Ovarian cysts are sacs filled with fluid or a semi-liquid component that arise in an ovary. These cystic ovarian lesions are frequently found in premenopausal women by routine ultrasound examination. The main types of ovarian cysts include physiological cysts and functional cysts that can produce hormones. The functional cysts include follicular cysts that produce oestrogen and measure >3.0 cm, corpus luteum cysts that produce progesterone and theca lutein cysts that are considered a gestational trophoblastic disease. For simple ovarian cysts with no suspicious features detected via US, current follow-up guidelines have been established according to a consensus statement by the society of radiologists in US [1,2].
Pelvic US is an essential safe imaging modality that is routinely used to evaluate the ovaries. The majority of pelvic masses can be correctly categorised based on grayscale, and colour or power Doppler US features [3]. Few studies have shown epidemiological data concerning benign ovarian cysts. However, present study classified ovarian cysts and attempted to find correlations with parity, occupation, and age.
Sonographic evaluation of ovarian cysts improves the prevention of malignancy and complications. Complications of ovarian cysts, such as rupture and haemorrhage, usually occur in association with physiological (functional) cysts [4]. The US is very accurate and sensitive for assessing complications that may cause severe morbidity. However, when a haemorrhagic cyst ruptures, it may result in massive haemoperitoneum that could easily be detected in the pelvis [5]. Early pelvic ultrasound scans should be done for precise diagnosis and management of cysts, to avoid these complications. In the current study, we used specific criteria to discriminate cysts for classification, and features of malignancy were eliminated from the study. These criteria included the regularity of the cyst wall, septations, shape and internal debris. Many studies have classified cystic ovarian lesions, and different scoring systems exist for discriminating benign and malignant adnexal masses which include the cystic appearance and biloculate or multiloculated presentation [6]. These criteria were supported by biochemical tests and clinical histories of the patients.
The impact of age and parity on occurrence ovarian lesions had been reported in several studies. Age is a predisposing factor for several abnormalities including ovarian cancer [7]. In Sudan, information on sonographic classification of benign ovarian cysts was rare, and there were no epidemiological data concerning these lesions. Exact data on the prevalence of benign ovarian cysts and classification were lacking, and most studies that have been conducted emphasises on the incidence of malignancy in ovaries with age. Therefore, the present study was conducted with an aim to classify ovarian cysts based on sonographic appearance and to analyse their frequency among the study population and to identify associations between ovarian cysts with advancing age and parity.
Materials and Methods
The present study was a cross-sectional quasi-experimental study conducted in Khartoum, Sudan at Khartoum Clinical Centres from March 2015 to December 2015. The subjects were referred to the ultrasound department for TVS. The participants were selected using simple, convenient systematic sampling method. Some of the women were symptomatic, and a few were asymptomatic. Patients with features of ovarian malignancies or with a history of cancer were excluded from the study. A structured questionnaire was designed to gather the patient’s demographic data, such as age, clinical history, parity, and occupation.
Ethical Considerations
The study was approved by the higher education committee of the faculty of radiological sciences and medical imaging of Alzaiem Al-azhari University. Patients were informed of the importance of the study for which data were being collected and of the need for their co-operation and consent. They were also told that no name or identity would be revealed and all the personal data were kept confidential. The patients were made aware of the transvaginal scanning procedure, consented to the process and signed an informed consent form to use their data for research purposes.
The Ultrasound Examination
Transvaginal US scanning was performed using a high-frequency probe at 7 MHz. The patients were prepared and scanned in a supine position with hips slightly flexed. The tip of the probe was lubricated with gel and gently inserted into the vagina. The transducer was then moved and rotated to obtain longitudinal, transverse and coronal sections through the uterus, ovaries, and adnexae.
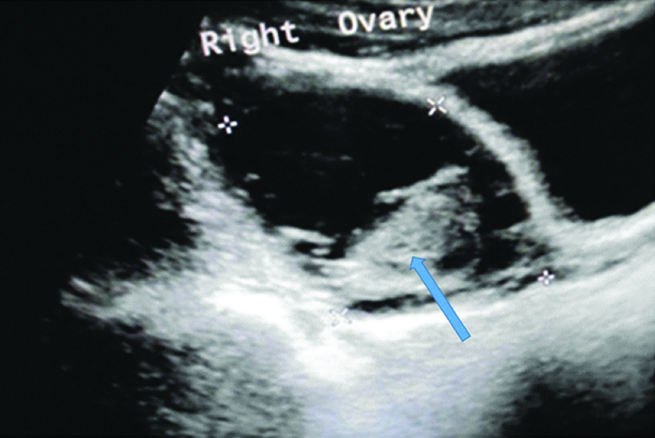
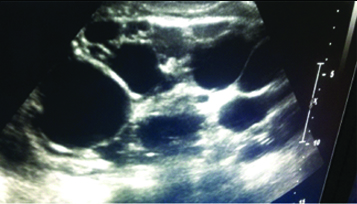
The sonographic criteria used to differentiate the ovarian cysts included the regularity of the wall, echogenicity and the presence of internal debris. However, an ovarian cyst was classified as a simple cyst (follicular or corpus luteal cyst) when it was anechoic, round, with a smooth, regular wall and measuring ≥3 cm [Table/Fig-1]. Corpus luteal cysts were always associated with pregnancy. A cyst with internal debris that mainly represents blood clotting was classified as a haemorrhagic cyst [Table/Fig-2]. POC were diagnosed when the ultrasound image revealed >10-12 follicles scattered peripherally in enlarged bilateral ovaries [Table/Fig-3]. Theca lutein cysts were large with thin walls located in enlarged ovaries. The patient’s clinical history and biochemical tests were integrated with the sonographic findings to accomplish the final interpretation.
