The burden of thyroid diseases in India is high. There has been an increase in the number of thyroid diseases being diagnosed due to greater awareness, which has also led to a higher number of surgeries being performed for benign disease [1].
With more people recognizing alteration of voice as a complication of thyroid surgery, there is a change in trend in many countries, preferring Otorhinolaryngology surgeons for thyroid surgeries over general surgeons [2,3]. With a global increase in the number of cases, surgeons are bound to give better care, reducing the associated morbidity and mortality to a bare minimum.
Conventionally, RLN is identified by its relationships with inferior thyroid artery, tracheoesophageal groove and ligament of Berry. However, this may not always be accurate due to possible anatomical variations and altered neurovascular relationship due to pathological conditions. Injury to the RLN results in a weak voice or loss of voice and aspiration, and bilateral nerve injury leads to dyspnoea and often life threatening glottal obstruction [4,5]. It has been observed that repeat surgeries, Grave’s disease and surgeries for thyroid malignancy, were more prone to RLN injury [6,7]. Identifying the RLN routinely for all thyroid and parathyroid surgeries is recommended to ensure the nerve integrity [8,9].
Other possible complications are hypocalcaemia (due to parathyroid injury), inability to raise the pitch of voice (superior laryngeal nerve injury), infection, airway compromise and excessive bleeding.
In the present study, we try a novel method of identification of RLN intraoperatively, by spraying methylene blue dye in the tracheoesophageal groove area, after ligation of superior pole and before ligation of inferior pole during dissection of the thyroid. Identification of RLN at this stage will help the surgeon to take adequate measures to preserve the nerve and avoid damage during dissection.
Materials and Methods
This was a prospective, observational study, conducted on 30 patients undergoing various thyroidectomy procedures at Bapuji Hospital and Chigateri General Hospital, teaching hospitals attached to department of otorhinolaryngology, head and neck surgery of JJM Medical College, Davangere, Karnataka, India, during the study period of October 2015 to July 2017.
Patients with a thyroid swelling, in biochemically euthyroid state requiring surgical management, willing for surgery under general anaesthesia, belonging to either gender, in the age group of 18-60 years were included in the study. The exclusion criteria were age more than 60 years and less than 18 years, hyperthyroid or hypothyroid states, patients unfit for general anaesthesia and those who had preoperative unilateral or bilateral vocal cord palsy as observed on indirect laryngoscopic examination.
Institutional Ethical Committee approval and written informed consent was obtained from all cases. Patients were monitored from the time of admission, up till the time of discharge from the hospital and were later followed up during the period of study at interval of 3 months in the OPD. A note was made of the patient demographics, type of thyroidectomy done, histopathological diagnosis and complications, if any.
In each patient, both before and after surgery, indirect laryngoscopic examination was performed to evaluate vocal cord mobility. The presence of clinical symptoms or signs of hypocalcaemia were noted.
Surgical Procedure
After positioning the patient on the operating table, parts were painted with 10% povidone iodine solution and draped. After the standard Kocher incision, total or partial thyroidectomy was performed according to the need. Following the elevation of flaps, lateral thyroid vein ligation and dissection of thyroid lobes were done. The superior pole was ligated and cut. Normally, at this stage, the identification of RLN or the parathyroid is difficult. Before inferior pole ligation, the thyroid lobe was deviated medially and 0.5 mL methylene blue diluted with 5 mL normal saline was sprayed over the thyroid lobe and perilobar area. The major structures in this area include RLN, parathyroids, inferior thyroid artery and veins which were observed post spraying. The surgical specimen was subjected for histopathological examination.
Postoperatively, serum calcium levels were estimated between the second to fifth postoperative days. Hypocalcaemia was defined as a serum calcium level less than 8 mg/dL [10]. A repeat indirect laryngoscopic examination was carried out to assess vocal cord mobility postoperatively.
Results
The study population included 30 patients, (2 male and 28 female patients) with a female:male ratio of 14:1. The mean age of the group was found to be 35.133 years. All 30 patients underwent thyroidectomy for goitrous thyroid enlargement, with euthyroid status.
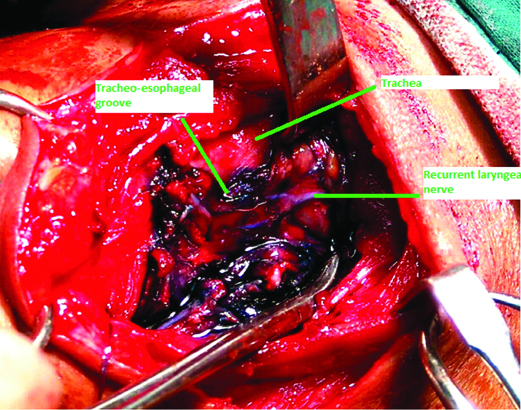
Intraoperatively, RLN could be identified in all the patients, as an unstained structure in the tracheoesophageal groove [Table/Fig-1].
Intraoperative image showing the right tracheoesophageal groove following methylene blue spraying. Right RLN is visible as an unstained structure (labelled as recurrent laryngeal nerve).
Among the 30 patients, 16 patients underwent either right or left hemithyroidectomy (54.34%), 13 patients underwent total thyroidectomy (43.33%) and 1 patient underwent completion thyriodectomy (3.33%) [Table/Fig-2].
