A Rare Variant of Germ Cell Ovarian Tumour with Glandular Differentiation and Cutaneous Metastasis
Smriti Agrawal1, Vinita Das2, Anjoo Agarwal3, Amita Pandey4, Namrata Kumar5
1 Associate Professor, Department of Obstetrics and Gynaecology, King George’s Medical University, Lucknow, Uttar Pradesh, India.
2 Professor, Department of Obstetrics and Gynaecology, King George’s Medical University, Lucknow, Uttar Pradesh, India.
3 Professor, Department of Obstetrics and Gynaecology, King George’s Medical University, Lucknow, Uttar Pradesh, India.
4 Professor, Department of Obstetrics and Gynaecology, King George’s Medical University, Lucknow, Uttar Pradesh, India.
5 Assistant Professor, Department of Obstetrics and Gynaecology, King George’s Medical University, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Smriti Agrawal, Associate Professor, Department of Obstetrics and Gynaecology, King George’s Medical University, Lucknow-226003, Uttar Pradesh, India.
E-mail: smritijainagrawal@rediffmail.com
A 35-year-old lady presented with a large ovarian tumour with cutaneous metastasis and tumour markers suggestive of germ cell tumour. Earlier, she underwent laparotomy for suspected chronic ectopic pregnancy of which details were unavailable. Her tissue biopsy from tumour as well as cutaneous deposit showed adenocarcinoma. She was confirmed to have a rare variant of glandular differentiation of germ cell tumour. In view of inoperable masses, Bleomycin Etoposide Cisplatin (BEP) chemotherapy was initiated and tumour along with cutaneous metastasis showed features of regression after two cycles. However, patient died due to complications, following chemotherapy. Glandular differentiation of germ cell tumour must be kept in mind if histopathology shows adenocarcinoma in presence of elevated α Fetoprotein (α-FP), β-HCG, LDH. Cutaneous metastasis in ovarian malignancy carries a poor prognosis.
Adenocarcinoma, Atypical histopathology, Elevated tumour markers
Case Report
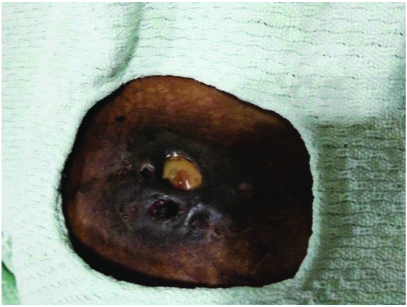
A 35-year-old primipara presented in OPD with a complaint of amenorrhoea and weight loss since two months. On examination, patient was cachexic with no pallor or lymphadenopathy. There was a pelvic mass palpable abdominally upto 16 week size gravid uterus in hypogastric region and both iliac fossae with hard consistency and restricted mobility. There was a cutaneous nodule measuring around 10×8 cm at the incision site and skin over it appeared stretched and erythematous [Table/Fig-1]. On palpation it was tender. She attended a local hospital four months back with history of pain in abdomen but her menstrual periods were regular. Her examination then showed an adnexal mass measuring 80×80 mm mass with firm consistency on right side with normal uterine size. Since her pregnancy test was positive, she was suspected to have chronic ectopic pregnancy and taken for laparotomy outside four months back. Right-sided salpingectomy with right-sided ovarian cyst excision was done. No intraoperative details or histopathology report was available. Around two months subsequently, patient developed a nodule on skin at lateral end of incision line, which gradually increased in size. Fine Needle Aspiration Cytology (FNAC) from cutaneous nodule was done outside which showed adenocarcinoma.
Cutaneous metastasis measuring 10×8 cm at the lateral end of incision line.

