Determining the Frequency of Macroamylasemia in Patients with Hyperamylasemia using PEG Precipitation Method
Amir Vahedi1, Bahareh Mehramouz2, Parham Maroufi3, Tannaz Pourlak4, Razak Rezvanpour5, Behrooz Shokouhi6, Tala Pourlak7
1 Associate Professor, Department of Pathology, Tabriz University of Medical Sciences, Tabriz, Iran.
2 Assistant Professor, Liver and Gastrointestinal Disease Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
3 Assistant Professor, Department of Orthopedic, Tabriz University of Medical Sciences, Tabriz, Iran.
4 Assistant Professor, Connective Tissue Diseases Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
5 Resident, Department of Pathology, Tabriz University of Medical Sciences, Tabriz, Iran.
6 Associate Professor, Department of Pathology, Tabriz University of Medical Sciences, Tabriz, Iran.
7 Assistant Professor, Connective Tissue Diseases Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Tala Pourlak, Connective Tissue Diseases Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
E-mail: dr.pourlaktala@yahoo.com
Introduction
The term acute abdomen refers to severe and sudden abdominal pain requiring urgent reorganisation. One of the factors causing acute abdomen is acute pancreatitis, which needs immediate measurements. Acute pancreatitis is also associated with increased levels of serum amylase and lipase. Increased serum amylase also appears under other conditions including macroamylasemia and would result in misdiagnosis.
Aim
This study aimed to investigate the frequency of macroamylasemia in hyperamylasemia patients using Polyethylene Glycol (PEG) precipitation method.
Materials and Methods
In this cross-sectional study, 100 patients with high serum amylase who received healthcare services in Tabriz Imam Reza Hospital from 2014 to 2015 were included. Presence of macroamylase was evaluated in patients using PEG sedimentation method. Collected data were analysed using SPSS software version 17 and chi-square test, as well as independent sample t-test were carried out. The significance level was set at <0.05.
Results
Of 100 patients, 63% were male and 37% were female and their mean age was 50.2±0.7 years. The mean level of serum amylase was 740.4±277.567 U/L and the mean level of serum amylase after PEG precipitation was 578±240.05 U/L. No significant correlation was found (p=0.478). In this study, the frequency of macroamylasemia was 4 (4%) and the frequency of real hyperamylasemia was equal to 96 (96%). The mean level of serum amylase after PEG precipitation was higher in real hyperamylasemia patients than in macroamylasemia patients and a significant association was observed in this regard (p<0.001).
Conclusion
The current study showed that a high percentage of hyperamylasemia patients experience macroamylasemia. Regarding the findings and the significance of this issue, it is recommended to consider the diagnosis of macroamylasemia as one of the best approaches to prevent undertaking unnecessary diagnostic procedures and treatments.
Acute abdomen, Acute pancreatitis, Amylase, Cholecystitis, Pancreatitis
Introduction
The term acute abdomen as one of the medical emergencies refers to sudden and severe abdominal pain, requiring immediate diagnosis and action. Many causes of the acute abdomen need surgery. The acute abdomen mostly manifests itself as pain. Some causes of the acute abdomen are as follows: Acute appendicitis, acute cholecystitis, acute pancreatitis, intestinal ischaemia, peptic ulcer, peritonitis and so on [1,2].
Acute pancreatitis is an inflammatory condition of the pancreas and occurs when the pancreatic enzymes, especially trypsin, activates in the intestine instead of the pancreas. Diagnosis of acute pancreatitis can be based on the positivity of following factors: initial clinical signs and diagnostic tests [3].
