The complex anatomy of elbow joint, displaced multiple fragments and intra-articular extension of fracture make these cases challenging to treat and carry a high complication rate. Early attempts at open reduction and internal fixation of these difficult fractures fell into disrepute because of inability to obtain a stable fixation which led to prolonged postoperative immobilisation [2].
The only reliable method for restoring the normal alignment and contour of the distal humerus is operative exposure and direct manipulation of the fracture fragments and internal fixation using screws and plates. Biomechanical comparison revealed no significant difference between locking compression plate and conventional reconstruction plate in the experimental study by Korner J et al., [3].
Only few studies have specifically addressed the results of fixation with AO reconstruction plates and one third tubular plates [4]. The present study was conducted to evaluate the results of these implants in operative management of distal humerus fractures as these plates are cheaper but with equivalent results.
Materials and Methods
A prospective study was conducted from March 2012 to June 2013, including 20 patients. The study was approved by Institutional Ethics Committee and written informed consent was obtained from all patients.
All fractures of distal humerus with intra-articular extension and fracture dislocation up to 3-week-old were included in the present study. We excluded the patients with pathological fractures, patients with previous non-functional elbow, and patients with significant neurovascular deficit in the affected limb, Type IIIB and IIIC open fractures, patients with recent or current joint infection. The patients were subjected to detailed history including mode of trauma.
Thorough clinical examination was carried out for any associated injuries and medical problems. After routine investigations, standard Antero-Posterior (AP) and lateral radiographs of elbow were taken. The CT scan of elbow with 3D reconstruction was done in those cases where radiographs did not give full information regarding articular fragments. Fractures were classified as per AO classification system of fractures of humerus distal segment. Open fractures were graded as per Gustilo RB and Anderson JT classification [5].
After pre-anaesthetic checkup and fitness, the patients were planned for surgery with preoperative planning for fixation for each individual patient. All patients were operated in lateral decubitus position with the injured limb freely mobile over a roll, in flexion. Tourniquet was applied as proximally on the arm as and when required. Posterior midline skin incision curving laterally at the olecranon area and ending in midline was used. The ulnar nerve was identified and retracted immediately away from operative site. The anconeus was elevated from the olecranon. Non-articular area of the olecranon identified usually 2 cm from the apex of olecranon by distracting the joint. A chevron osteotomy was then performed with a thin saw blade upto the anterior cortex. The osteotomy was completed using a thin osteotome. The fracture was exposed by stripping of triceps from the metaphyses as and when required and reduced to anatomic position, paying special attention to the articular surface. Tourniquet was routinely deflated 60 to 90 minutes later to decrease the risk of complications. Provisional fixation was done with K-wires. Inter fragmentary compression was given with 4.0 mm cancellous lag screw and then definitive fixation was done as per preoperative planning/modification using 3.5 mm AO reconstruction plates and one-third tubular plates. Stability of fixation was checked by gently moving the elbow joint through the complete range of motion.
Olecranon osteotomy was fixed with 2.0 mm K-wires and tension band wiring. The incision was closed in layers over a negative suction drain. Postoperatively the patients were given an above elbow POP back slab. Negative suction drain was removed after 24-48 hours as per drainage. As soon as the patient was pain free, physiotherapy was started in the form of guarded active movements of the elbow. POP back slab was completely discarded by the time of stitch removal or earlier depending upon the per-operative assessment of stability of fixation so as to permit free active and assisted extension and flexion.
The patients were reviewed clinically and radiologically initially after two weeks and subsequently at every three weeks interval with minimum follow-up of six months to evaluate the progress of union, physiotherapy and complications. At final follow-up, all the patients were evaluated for clinical and radiological evidence of union and functional outcome. The final evaluation was done using MEPIS as shown in [Table/Fig-1] [6].
Mayo elbow performance index score.
| Function/Definition | Points | Definition | Points |
|---|
| Pain | 45 | None | 45 |
| Mild | 30 |
| Moderate | 15 |
| Severe | 0 |
| Motion | 20 | Arc>100 | 20 |
| Arc=50-100 | 15 |
| Arc<50 | 05 |
| Stability | 10 | Stable | 10 |
| Moderately unstable | 05 |
| Grossly unstable | 0 |
| Function | 25 | Able to comb hair | 05 |
| Able to feed oneself | 05 |
| Able to perform personal hygiene | 05 |
| Able to put on shirt | 05 |
| Able to put on shoes | 05 |
Results were categorised as ‘Excellent’ for MEPS between 90-100 points, ‘Good’ for MEPS between 75-89 points, ‘Fair’ for MEPS between 60-74 points and poor if MEPS <60.
