Perforated Jejunal Diverticulitis: An Uncommon Cause of Abdominal Pain
Vimalkumar Dhaduk1, Juneed Mohmed Lanker2, Nadeem Mushtaque Ahmed3, Priyanka Tiwari4, Prasanna Kumar Reddy5
1 Registrar, Department of SGE and Minimal Access Surgery, Apollo Hospital, Chennai, Tamil Nadu, India.
2 Registrar, Department of SGE and Minimal Access Surgery, Apollo Hospital, Chennai, Tamil Nadu, India.
3 Registrar, Department of SGE and Minimal Access Surgery, Apollo Hospital, Chennai, Tamil Nadu, India.
4 Registrar, Department of SGE and Minimal Access Surgery, Apollo Hospital, Chennai, Tamil Nadu, India.
5 Consultant and Head, Department of SGE and Minimal Access Surgery, Apollo Hospital, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Juneed Mohmed Lanker, Registrar, Department of SGE and Minimal Access Surgery, Apollo Hospital, Chamber 5 A, Chennai-600006, Tamil Nadu, India.
E-mail: drjuneed48@yahoo.co.in
Diverticular disease of the jejunum is a rare entity. Most patients with small bowel diverticula are asymptomatic. Patients who develop symptoms generally report symptoms that reflect associated complications. The most common are non specific epigastric pain or flatulent dyspepsia, mainly postprandial. Complications including haemorrhage, intestinal obstruction, diverticulitis and perforation may be life threatening and warrants early surgical intervention. We report a case of a 68-year-old male admitted with jejunal diverticulosis complicated by sealed off perforation and phlegmon formation who has been admitted and treated for abdominal pain previously with different diagnosis in two occasions, once with a diagnosis of symptomatic cholelithiasis and second time with mild pancreatitis which could be the manifestation of jejunal diverticulitis. On admission CT abdomen confirmed the diagnosis of diverticulitis and he underwent laparoscopic assisted resection of involved segment of jejunum and jejuno-jejunal anastomosis. On one year follow-up patient was pain free and symptom free throughout the period. The purpose of presenting this case is to evaluate a presentation of diverticulitis which can delay the diagnosis and contribute to diagnostic dilemma.
Abscess, Diverticulosis, Enterectomy, Jejunal phlegmon, Peritonitis
Case Report
A 68-year-old male presented with a complaint of severe epigastric pain for seven days, not related to food intake, nausea, vomiting, jaundice or diarrhoea. He had similar albeit mild complaints occasionally during the past year for which he underwent laparoscopic cholecystectomy one year back and was admitted with a diagnosis of acute mild pancreatitis eight months back.
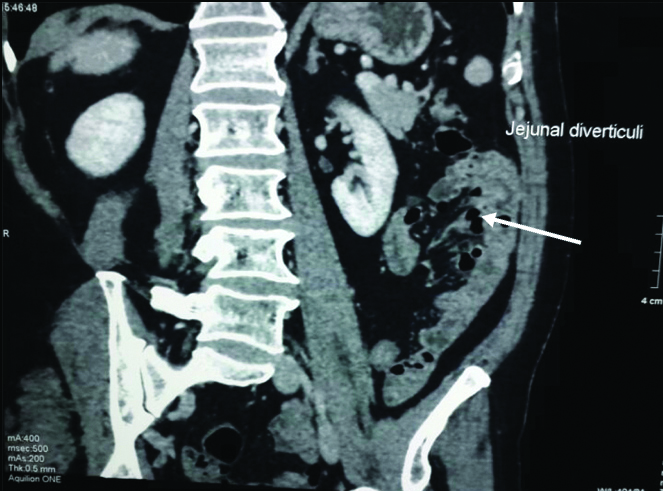
Physical examination revealed tenderness in epigastrium and umbilical region without any sign of peritonitis while other vital parameters were within a normal limit. Laboratory findings (CBC, LFT, KFT, amylase and lipase) were within normal limits. Ultrasonography was apparently normal. CECT abdomen showed jejunal diverticulitis with surrounding haziness and fat stranding along with small mass formation by surrounding omentum and jejunal loops with multiple jejunal diverticuli [Table/Fig-1,2 and 3].
An arrow shows multiple extraluminal air pockets-Diverticuli.
Formation of mass with jejunal loop and surrounding omentum and abdominal wall.

Jejunal loop diverticulitis with surrounding haziness and fat stranding.