In the initial stages (within the first 24 hours of acute pancreatitis), serum amylase and lipase levels increase. Increased levels of total serum amylase in acute pancreatitis may be accompanied with other problems like salivary gland diseases including mumps; perforated peptic ulcer, peritonitis, misplaced pregnancy, pancreatic carcinoma, trauma and macroamylasemia [4]. Macroamylasemia is one of the causes of increased serum amylase (hyperamylasemia) levels which is not associated with the pancreas. Macroamylasemia itself is not considered as a disease and requires no treatment. It is more common in men than women due to unknown reasons [4]. Macroamylasemia is a condition where the serum amylase protein links to other serum proteins such as immunoglobulins A and G and forms complex macromolecules of large size [5]. This complex’s excretion by the kidney is slower than serum amylase excretion; therefore, it is accumulated in the blood circulation and its serum levels increase. As a result, macroamylasemia can cause diagnostic problems in hyperamylasemia and acute pancreatitis patients [6]. Distinguishing macroamylasemia and hyperamylasemia in pancreatic diseases such as acute pancreatitis is clinically important and is to prevent unnecessary diagnostic procedures and treatment [5,7]. Also, macroamylasemia in some patients with acute abdomen may be due to non pancreatitis reasons such as acute appendicitis and, if not concerned, misdiagnosis may occur and it is wrongly diagnosed as acute pancreatitis that would be detrimental to the patient [8]. Macroamylasemia in patients with abnormal humoral immunity or patients with possible pancreatitis diagnosis or pancreatitis itself is aggravated and thus, pancreatitis should be abandoned. The conditions should be considered more closely in patients with asymptomatic hyperamylasemia.
Patients with idiopathic hyperamylasemia are even being evaluated by expensive tests such as several blood tests, CT-scan, laparoscopy and laparotomy. In these cases, this may be caused by misdiagnosis of macroamylasemia as hyperamylasemia. Nowadays, the PEG precipitation method is the method of choice for detecting macromolecules including macroamylase. The method is not complicated, provides a quick response and is financially affordable [9]. It takes 10 minutes to detect macroamylasemia using the simple PEG deposition method with no additional costs. This highlights the significance of macroamylasemia for such patients to prevent unnecessary actions [7].
In this study, the patients whose physicians requested a serum amylase test for various reasons and whose serum amylase level was high, the macroamylasemia was checked using the PEG deposition method in order to determine the frequency of macroamylasemia in patients with high serum amylase levels.
Materials and Methods
In this cross-sectional study, 100 patients with high serum amylase levels who were admitted at Tabriz Imam Reza Hospital were evaluated. Patients were randomly selected among all the patients with high serum amylase levels whose physician requested laboratory test for the serum amylase level to be examined. The patients’ macroamylase level was examined using the PEG precipitation method in the Central Laboratory of Imam Reza Hospital. Basic variables consisted of serum amylase level and serum macroamylase level. Other variables were age and gender. The study was carried out for one year (2014-2015).
PEG deposition method is a low cost and effective method, 120 g/L PEG 6000 was used for macroamylase deposition and 0.2 mL of PEG solution was added to 0.2 mL of the patients’ serum and it was incubated at 37°C for 10 minutes. Then, it was centrifuged for three minutes at 3500 rpm. In another tube, 0.2 mL of water was added to 0.2 mL of the patients’ serum. In PEG method, if 73% of amylase compared to water tubes was deposited, macroamylase could be detected; however, there could be only 52% deposition for amylase because of its normal molecular weight [10,11]. Serum free amylase level was determined by subtracting macroamylase concentration from total amylase. The patients were then divided into three groups:
A group of patients who had just macroamylasemia with normal serum free amylase level.
A group of patients who had macroamylasemia with high serum free amylase level (macroamylasemia+real hyperamylasemia).
A group of patients with no macroamylasemia but with high serum free amylase level (real hyperamylasemia).
Statistical Analysis
The number and proportion of patients in each group was determined. For descriptive statistical analysis, frequency, percentage, mean and standard deviation were used. Chi-square test was used for qualitative variables and independent sample t-test was used for quantitative variables. The statistical analyses were performed with the SPSS software version 17 and p-value was set at <0.05 in all analytical tests.
Results
Demographic Findings
In this study, 100 patients with a high serum amylase level were included. The participants’ mean age was 50.2 years and the median was 49.5 years. The calculated mean age was higher in female than male patients. The youngest and oldest patients were 30 and 70-year-old, respectively, [Table/Fig-1] shows the patients’ age distribution. Of 100 patients, 63% (n=63) were male and 37% (n=37) were female.
Participants’ age distribution.