Statistical Analysis
Descriptive statistics was analysed with SPSS version 17.0 software. Continuous variables were presented as mean+SD. Categorical variables are expressed as frequencies and percentages. The comparison of continuous variables was performed using ANOVA. Nominal categorical data between the groups were compared using chi-squared test. p<0.05 was considered significant.
Results
In present study the age of patients ranged from 17 to 65 years with mean age of 37 years. Most patients (35%) were in age group of 40 to 49 years. There were 16 males and 4 female patients. The mode of injury in majority of patients was fall on the elbow from a standing height. A total of 13 patients reported within first week of injury, four patients reported within 7-14 days and three patients reported between 14-21 days. There was a predominance of left sided hand being affected in 14 (70%) of cases. Four patients (20%) had associated injury.
The fractures were classified according to the AO classification, 2 fractures were classified as Type B and 18 as Type C. Out of these 18 Type C, 10 (50%) were Type C1, 4 (20%) Type C2 and 4 (20%) Type C3 as shown in [Table/Fig-2].
Patients classified based on AO classification.
| Classification of fracture | No. of patient (%) |
|---|
| B1 | 1 (5%) |
| B2 | 0 |
| B3 | 1 (5%) |
| C1 | 10 (50%) |
| C2 | 4 (20%) |
| C3 | 4 (20%) |
There were 18 closed injuries and out of 2 open fractures one was Type I and other was Type II according to Gustilo RB and Andersons JT classification [5].
The average duration between injury and surgery was 12.7 days, with a range of 7-23 days. Most of the cases were operated upon within 10 days of injury.
All the patients were operated in lateral decubitus position posterior midline incision curving laterally at the olecranon area was used. In all 20 patients intra articular chevaron osteotomy was done to expose the fracture. Osteotomy was fixed with K-wires and tension band wirers with K-wires engaging the anterior cortex of ulna. Other approaches which may be used for exposing the fracture include Triceps Reflecting Anconeus Pedicle (TRAP) approach or triceps tongue approach (Campbell’s).
In 17 patients, two plates were used after contouring intraoperatively. In 14 patients one plate was used postero-laterally and another plate was used to buttress the medial column in a 90-90 configuration. In three patients both plates were placed posteriorly. In another three patients single plate was used to stabilise the fracture. In none of the patients parallel plating was used. All the plates used posteriorly were 3.5 mm reconstruction plates and plates used for medial buttressing were both reconstruction plates and one third tubular plates. The preoperative, operative, postoperative images and the movements at elbow joint are shown in [Table/Fig-3,4 and 5].
Images 1a & 1b show preoperative x-rays of elbow, AP and Lateral views. 1c and 1d show intra-operative images and fracture after fixation. Images 1e and 1f show immediate postoperative AP and Lateral views of x-rays. 1g and1h x-rays show fracture union at follow up. Patient pictures from 1i-l show elbow movements in flexion, extension, supination and pronation at six months follow up.

Images 2a & 2b show preoperative x-rays of elbow, AP and Lateral views. 2c and 2d show intra-operative images and fracture after fixation. Images 2e and 2f show immediate postoperative AP and Lateral views of x-rays. 2g and 2h x-rays show fracture union at follow up. Patient pictures from 2i-l show elbow movements in flexion, extension, supination and pronation at six months follow up.

Images 3a & 3b show preoperative x-rays of elbow, AP and Lateral views. 3c and 3d show intra-operative images and fracture after fixation. Images 3e and 3f show immediate postoperative AP and Lateral views of x-rays. 3g and 3h x-rays show fracture union at follow up. Patient pictures from 3i-l show elbow movements in flexion, extension, supination and pronation at six months follow up.

The average duration is mentioned below in the table for various procedures and union in [Table/Fig-6]. Majority of patients in present study had no pain after six months. Only six patients experienced mild and occasional pain resolving with ibuprofen without any requirement of medication on a regular basis. None of the patients in the present study had moderate or severe pain after six months [Table/Fig-7]. The arc of motion of patients in the current study was 96.7° [Table/Fig-8]. The average MEPIS was found to be 86.0.
