patients received etomidate 0.5 mg/kg intravenously and Group II patients received midazolam 0.1 mg/kg+fentanyl 5 μg/kg slow intravenously.
Sample size was calculated on the basis of 80% power of study.
n=Z2pq/d2
n=desired sample size
Z=standard normal deviate; usually set at 1.96 (or a~2), which correspond to 95% confidence level.
p=proportion in the target population estimated to have a particular characteristics. If there is no reasonable estimate, use 50% (i.e 0.5)
q=1-p (proportion in the target population not having the particular characteristics)
d=degree of accuracy required, usually set at 0.05 level (occasionally at 2.0)
All patients were given morphine 0.2 mg/kg intramuscularly 30 minutes before entering operation theatre. The blood pressure was recorded by left radial artery cannulation under local anaesthesia in preoperative room. The laryngoscopy and intubation was facilitated with rocuronium bromide 0.9 mg/kg and anaesthesia was maintained with O2 and N2O in 1:2 ratio with isoflurane 0.6%.
Haemodynamic parameters such as heart rate, blood pressure, pulse oximeter and electrocardiogram were monitored continuously, and recorded at baseline, during induction, during intubation and thereafter at intervals of 1, 3, 5 and 10 minutes. In Group I after 10 minutes of induction, injection fentanyl 5 μg/kg was given to provide analgesia for sternotomy and surgical procedure. In both the group after 10 minutes anaesthesia was maintain with O2 and N2O in 1:2, isoflurane 0.6%, fentanyl and rocuronium bromide intermittently till end of surgery.
N2O is not used by majority of the centres, we used N2O as it is a good aesthetic agent and provide good analgesia, and helps to maintain depth of anaesthesia. Fentanyl and isoflurane supply are limited in our institution.
Statistical Analysis
The results are presented in mean±SD and percentage. The chi-square test was used to compare the categorical or dichotomous variables among the groups. The p-value <0.05 was considered significant. All the analysis was carried out by using SPSS 16.0 version.
Results
The demographic profile such as age and gender of the patients in both groups were not significantly different as shown in [Table/Fig-1].
Demographic profile of patients.
| Characteristic | Group I(n=30) | Group-II(n=30) | p-value |
|---|
| Age (mean±SD) years | 56.17±8.98 | 58.30±6.72 | 0.302 |
| Gender Female | 6 (20.0%) | 3 (10.0%) | 0.278 |
| Male | 24 (80.0%) | 27 (90.0%) |
Notes: Pes of implant
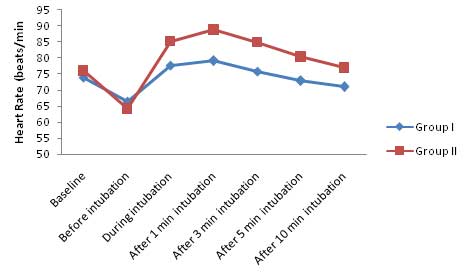
Baseline heart rate was not statistically significant in between Group I (73.93±5.67 beats/minutes) and Group II (75.97±7.31 beats/minutes). The heart rate was also similar in both group after induction till intubation, however it was found to be significantly lower in Group I as compared to Group II for rest of the study period [Table/Fig-2].
Heart rate (beats/minutes).
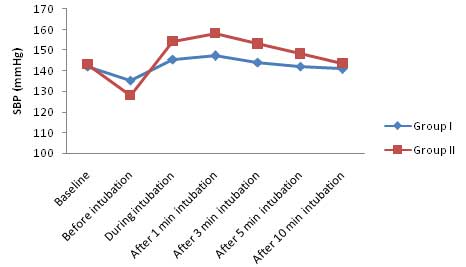
At baseline SBP was not significantly different in between Group I (142.07±8.11) and Group II (143.20±10.22). Before intubation, mean SBP was significantly higher in Group I as compared to Group II. Moreover, the SBP were significantly different in between Group I and Group II at all the other time intervals (p<0.001) except 10 minutes after intubation (p=0.265) as shown in [Table/Fig-3].