Operative procedure done.
| Procedure | Number of cases | Percentage (%) |
|---|
| Hemithyroidectomy | 16 | 53.34 |
| Total thyroidectomy | 13 | 43.33 |
| Completion thyroidectomy | 1 | 3.33 |
| Total | 30 | 100 |
Histopathology revealed 12 cases of colloid goiter (40%), 9 cases of solitary thyroid nodules (30%), 6 cases of multinodular goiters (20%), 2 cases of follicular adenomas (6.67%) and 1 case of follicular neoplasm (3.33%), among the study population [Table/Fig-3].
Histopathological diagnosis.
| Histopathological diagnosis | Number of cases | Percentage (%) |
|---|
| Colloid goiter | 12 | 40 |
| Solitary nodule thyroid | 9 | 30 |
| Multinodular goiter | 6 | 20 |
| Follicular adenoma | 2 | 6.67 |
| Follicular neoplasia | 1 | 3.33 |
| Total | 30 | 100 |
The parathyroid glands washed out the stain within 3 minutes and were visible in the original yellow colour, whereas it took close to 10 minutes for the thyroid tissue to wash out the stain in all cases. The perithyroid muscles, tendons and lipoid structures retained the blue colour for more than 30 minutes. None of the patients had RLN palsy postoperatively.
The examination of vocal cords was done at the time of extubation and using indirect laryngoscopy on postoperative day 1, 1 week, 1 month and 3 months.
None of the 30 patients included in this study developed any other postoperative complication.
Discussion
With superior dissection techniques and expertise in thyroid surgeries, the occurrence of complications has come down, but when they occur, they cause lifelong handicap. The most important complications encountered are injury to the RLN and parathyroids. Among the various factors that result in injury to these structures are extents of resection, reoperation and surgeon factors. Meticulous dissection is a key factor in minimising the development of complications [11-16].
During thyroid surgery, the parathyroid glands and RLN can be protected by careful dissection. Various methods have been tried including capsular dissection, attention to protection of the arterial branches to parathyroids, avoiding unnecessary manipulation in the area of RLN or its blood supply [17].
The important factor in thyroid surgery for benign conditions is the extent of resection, as it was believed that total thyroidectomy leads to a higher chance of injury to RLN or the parathyroids as opposed to partial thyroidectomies [18]. Studies show an incidence of RLN palsy between 0.3 and 1.7%, and that of permanent hypoparathyroidism between 0.7 to 3.0% [12,19-23].
Due to the lifelong implications of RLN injury or parathyroid injury, this area has been studied extensively so as to minimise the risk of these complications.
RLN function can be assessed by several methods like nerve stimulation and finger palpation of cricoarytenoid muscle, direct or fibreoptic laryngoscopy for observation of vocal cords and the use of intramuscular vocal cord electrodes [24].
A multicentre study by Dralle H et al., observes that direct identification of RLN by sight is ideal, and is considered the “gold standard” of care [25].
The technique of using dyes in identification of parathyroid glands and prevention of hypoparathyroidism, was first described by Klopper PJ and Moe RE [26]. Initial studies were conducted using dyes like toluidine blue and tryptan blue, however, these were replaced by methylene blue as their teratogenic effects were discovered [27-29].
In the literature, all the studies related to thyroid surgery and parathyroid staining was performed by injecting the dye via intravenous or intra arterial route. Dudley NE used an intravenous infusion technique on 17 patients and demonstration of one or more parathyroids was possible with this technique [29].
Elias D et al., used the same technique on 59 patients and was able to precisely localise the parathyroid glands in 87% cases [30].
With this technique, only the parathyroid glands can be visualised. This is because of the rich vascularity of the glands. Identification of the RLN is not possible with this method.
In 2012, Sari S et al., studied the effects of methylene blue spraying in identification of RLN and performing safe thyroidectomy [31]. They observed that dye did not stain the RLN and inferior thyroid arteries, while all other tissues stained blue. Further, it was noted that although the parathyroids were stained, they washed out the colour in three minutes and were visible in their original yellow colour.
We obtained similar results in our study also. In all 30 patients, the RLN was visible as an unstained white structure in the blue stained background and could be easily identified.
Riddell VH compared identification and non identification of RLN during thyroidectomies and that study has been the basis of the present day dictum that proper knowledge of anatomy, nerve visualization and experience of the surgeon are the most important tools for protecting the nerve [32].
Guglielmo A et al., mention in their study that the only safe guard against RLN damage, when performing a thyroidectomy, is identifying rather than avoiding the nerve. It has been observed and widely agreed upon that the experience of the surgeon is also an important factor that accounts for the variation in the rate of occurrence of paralysis of vocal cords [33].
Lahey FH reported his experience with deliberate exposure and identification of RLN over 10,000 thyroidectomies. The less than 1% RLN injury rate was significantly lower than any previously published series and lead him to advocate the routine identification and dissection of the nerve during thyroid surgeries [34,35].
Steurer M et al., have concluded from their study that RLN preparation does not increase the overall number (temporary and permanent) of RLN palsies but effectively reduces the number of permanent RLN palsies. Whenever extracapsular thyroid or parathyroid surgery is performed, RLN preparation should be performed [36].
In present study, we have identified the RLN in all 30 cases and have successfully avoided injury in all patients, as confirmed on postoperative indirect laryngoscopic examination.
Limitation
The limitation of present study was the small sample size. There is a need for a study with a larger sample size for strengthening the results.
Conclusion
In present study, we have found that spraying of methylene blue dye (0.5 mL in 5 mL normal saline) in the perithyroidal area after ligation of superior pole helps in fast and easy identification of the RLN as well as the parathyroids glands, along with the thyroid arteries. In addition, it does not require intravenous or intra arterial administration of methylene blue, and thus the potential complications of intravascular dye infusion can be avoided.