Average duration of procedures.
| Procedures | Duration |
|---|
| Average operative time | 2 hours 10 minutes |
| Average hospital stay | 9 days |
| Clinico-radiological consolidation | 11-14th weeks |
| Union of olecranon osteotomy | 11-14th weeks |
The list of complications encountered in the study.
| Complications | No. of Patients (%) |
|---|
| Superficial infection | 2 (10%) |
| Delayed union of osteotomy | 2 (10%) |
| Gun stock deformity | 1 (5%) |
| Ulnar nerve sensory neuropathy | 3 (15%) |
| Heterotopic ossification | 1 (5%) |
| Varus/Valgus instability | 0 |
| Arc of motion | Number of patients | Percentage (%) |
|---|
| >100° | 11 | 55% |
| 50°-100° | 9 | 45% |
| <50° | 0 | 0% |
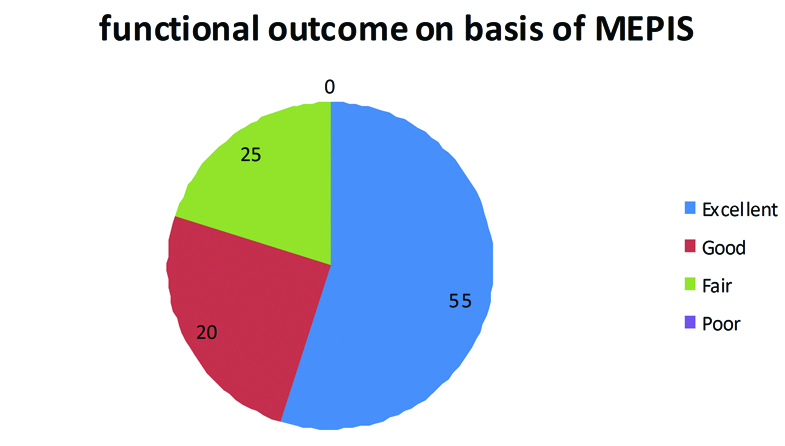
A total of 11 (55%) patients showed excellent results, 4 (20%) good and 5 (25%) fair results. No patient had a poor score in present study as shown in [Table/Fig-9].
Functional outcome based on MEPIS.
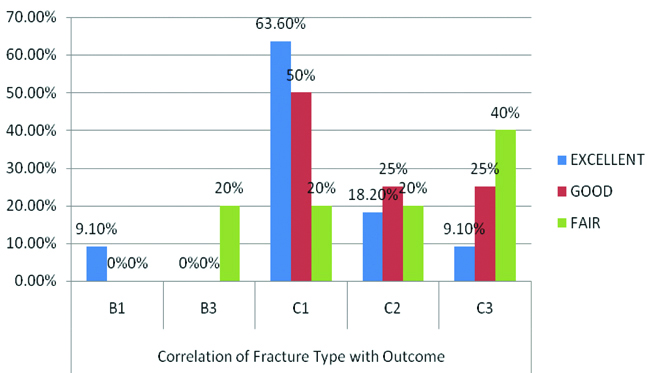
No significant correlation was seen between fracture type and outcome assessed by MEPS (p=0.547). A p-value (0.547) was not significant. A good outcome may be obtained even in Type C3 comminuted fractures [Table/Fig-10]. No significant correlation was seen between the time delay in surgery upto three weeks (p=0.804) and good results may be obtained even for fractures presenting late upto three weeks. The correlation was studied using ANOVA and chi-square test.
The correlation of fracture type with outcome.
Discussion
The past two decades have witnessed significant advancements in surgical techniques and implants to ensure stable osteosynthesis of small intra-articular fracture fragments.
Literature favours management of these fractures by open reduction and internal fixation [7]. Two new implants, the Locking Compression Plate (LCP, Synthes GmbH, Solothurn, Switzerland) and the anatomically preshaped Distal Humeral Plate (DHP, Synthes GmbH, Solothurn, Switzerland) have been introduced to address implant failure.