Systolic blood pressure (mmHg).
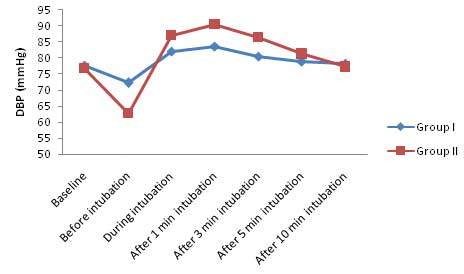
At baseline the DBP was not significantly different between Group I (77.73±6.92) and Group II (76.80±6.55). After induction but before intubation, DBP was significantly lower (<0.001) in Group II as compared to Group I. During intubation, at 1 minute, and 3 minute interval, DBP in Group II was significantly (<0.001) higher as compared to Group I until 5 minutes where (p=0.140) as shown in [Table/Fig-4].
Diastolic blood pressure (mmHg).
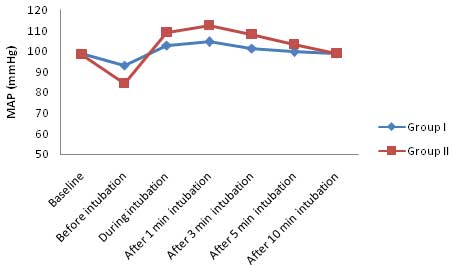
At baseline the Mean Arterial Pressure (MAP) was not significantly different between Group I (98.80±6.71) and Group II (98.50±7.17). Before intubation, the MAP was significantly lower (p<0.001) in Group II as compared to Group I. Moreover at all other time intervals, the MAP was significantly lower (p<0.05) in Group I as compared to Group II until 10 minutes after intubation (p=0.905) as shown in [Table/Fig-5].
Mean arterial pressure (mmHg).
Rate Pressure Product (RPP) at baseline was non significant between Group I and Group II (p=0.233). The RPP was significantly higher in Group I as compared to baseline during intubation, one minutes and after three minutes intubation and it was significantly lower as compared to baseline at rest of the time intervals. In Group II, the RPP before intubation lower by 24.4% as compared to baseline. At all other interval it was higher than Group I, the increase was maximum 1 minutes after intubation (28.6%), At all the follow up intervals change was significant statistically (p<0.05) as shown in [Table/Fig-6].
Evaluation of RPP in two groups at different time intervals
| Time interval | Group I Mean±SD | Group II Mean±SD | p-value |
|---|
| Baseline | 105.02±10.29 | 109.29±16.41 | 0.233 |
| Before intubation | 89.87±9.58 | 82.60±15.16 | 0.030 |
| During intubation | 112.72±9.19 | 131.73±15.67 | <0.001 |
| 1 minutes after intubation | 116.33±9.59 | 140.50±14.44 | <0.001 |
| 3 minutes after intubation | 109.10±9.26 | 130.39±15.69 | <0.001 |
| 5 min after intubation | 103.42±7.82 | 119.49±16.75 | <0.001 |
| 10 minutes after intubation | 99.99±8.19 | 110.85±16.31 | 0.002 |
Discussion
Induction of general anaesthesia in patients with compromised left ventricular function for CABG is a challenge to anaesthesiologist to maintain haemodynamic and minimal instability. There is paucity of literature regarding the choice of suitable agent. Fall in arterial pressure in patients of poor left ventricular function after induction of anaesthesia is mainly due to depression of sympathetic activity, which can be overcome by choosing an induction agent like etomidate, which lacks effect on the sympathetic nervous system and on the function of the baroreceptor [16,17].
The first report of etomidate was published in 1965 but introduced in clinical practice in 1972. Among all the studies conducted till now etomidate used as an induction agent have shown to have minimal effect on cardiovascular system and histamine release due to which it was considered as induction agent of choice in patients with compromised cardiovascular system. However, the enthusiasm among clinicians tempered in the 1980s by reports that the drug can cause temporary inhibition of cortisol synthesis and myoclonus [10].