Serum Amylase Level Before and After PEG Test
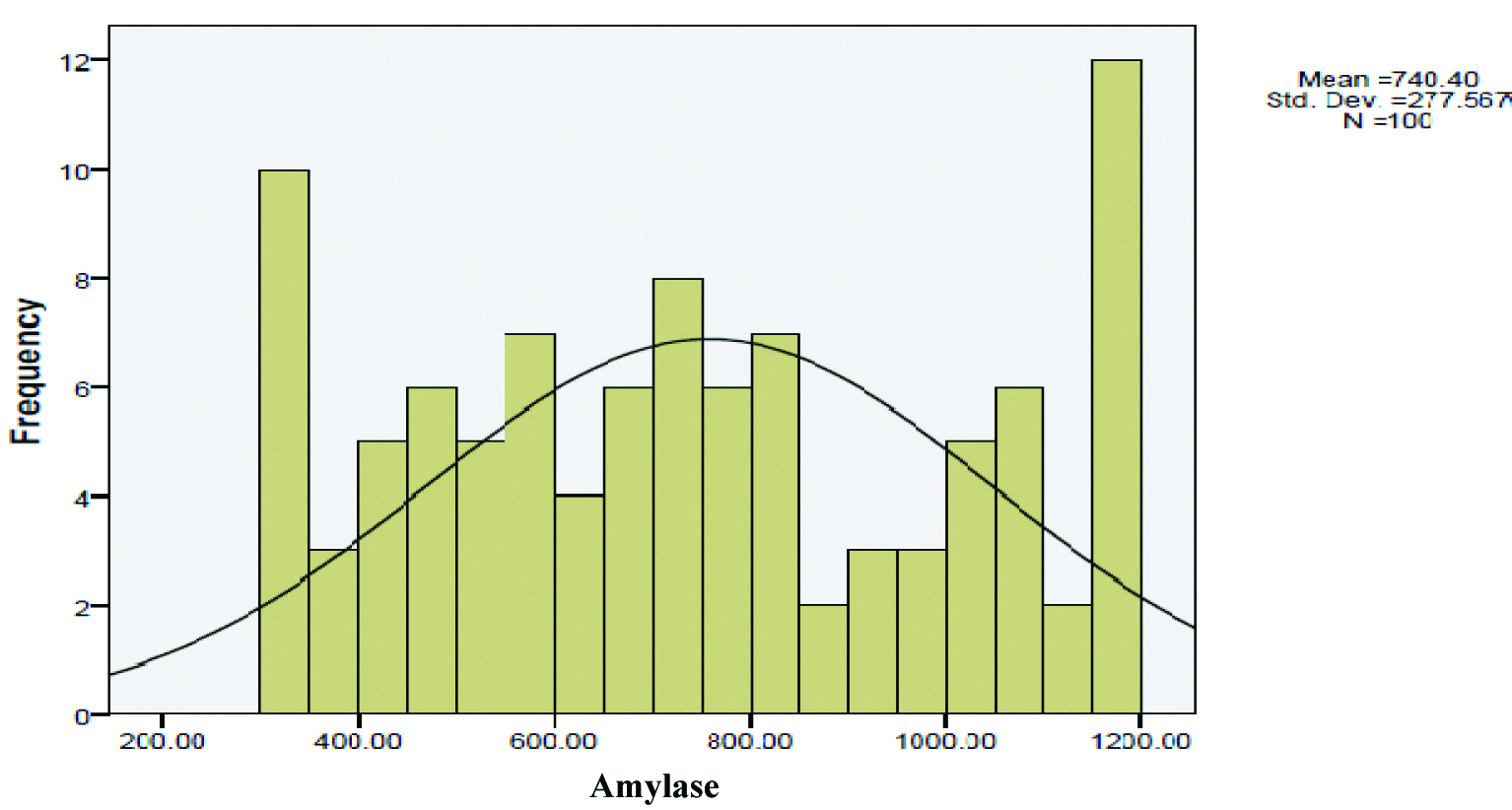
Average serum amylase level before PEG precipitation was 740.4±277.567 U/L (median=736.5) and mean serum amylase level after the PEG precipitation method in females was higher than males. Highest and lowest serum amylase levels were 1199 and 302 U/L, respectively; [Table/Fig-2] shows the serum amylase level distribution before the PEG precipitation method.