However, most of the patients in India belong to economically poor or middle class strata. The cost of these locking plate systems is almost four times compared to the simple reconstruction plates used in the present study [8].
Most of the case reports and biomechanical studies available in the literature during the last 10 years show equivalent results of the locking plates compared to the traditional plates for most of the fracture configurations [9].
The purpose of the present study was to investigate the functional outcome and the role of 3.5 mm reconstruction plates and one-third tubular plates for open reduction and internal fixation in fractures of distal humerus in adults.
A number of classification systems have been proposed for the so called “T” or “Y” distal humeral fractures. A much more comprehensive scheme is the recently revised classification of Muller ME et al., and now accepted by the Orthopedic Trauma Association/AO comprehensive classification system of long bones i.e., Type A-non articular, Type B-partial articular, Type C-complete articular [10]. These are further sub-divided based on position of fracture line and degree of comminution. This system is widely used in literature and helps to standardise research protocols and treatment outcomes. It has been used by most of the authors in the literature [11-13].
In the current study, fractures were classified according to the OTA/AO comprehensive classification system. Unfortunately, none of the classification systems accounts for factors such as closeness of the fracture lines from the joint surface or coronal fractures, both of which significantly influence the difficulty of operative management, surgical technique, and patient outcome. One of present study patients had marked intraoperative comminution of the lateral condyle which could be held only by K-wires. In one patient tricortical structural graft was used to reconstruct the gap in capitulum and postero-lateral metaphysis due to impaction at the time of trauma and repeated surgeries. Both these cases in the present study had comparatively less favourable outcome, indicating that this factor should be taken into account while classifying these fractures for defining the prognosis.
All the patients in the present series were operated in the lateral decubitus position with the fore arm hanging by the side over a sand bag placed against the patient’s chest. Lateral decubitus position allowed good visualisation of the fracture fragments by flexing the elbow and made maintenance of reduction easy. This position also poses fewer problems to the anesthetist as compared to the prone position and was also observed to be more comfortable for the assistant.
A midline posterior incision gently curving on the radial side of the olecranon prominence was routinely used. Various series in literature have favoured a dorsal midline incision as it provides extensile approach to the elbow [14]. It preserves more cutaneous nerves than the medial or lateral incision. Scar sensitivity at the olecranon tip can be avoided by slightly skirting the incision away from the olecranon tip. Advantages of dorsal midline approach has also been confirmed by the study of Dowdy PA et al., on standard incisions for approaching joint, where they observed that the number and diameters of cutaneous nerves crossing the posterior incision line decreases the incidence of painful neuroma formation and paraesthesia at the local site [14]. No scar sensitivity was observed in any of the patients in the present study. For exposure of fracture intra articular cheveron shaped osteotomy of the olecranon was used in all the cases in the present study.
Most of the studies in the literature have advocated olecranon osteotomy in comminuted Type C3 fractures citing better visualisation as the reason [15]. However, it does create another fracture with its own concomitant complications such as possible implant irritation, non-union and osteoarthritis. The exposure of articular surface was further improved by acutely flexing the elbow per operatively. During the last two decades, dual plate fixation has become an accepted standard method in the treatment of distal humeral fractures [16].
Dual plate fixation was carried out in 17 of the 20 patients in the study. The reason for using only one plate in the remaining three cases included, a Type B fracture or a long oblique medial condylar fragment which was fixed to the shaft with only inter fragmentary screws and plate was applied laterally to fix the lateral condyle fragment with shaft. Union was seen in all the cases and there were no cases of secondary fracture displacement or implant failure.
In the present study, orthogonal plating in 90-90 configuration was used in 14 patients (70% cases). Majority of authors in the literature have advocated orthogonal placement of plates, which involves placing the medial plate over the medial supracondylar crest and the lateral plate postero-laterally over the dorsal surface, to enable more secure fixation [8]. Several biomechanical studies have proved the orthogonal placement of plates provided rigid stability [17]. The placement of both the plates on the posterior flat surface of humerus which is directly under vision by a posterior approach requires neither extensive dissection nor significant retraction of ulnar nerve, thereby decreasing the incidence of ulnar nerve neuropraxia, heterotopic ossification, delayed union and non-union.
Ozer H et al., in their study treated 11 patients with inter-condylar fracture of humerus with dorsal plating and found stable union in all their patients [18]. Ulnar nerve paraesthesia occurred in two of their patients, which was transient and both patients recovered in four weeks.