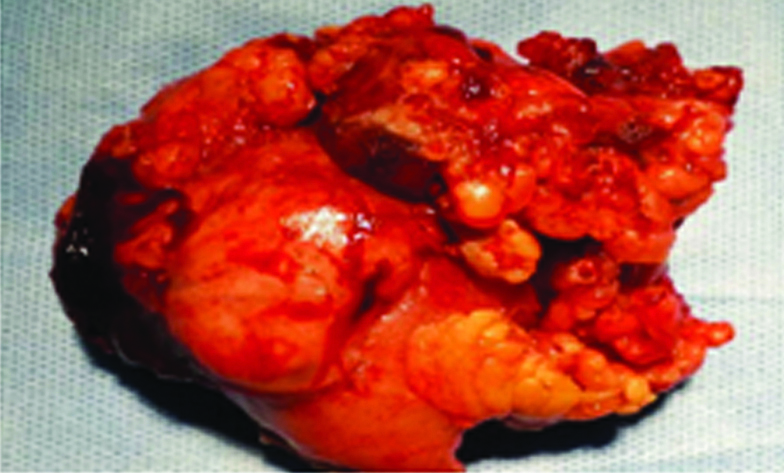
The patient was subjected to diagnostic laparoscopy. About 30 cm from the DJ flexure there was a small jejunal mass of size of 5×4 cm, adherent to the abdominal wall on the left side with dilated proximal bowel. This was released and was exteriorised through a 5 cm infra umbilical incision. It was consistent with jejunal diverticulitis with sealed off perforation. About 7 cm of bowel was resected and functional end to end stapled anastomosis was done, after releasing the adjacent bowel loop which was densely adherent to the mass [Table/Fig-4]. Patient was discharged on 4th postoperative day. Pathology report described intestinal wall with a marked adventitial subacute inflammation with an abscess formation, composed of nodular aggregates of neutrophils and histiocytes surrounded by marked fibroblastic reaction. Mucosal diverticulae extended through muscularis propria into the adventitia focally. Patient was followed up after one year and he was asymptomatic completely throughout the period.
Segment of jejunal loop of 7 cm forming mass with adhesions and exudates.
Discussion
Unlike colonic diverticula, jejunal diverticula are an uncommon and acquired condition which is found in 0.06-4.6% in autopsy [1]. Cooper A in 1807 first reported jejunal diverticulosis [2]. Jejunal diverticula are pseudo diverticula usually occur in proximal jejunum in multiple numbers. Exact mechanism is unknown but, possible mechanism is increased luminal pressure with jejunal muscular wall atrophy. Jejunal diverticula is asymptomatic but, can present more acutely up to four times more often than duodenal or colonic diverticula [3,4]. Patient may present with bleeding, abdominal pain and diarrhoea. Complications include abscess formation, perforation, mass or phlegmon formation and intestinal obstruction [5,6], occurs in 6-10% patients [7].
Diagnosis of jejunal diverticula is often incidental finding on contrast study or intraoperatively. Because of its rarity and non specific symptoms acute jejunal diverticulitis is rarely considered in the clinical differential diagnosis which make it difficult to diagnose and possibly delay the diagnosis and when therapy is delayed, further complications can have serious consequences [8]. Barium follow-through and enteroclysis can be use for diagnosis. A CT scan of the abdomen is useful to identify diverticulitis and abscess formation following diverticular perforation. Indirect sign of diverticulitis in CT are wall thickness, entrapped air or fat tissue inhibition [9]. Diagnostic laparoscopy is a good tool to evaluate intra-abdominal condition and may help to reach a precise diagnosis and curative dissection if requires. In case of jejunal diverticulitis treatment is predominantly surgical; however, in case of locally or self-limiting inflammation and without perforation conservative management is a possible option [10]. It has been found that surgical management is required in approximately 8.5% of patients with jejunal diverticula [11]. Surgical management was first described by Gordinier HC and Sampson JA in 1906 [12]. Treatment of jejunal diverticulitis usually consists of resection of the abnormal segment with primary end to end anastomosis [13]. Although rarely reported in the literature, the laparoscopically assisted resection seems to be safe and feasible [14]. Novak JS et al., has described non surgical management with percutaneous drainage for patient with diverticulitis with localised peritonitis [15]. Walter BM et al., in his case series treated one of the patient with diverticulitis without perforation by laparotomy and resection of jejunum containing diverticulitis who initially failed to improve on conservative management [16] whereas like in present case, Jerraya H et al., preferred laparoscopic management for jejunal diverticulitis [13] in a patient presented with acute abdominal pain and CT showed focal area of asymmetric jejunal wall thickening with oedema without any features of perforation. CECT abdomen and diagnostic laparoscopy is better tool for early diagnosis [17] and treatment of underlying cause in a case of diagnostic dilemma.
Conclusion
Jejunal diverticula is usually a silent disease and presents with variety of symptoms which can mimic symptoms of other diseases, so for clinician to reach the diagnosis is difficult. It is important for clinician to have heightened awareness of jejunal diverticulitis because if it is not recognised promptly in symptomatic patient then complication can occur which can be more morbid and even lead to mortality.