Serum amylase levels before adopting PEG precipitation method.
Average serum amylase level after PEG precipitation was 578.3±240.05 U/L (median=577) and the mean serum amylase level after PEG was higher in females than males. No significant correlation was found between the mean level of serum amylase before and after PEG precipitation (p=0.478). Highest and lowest serum amylase levels were 1076 and 72 U/L, respectively; [Table/Fig-3] shows the distribution of serum amylase level after using the PEG precipitation method.
Serum amylase levels after adopting PEG precipitation method.

According to laboratory findings, the macroamylasemia was observed only for 4% (n=4) of patients and 96% (n=96) of patients had real hyperamylasemia. Four patients diagnosed with macroamylasemia had no high serum amylase level after PEG deposition test. There was no significant association between the serum amylase levels after using the PEG deposition method and macroamylasemia detection (p=0.649). There was also no patient suffering from both macroamylasemia and hyperamylasemia.
Comparison of Findings According to Gender
[Table/Fig-4] demonstrates the mean age and amylase levels before and after using the PEG precipitation method for both genders. Concerning the results, the mean age was higher in females than males and females had higher serum amylase levels before and after using the PEG precipitation method in comparison to males. However, there was no statistically significant difference between the two groups in this respect.
Mean age and serum amylase levels before and after adopting PEG precipitation method with regard to partcipants’ gender.
| Variables | Male (n=63) | Female (n=37) | p-value |
|---|
| Age | 49.11±14.91 | 50.14±19.01 | 0.5 |
| Amylase | 708.272±14.18 | 795.281±32.71 | 0.13 |
| Amylase after PEG precipitation | 554.236±4.69 | 619.245±59.75 | 0.19 |
Chi-square test; p<0.05=significant
[Table/Fig-5] shows the mean age and amylase levels before and after PEG precipitation for real hyperamylasemia and macroamylasemia. It can be seen that the mean age was higher in real hyperamylasemia patients than macroamylasemia patients; however, there was no statistically significant difference between these two groups (p=0.640). Serum amylase level was higher for real hyperamylasemia patients than macroamylasemia ones; however, no statistically significant difference was observed between the two groups (p=0.060).
Mean age and serum amylase levels before and after adopting PEG precipitation method for real hyperamylasemia and macroamylasemia groups.
| Variables | Real hyperamylasemia group (n=96) | Macroamylasemia group (n=4) | p-value |
|---|
| Age | 49.12±0.91 | 47.10±0.42 | 0.64 |
| Amylase | 750.278±66.06 | 494.97±88.17 | 0.06 |
| Amylase after PEG precipitation | 598.224±36.29 | 96.30±75.08 | <0.001 |
Chi-square test; p<0.05=significant
In real hyperamylasemia patients, the serum amylase level after PEG precipitation was higher in comparison to those with macroamylasemia. Furthermore, the differences between two groups were statistically significant (p<0.001).
Discussion
In this study, the frequency of macroamylasemia in patients with a high serum amylase level was detected. Of 100 patients, 4% of patients suffered from macroamylasemia and 96% of patients had real hyperamylasemia. According to the results and based on the high incidence of macroamylasemia in these patients, the importance of macroamylasemia observation for target patients was highlighted in this study, preventing unnecessary diagnostic and therapeutic measures in patients with the high serum amylase levels.
In a recent study conducted by Gubergrits N et al., on 186 patients with acute pancreatitis in 2014, the serum amylase and lipase levels and amylase urinary clearance ratio to creatinine urinary clearance level were measured and macroamylasemia was then measured using the PEG precipitation method and chromatography. Eleven percent of patients had macroamylasemia (15 patients with hyperamylasemia and 5 patients with a normal serum amylase level) [12]. Thus, patients with asymptomatic pancreatitis and increased amylase should first be checked for macroamylasemia. It is useful to check the presence of macroamylasemia, prior to performing costly and complicated examinations, in patients with few symptoms or in asymptomatic patients, because of the possibility of macroamylasemia presence in these patients. In these cases, if the presence of macroamylasemia is proved, there will be no need for further diagnostic and therapeutic measurements; however, real hyperamylasemia requires further diagnostic evaluations, hospitalisation and therapeutic measures and consequently more time and cost. These can be prevented by a quick macroamylasemia check.