In the present study, at least one plate was applied dorsally in 17 of 20 patients and stable union was achieved in all patients at final follow up. Most distal humerus fractures in elderly people are complete intra articular fractures (AO Type C) [19]. Stable fracture fixation is difficult to achieve for complete intra-articular fractures with metaphyseal comminution (AO Type C2 and C3). The most frequent, clinically reported failure occurs by loosening of the bone-implant anchorage at the distal lateral column. The risk of bone implant loosening and failure of osteosynthesis rises with diminished bone quality [7,17].
In the current series, all cases were managed with 3.5 mm conventional AO reconstruction plates and one third tubular plates. The reconstruction plate has several unique characteristics making it suitable for fixing the complex geometry of distal humerus. First, it has notches along the sides of the plate, which enables bending in three dimensions. Second, its hole accepts 4.0 mm cancellous bone screws when the plate is over cancellous bone. Thirdly, screws can be inserted at an angle approximately 25° longitudinally and 7° sideways to allow perfect purchase of bony pillars either in contoured or non-contoured plates [20]. Plates were contoured preoperatively as per the fracture configuration.
No incidence of implant breakage or loosening of screw before fracture union was seen in the current study. Two cases with doubtful stability of the construct, the POP slab was continued for four weeks and the patients were later given a hinged ROM elbow brace when aggressive physiotherapy was started after four weeks.
Early mobilisation of elbow has been universally accepted as a golden rule to ensure an acceptable outcome. In the current study as soon as the patient was pain free, physiotherapy was started in the form of guarded active movement. It is note-worthy that in the present study almost all patients with relatively lesser range of motion at the elbow were either old or those with poor postoperative physiotherapy record. No significant restriction of supination and pronation was observed in any of the patients.
Sardelly M et al., observed that most of the activities of daily living could be accomplished with 100° of elbow flexion in an arc between 30°-130° [21]. The mean arc of flexion in the current study was 96.6°. Most of the patients in the present study were able to accomplish most of the activities of daily living without much difficulty.
The median MEPIS in the current study was 86.0, with most patients reaching either ‘good’ or ‘excellent’ results. The MEPI score is comparable to other studies in literature. Despite the lack of significant difference in functional outcomes when comparing elderly to younger patients, or complex to simpler fractures, there was tendency towards better results in younger patients and patients with fractures other than C3 Type.
A high percentage of acceptable results can probably be attributed to the younger age group in the present series, with a good bone stock and this may have been the reason for a lack of fixation failures and the higher percentage of acceptable results. Beazley JC et al., and Holdsworth BJ and Mossad MM have also indicated that old age is no contraindication for surgical management of these fractures and final outcome is more dependent on the quality of bone rather than the chronological age of the patient [22,23].
The AO reconstruction plates used in the current study had several advantages over other types of plates and found to be very useful and effective in the treatment of this kind of fractures. Early surgical intervention, shorter operative time and early mobilisation of elbow are important parameters for obtaining an excellent outcome. The favourable outcome in this small number of patients does indicate usefulness of this procedure.
Limitation
The present study could not categorically establish the affectivity of these implants in elderly patients with osteoporotic bones and patients with low and severely comminuted fractures where pre-contoured locking plates are preferred.
Conclusion
The present study reinforces the advantage of open reduction and internal fixation in the treatment of adult distal humerus intra-articular fractures. Olecranon osteotomy approach in lateral decubitus position is useful for operation as it gives very good exposure of fracture with visualisation upto anterior trochlea by acutely flexing the elbow.
Use of 3.5 mm AO reconstruction plates and one third tubular plates with the dynamic possibility of contouring the plate per-operatively according to fracture anatomy; give good results with no incidence of implant failure. Good functional outcome with low rate of complications can be obtained even in comminuted fractures and even in patients operated up to three weeks after injury. Routine anterior transposition of ulnar nerve may not be required as the incidence of complications related to it is low.
Fixation of distal intra-articular fractures of humerus in adults with use of AO reconstruction plates and one third tubular plates gives good results in terms of functional outcome because of the dynamic possibility of contouring these plates per-operatively according to fracture anatomy. These plates are cost effective compared to pre contoured locking plates.