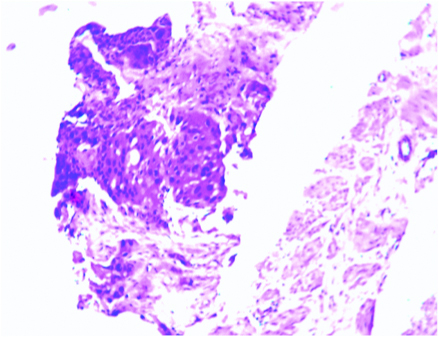
She was admitted in this hospital and evaluated. Clinically the mass seemed to arise from pelvis with restricted mobility. The mass was not resectable clinically. Ultrasonography showed normal sized uterus with bilateral adnexal masses with mixed echogenicity, each measuring around 7×8 cm in size. There was minimal free fluid in pelvis. Her tumour markers done at this stage were LDH: 1530 U/L (<247 U/L), β-HCG >2, 25,000 (<5 mIU/mL), Serum α-FP: 22352 ng/mL (<8.5 ng/mL), Serum CA 125: 21.3 U/L (<35 U/mL), Serum CA 19.9: 87 U/mL (<40 U/mL), Serum CEA: 4.6 ng/mL (<5 ng/mL). Since there was no histopathology from previous surgery, it was decided to do biopsy. FNAC was done from pelvic mass which showed papillaroid sheets of atypical pleomorphic cells on basis of which diagnosis of moderate to poorly differentiated adenocarcinoma was made and cutaneous nodule showed metastatic adenocarcinoma. However, since the tumour markers did not correlate with cytology, the trucut biopsy from the mass was done. Histopathology from cutaneous nodule showed necrotic tissue only and ovarian mass again showed moderate to poorly differentiated adenocarcinoma [Table/Fig-2]. Immunohistochemistry showed Cytokeratin (CK) positive [Table/Fig-3]. Other immunohistochemistry could not be done as the tissue size was very small. She also had bilateral hydronephrosis and deranged renal function, hence bilateral percutaneous nephrostomy was placed to optimise renal function. She was subsequently planned to start neoadjuvant chemotherapy.
Histopathology showed papillaroid sheets of atypical pleomorphic cells suggestive of moderate to poorly differentiated adenocarcinoma. There was no evidence of two cell population i.e., cytrophoblasts and synctitrophoblast (H&E, 10X).
Immunohistochemistry shows CK positive as seen in germ cell tumours (40X).

There was a big dilemma about the choice of chemotherapy in view of poor correlation with tumour markers and histopathology. In view of possibility of glandular differentiation in germ cell tumours, BEP regimen was started after consultation with medical oncologist. She tolerated two cycles well and the abdominal lump along with cutaneous nodule showed features of regression [Table/Fig-4]. However, she developed intractable vomiting with severe hypokalaemia which appeared to be a side effect of chemotherapy than the original disease. Despite corrective measures, she died of electrolyte imbalances.
Cutaneous metastasis measuring 4×3 cm showing features of regression.
Discussion
Germ cell tumours have a direct correlation with elevated tumour markers like α-FP, β-HCG, LDH. In the present case, all the three tumour markers were suggested of germ cell tumour and histopathology showed adenocarcinoma. Hence, glandular differentiation of germ cell tumours was thought and it was decided to start neoadjuvant chemotherapy-BEP regime, as the mass was unresectable.
On reviewing the literature, there is a case series of eight cases of ovarian yolk sac tumours with glandular patterns resembling endometrioid adenocarcinoma by Clement PB et al., [1]. Here the patients ranged in age from 11-34 years and had elevated serum α-FP. The endometrioid-like pattern reflected an unusual form of endodermal differentiation within yolk sac tumors that should be distinguished from endometrioid carcinoma. Strong JW et al., also reported a case of endometrioid like variant of testicular yolk sac tumour diagnosed on FNAC in a young male [2]. So, glandular differentiation of germ cell tumour should be kept in mind when histopathology shows adenocarcinoma in presence of elevated tumour markers.