[1]. Makris K, Tsiotos GG, Stafyla V, Sakorafas GH, Small intestinal nonmeckelian diverticulosisJournal of Clinical Gastroenterology 2009 43(3):201-07.10.1097/MCG.0b013e318191926119142169 [Google Scholar] [CrossRef] [PubMed]
[2]. Cooper A, On hernias. Part II. The Anatomy and Surgical Treatment of Crural and Umbilical Hernias 1807 LondonLongmans, Green & Company:90 [Google Scholar]
[3]. Lempinen M, Salmela K, Kemppainen E, Jejunal diverticulosis: a potentially dangerous entityScandinavian Journal of Gastroenterology 2004 39(9):905-09.10.1080/0036552041000628815513392 [Google Scholar] [CrossRef] [PubMed]
[4]. Moris D, Vernadakis S, Jejunal diverticulosis as the obscure cause of acute abdominal painSurgery 2014 155(6):1093-94.10.1016/j.surg.2012.12.00723452878 [Google Scholar] [CrossRef] [PubMed]
[5]. Wilcox RD, Shatney CH, Surgical implications of jejunal diverticulaSouthern Medical Journal 1988 81(11):1386-91.10.1097/00007611-198811000-000133142056 [Google Scholar] [CrossRef] [PubMed]
[6]. Krishnamurthy S, Kelly MM, Rohrmann CA, Schuffler MD, Jejunal diverticulosis. A heterogenous disorder caused by a variety of abnormalities of smooth muscle or myenteric plexusGastroenterology 1983 85(3):538-47.10.1016/0016-5085(83)90005-7 [Google Scholar] [CrossRef]
[7]. Shanmugam RP, Shivakumar P, A rare complication of jejunal diverticulosisTrop Gastroenterol 2005 27(3):134-35. [Google Scholar]
[8]. Schloericke E, Zimmermann MS, Hoffmann M, Kleemann M, Laubert T, Bruch HP, Complicated jejunal diverticulitis: a challenging diagnosis and difficult therapySaudi J Gastroenterol 2012 18(2):12210.4103/1319-3767.9381622421718 [Google Scholar] [CrossRef] [PubMed]
[9]. Macari M, Faust M, Liang H, Pachter HL, CT of jejunal diverticulitis: Imaging findings, differential diagnosis, and clinical managementClin Radiol 2007 62:73-77.10.1016/j.crad.2006.09.01417145267 [Google Scholar] [CrossRef] [PubMed]
[10]. Veen M, Hornstra BJ, Clemens CH, Stigter H, Vree R, Small bowel diverticulitis as a cause of acute abdomenEuropean Journal of Gastroenterology & Hepatology 2009 21(1):123-25.10.1097/MEG.0b013e328303bfdb19011578 [Google Scholar] [CrossRef] [PubMed]
[11]. Rodriguez HE, Ziauddin MF, Quiros ED, Brown AM, Podbielski FJ, Jejunal diverticulosis and gastrointestinal bleedingJournal of Clinical Gastroenterology 2001 33(5):412-14.10.1097/00004836-200111000-0001411606860 [Google Scholar] [CrossRef] [PubMed]
[12]. Gordinier HC, Sampson JA, Diverticulitis (not Meckel’s) causing intestinal obstructionJAMA 1906 46:1585-90.10.1001/jama.1906.62510480013001c [Google Scholar] [CrossRef]
[13]. Jerraya H, Gouta EL, Safta AB, Dziri C, Jejunal diverticulitis: a challenging diagnosisJ Gastrointest Dig Syst 2015 5(340):2 [Google Scholar]
[14]. Saberski E, Novitsky YW, Laparoscopic diagnosis and management of an acute jejunal diverticulitisSurgical Laparoscopy Endoscopy & Percutaneous Techniques 2012 22(1):e18-20.10.1097/SLE.0b013e31823c9ba622318070 [Google Scholar] [CrossRef] [PubMed]
[15]. Novak JS, Tobias J, Barkin JS, Nonsurgical management of acute jejunal diverticulitis: a reviewAm J Gastroenterol 1997 92(10):1929-31. [Google Scholar]
[16]. Walter BM, Winker J, Wagner M, Jung A, Strebel H, Born P, Complicated jejunal diverticulosis-a rare but important diagnosis to consider in abdominal pain: a report of three casesZ Gastroenterol 2016 220(06):562-65.10.1055/s-0042-10529827284931 [Google Scholar] [CrossRef] [PubMed]
[17]. Koger KE, Shatney CH, Dirbas FM, McClenathan JH, Perforated jejunal diverticulaAm Surg 1996 62:26-29. [Google Scholar]