In contrast to etomidate, midazolam had modest decrease in arterial blood pressure resulting from decrease in systemic vascular resistance. Midazolam produces a “nitro-glycerine-like” effect by decreasing the filling pressures and increasing cardiac output. Concurrent use of opioid has been shown to produce minimal cardiovascular changes [4].
In this study, the baseline heart rate was similar in both groups. The heart rate was also similar in both group after induction till intubation, but it was found to be significantly higher in midazolam-fentanyl group as compared to etomidate group for rest of the study period. SBP was also similar in between both groups at baseline. Whereas there was significant difference in SBP between etomidate and midazolam-fentanyl group at all the other time intervals except 10 minutes after intubation. The DBP was not significantly different in between both groups at baseline. Before intubation, after intubation and 10 minutes after intubation the mean value of DBP was higher in etomidate group. At all the other time intervals, mean value of DBP was significantly lower in etomidate group as compared to midazolam-fentanyl group. The MAP was not significantly different in between groups. Before intubation, the MAP was significantly lower in midazolam-fentanyl group. Moreover at all other time intervals (except 10 minutes after intubation), the MAP was significantly lower in etomidate group. Our results shows that the haemodynamic parameters (SBP, DP and MAP) shows less instability and early recovery with etomidate in comparison to midazolam-fentanyl. Our results are supported by similar findings of previous studies by Shivanna S et al., [11], who found that the etomidate showed less reduction in contractility, after load, preload as compared to propofol. The haemodynamic response in CABG surgery comparing etomidate and ketamine-thiopentone had shown no statistically significant difference between the two, and both the groups were equally good for being used as induction agent [12]. There was no significant change in systolic, diastolic and MAP in group induced with etomidate while in other groups (thiopentone and propofol) were shows significant change in haemodynamic parameter [18]. The haemodynamic parameters and serum cortisol levels in patients undergoing CABG surgery, and found there were significant reduction in blood pressures in propofol group as compared to etomidate group, though there was no significant difference in serum cortisol levels between groups at 24 hours after induction, although the values were close to double the baseline levels [13]. Other study reported that the heart rate and blood pressure both increased remarkably (40%-60%) post-tracheal intubation in midazolam group, the heart rate and blood pressure increased 40%-60%, and then fell back slowly [14]. Etomidate effectively alleviated the cardiovascular responses to tracheal intubation, meanwhile the blood pressure, heart rate were stable at pre and post-tracheal intubation. Systolic and DBP of midazolam group was much lower than those of etomidate group after anaesthetic induction and blood pressure of midazolam group were much higher than those of etomidate group at one minute post-tracheal intubation.
In the present study we observed that the RPP reflects the variation or fluctuation in SBP and heart rate. It was significantly higher in etomidate group before intubation but at all other intervals it was higher in midazolam group and difference was statistically significant. The variation in etomidate group ranged from 10.8%-14.4% while in midazolam group from 24.4%-28.6%. We did not find any significant side effects of etomidate, midazolam or fentanyl during whole study. There was no significant difference in vasopressor requirement in postoperative period in both groups. Urine output was almost normal in both groups. When etomidate used as anaesthetic agent for induction, patients well tolerated the stimulus of tracheal intubation as shown by stable blood flow dynamics. It produces minimal blood pressure and heart rate changes, and resistance of peripheral and coronary vessels decreases is not significant. Thus, its use has been advocated in patients with compromised heart. When used for tracheal intubation, etomidate alone could not prevent the cardiovascular responses, as it does not block sympathetic response to laryngoscopy and intubation, these are often blunted by premedication or co-induction with opioids. Midazolam for anaesthetic induction could cause a decrease in blood pressure by reducing vascular resistance [17], although it had some advantages like sedation, hypnosis, anxiolysis and amnesia. When used as anaesthetic induction agent midazolam-fentanyl drug combination did not effectively alleviate cardiovascular response to tracheal intubation and fluctuation in haemodynamics is very high.
Conclusion
From our study we can conclude that considering haemodynamic effects for patients with CAD etomidate as a drug choice for induction of anaesthesia compared to midazolam-fentanyl.
Notes: Pes of implant