Cutaneous metastasis in ovarian malignancy is not very common. Most of the cutaneous metastasis are associated with breast cancer, prostate cancer and cancer involving gastrointestinal tract. The present lady developed metastasis on the incision line two months after laparotomy due to possible spread of the tumour while removal. Wiechert AC et al., reported a rare case of cutaneous metastases in recurrent epithelial ovarian cancer in which metastasis were diffuse in inguinal fold with intense pruritis [3]. Port site recurrence is also sometimes seen in laparoscopic management of ovarian malignancy. Incidence varies from <1% to 16% in the literature [4]. Prognosis of patient after diagnosis of cutaneous metastasis is usually poor and the most important prognostic factor is the interval between diagnosis of ovarian tumour and cutaneous involvement [5]. In the present case, cutaneous metastases appeared two months after laparotomy indicating a poor prognosis. Management comprises of local excision, chemotherapy and radiotherapy [6]. Since, the tumour was inoperable, neoadjuvant chemotherapy was initiated. There was regression of tumour along with cutaneous metastasis after two cycles of BEP regime.
Germ cell malignancy can masquerade as ectopic pregnancy due to presence of positive pregnancy test and adnexal mass similar to present case [7]. However, here non availability of operative details or histopathology delayed suspicion and further detection of ovarian malignancy. Subsequently development of cutaneous metastasis worsened the prognosis. Presence of elevated tumour markers like α-FP, β-HCG, and LDH (confirmed twice) with histopathology of adenocarcinoma led to the possibility of glandular differentiation in germ cell tumours.
Conclusion
The present case report is being reported due to its unusual presentation of adnexal mass with cutaneous metastasis with elevated tumour markers suggestive of germ cell malignancy. Diagnosis was challenging as it was a rare variant of glandular differentiation. Glandular differentiation of tumour must be borne in mind when suspected germ cell tumour shows adenocarcinoma on histopathology.
[1]. Clement PB, Young RH, Scully RE, Endometrioid-like variant of ovarian yolk sac tumor. A clinic pathological analysis of eight casesAm J Surg Pathol 1987 11(10):767-78.10.1097/00000478-198710000-000043661822 [Google Scholar] [CrossRef] [PubMed]
[2]. Strong JW, Worsham GF, Baker AS, Hawk JC 3rd, Austin RM, Fine-needle aspiration cytology of an endometrioid-like variant of yolk sac tumorDiag Cytopathol 1992 8(6):600-04.10.1002/dc.28400806131281767 [Google Scholar] [CrossRef] [PubMed]
[3]. Wiechert AC, Garrett LA, Lin G, Goodman A, Management of a skin metastasis in a patient with advanced ovarian cancerGynecologic Oncology Reports 2012 2:124-26.10.1016/j.gynor.2012.07.00324371642 [Google Scholar] [CrossRef] [PubMed]
[4]. Chitrathara K, Khan A, Sreedharan N, Shriya N, Raj S, Vaginal vault metastasis - The new enigma in port site recurrences in gynecological laparoscopic surgeriesGynecology and Minimally Invasive Therapy 2016 5:116-19.10.1016/j.gmit.2015.06.003 [Google Scholar] [CrossRef]
[5]. Cormio G, Capotort M, Di Vagno G, Cazzolla A, Carriero C, Selvaggi L, Skin metastases in ovarian carcinoma: a report of nine cases and a review of the literatureGynecol Oncol 2003 90(3):682-85.10.1016/S0090-8258(03)00400-1 [Google Scholar] [CrossRef]
[6]. Demirci S, Yavas F, Ozsaran Z, Ozsaran A, Dikmen Y, Zekioglu O, Palliative radiotherapy for the skin metastasis of ovarian cancer: a case report and review of the literatureMed Oncol 2010 27(3):628-31.10.1007/s12032-009-9259-z19536657 [Google Scholar] [CrossRef] [PubMed]
[7]. Kucera C, Cox-Bauer C, Miller C, Apparent ectopic pregnancy with unexpected finding of a germ cell tumor: A case reportGynecol Oncol Rep 2017 21:31-33.10.1016/j.gore.2017.05.00428664181 [Google Scholar] [CrossRef] [PubMed]