There are various recent reports concerning the frequency of macroamylasemia. Sachdeva CK et al., detected the macroamylasemia frequency in western countries and reported it to be 0.4%; however, Bouglouga O et al., in a recent study conducted in France stated that the macroamylasemia frequency was 10% [4,13]; however, the macroamylasemia frequency in patients with a high serum amylase level was reported to be 4.5% [9]. In a study conducted in 2011 in Korea by Cho SY et al., macroamylasemia level was claimed to be 2.5% in patients with hyperamylasemia and 1% in the general population [14]. The findings of the present study were consistent with the ones obtained in a study carried out in the US in 1980 on 400 patients, indicating that there were 2.5% of hyperamylasemia patients with macroamylasemia and 1% of healthy individuals with the normal serum amylase level [7].
The frequency difference reported in the current study (4%) could be due to the limited number of patients as slight differences were also observed in various similar studies. Furthermore, this study was conducted on patients with a high serum amylase level; however, macroamylasemia can be present in people with the normal serum amylase level as well. However, this study like other similar studies demonstrates the high frequency of macroamylasemia in patients with a high serum amylase level and it was also mentioned that the investigation of macroamylasemia can be helpful especially in patients with a high serum amylase level when there is no diagnostic certainty. On the other hand, recent studies showed macroamylasemia can also be misdiagnosed in symptomatic patients with clinical symptoms like pancreatitis and high serum amylase levels and other acute abdomen diseases are misdiagnosed as acute pancreatitis [15]. Thus, it seems that investigation of macroamylasemia, even in the presence of clinical signs, can be of benefit.
With increasing levels of the serum amylase up to three times, the normal amylase specificity for diagnosis of acute pancreatitis increases. Macroamylasemia usually causes lower serum amylases levels than the real hyperamylasemia [16].
In the study, there were four patients with macroamylasemia and the male to female ratio was estimated to be 1:1. In other studies, the macroamylasemia frequency was higher in men than women due to unknown reasons. This inconsistency can be caused by the small size of population included in this study [6,10,13,17-19].
Limitation
The main limitation of the present study was a smaller sample size. Collection from a larger sample, could lead to more clear results.
Conclusion
This study showed significant correlation and importance of using the PEG method to examine macroamylasemia in patients with high serum amylase levels. Also, this study showed that a high percentage of the patients with high serum amylase levels suffered from macroamylasemia. Checking the macroamylase level in symptomatic patients with the acute abdomen is beneficial to prevent undertaking unnecessary interventional measurements. Patients with real hyperamylasemia had higher serum amylase levels after using PEG precipitation method in comparison to macroamylasemia patients. These results indicate PEG precipitation method as a trustable and more accurate method.
[1]. Chang J, Chung C, Diagnosing acute pancreatitis: amylase or lipase?Hong Kong J Emerg Med 2011 18(1):2010.1177/102490791101800104 [Google Scholar] [CrossRef]
[2]. Esmaili HA, Mehramuz B, Maroufi P, Ghasemi A, Pourlak T, Diagnostic value of amylase and lipase in diagnosis of acute pancreatitisBiomed Pharmacol J 2017 10(1):389-94.10.13005/bpj/1120 [Google Scholar] [CrossRef]
[3]. Banks PA, Freeman ML, Practice guidelines in acute pancreatitisAm J Gastroenterol 2006 101(10):237910.1111/j.1572-0241.2006.00856.x17032204 [Google Scholar] [CrossRef] [PubMed]
[4]. Sachdeva CK, Bank S, Greenberg R, Blumstein M, Weissman S, Fluctuations in serum amylase in patients with macroamylasemiaAm J Gastroenterol 1995 90(5) [Google Scholar]
[5]. Levitt MD, Ellis C, A rapid and simple assay to determine if macroamylase is the cause of hyperamylasemiaGastroenterol 1982 83(2):378-82. [Google Scholar]
[6]. Rajca B, Guda NM, Elevated amylase and lipase: physiology including non-pancreatitis related elevationsPancreas Biliary Dis 2016 :1-20.10.1007/978-3-319-28089-9_1 [Google Scholar] [CrossRef]
[7]. Klonoff DC, Macroamylasemia and other immunoglobulin-complexed enzyme disordersWest J Med 1980 133(5):392 [Google Scholar]
[8]. Um JW, Kim KH, Kang MS, Choel JH, Bae JW, Hong YS, Macroamylasemia in a patient with acute appendicitisJ Korean Med Sci 1999 14:679-81.10.3346/jkms.1999.14.6.67910642949 [Google Scholar] [CrossRef] [PubMed]
[9]. Isham C, Ridgeway N, Hedrick R, Cate J, Screening for macroamylase in a community hospitalClin Chem 1984 30(5):741-42. [Google Scholar]
[10]. Siddiqi HA, Salwen MJ, Shaikh MF, Bowne WB, Laboratory diagnosis of gastrointestinal and pancreatic disordersHenry’s Clinical Diagnosis and Management by Laboratory Methods 2016 :306 [Google Scholar]
[11]. Jensen DM, Royse VL, Bonello JN, Schaffner J, Use of amylase isoenzymes in laboratory evaluation of hyperamylasemiaDigest Dis Sci 1987 32(6):561-68.10.1007/BF012961542436867 [Google Scholar] [CrossRef] [PubMed]
[12]. Gubergrits N, Golubova O, Lukashevich G, Fomenko P, Elevated serum amylase in patients with chronic pancreatitis: Acute attack or macroamylasemia?Pancreatol 2014 14(2):114-16.10.1016/j.pan.2013.12.00424650965 [Google Scholar] [CrossRef] [PubMed]
[13]. Bouglouga O, Lawson-Ananissoh LM, Bagny A, Kaaga L, Redah D, Pancreatic cancer: Epidemiological, clinical, and management aspects in the department of hepatogastroenterology at the Lome Campus teaching hospital (Togo)Med Sante Trop 2015 25(3):323-26.10.1684/mst.2015.049026446745 [Google Scholar] [CrossRef] [PubMed]
[14]. Cho SY, Lee A, Lee HJ, Suh JT, Overlapping presence of macroamylasemia and hyperamylasemia in acute pancreatitisKorean J Lab Med 2011 31(2):98-100.10.3343/kjlm.2011.31.2.9821474984 [Google Scholar] [CrossRef] [PubMed]
[15]. Memar MY, Varshochi M, Shokouhi B, Asgharzadeh M, Kafil HS, Procalcitonin: The marker of pediatric bacterial infectionBiomed Pharmacother 2017 96:936-43.10.1016/j.biopha.2017.11.14929203386 [Google Scholar] [CrossRef] [PubMed]
[16]. Matull W, Pereira S, O’Donohue J, Biochemical markers of acute pancreatitisJ Clin Pathol 2006 59(4):340-44.10.1136/jcp.2002.00292316567468 [Google Scholar] [CrossRef] [PubMed]
[17]. Smith RC, Southwell Keely J, Chesher D, Should serum pancreatic lipase replace serum amylase as a biomarker of acute pancreatitis?ANZ J Surg 2005 75(6):399-404.10.1111/j.1445-2197.2005.03391.x15943725 [Google Scholar] [CrossRef] [PubMed]
[18]. Cappell MS, Acute pancreatitis: etiology, clinical presentation, diagnosis, and therapyMed Clin North Am 2008 92(4):889-923.10.1016/j.mcna.2008.04.01318570947 [Google Scholar] [CrossRef] [PubMed]
[19]. McPherson RA, Pincus MR, Henry’s clinical diagnosis and management by laboratory methods 2016 Elsevier Health Sciences [Google Scholar]