A sonogram shows a follicular cyst in the left ovary of a 35-year-old women underwent TVS.

A sonogram demonstrates a haemorrhagic cyst at the right ovary of a 39-year-old women complained of right iliac pain. Arrow points to a solid component which represents blood clotting.
A sonogram depicts a polycystic ovary of a 23-year-old women.
Statistical Analysis
The results were analysed using SPSS version 19.0 software program (SPSS Inc., Chicago, IL, USA). Most of the variables were qualitative, and we used a non-parametric test (Pearson’s chi-squared) to find relationships between ovarian cysts and age, parity, occupation and the location within the ovaries. A p-value <0.05 was considered statistically significant for an association. Percentages were used to describe the frequency of the ovarian cysts in the study population.
Results
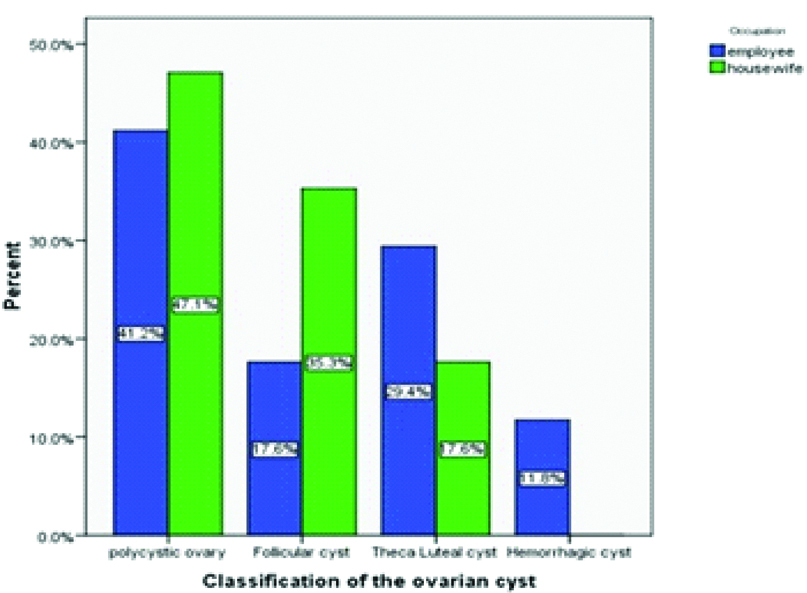
The study population was composed of 100 women of different ages and parity: the age range was 18-45 years. The mean age was 33.37±6.88 years. The patients were categorised into three age groups, to highlight the incidence of ovarian cysts among the groups [Table/Fig-4]. The demographic characteristics of the participants in addition to cysts location in ovaries were demonstrated in [Table/Fig-5]. POC were more common in housewives than employed women (47.1% vs. 41.2%). Follicular cysts were more common in housewives than employed women (35.3% vs. 17.6%), theca lutein cysts were more common in working women than housewives (29.4% vs. 17.6%). Haemorrhagic cysts were less frequent and were present only in employed women (11.8%) as shown in [Table/Fig-6]. There was a significant relationship between the incidence of ovarian cysts and age (p-value ≤0.001), as shown in [Table/Fig-7].
Frequency of age distribution of the participants.
| Age groups | Frequency | Percent |
|---|
| 17-25 years | 16 | 16% |
| 26-35 years | 35 | 35% |
| 36-49 years | 49 | 49% |
Demographic characteristics of the study population diagnosed with ovarian cysts.
| Demographic characteristics | n | % |
|---|
| Parity |
| Nulliparous | 72 | 72% |
| Multiparous | 28 | 28% |
| Occupation |
| Housewives | 67 | 67% |
| Employee | 33 | 33% |
| laterality |
| Bilateral | 56 | 56% |
| Unilateral | 44 | 44% |
| Side |
| Right ovary | 23 | 23% |
| Left ovary | 21 | 21% |
Distribution of ovarian cysts in relation with patients, occupation.
Distribution of the ovarian cysts among age groups.
| Age groups (years) | Classification of the ovarian cyst | Pearson chi-square |
|---|
| Polycystic Ovary | Corpus luteal | Follicular cyst | Theca luteal cyst | Haemorrhagic cyst | Total | p-value |
|---|
| 17-25 | 12 | 0 | 2 | 0 | 0 | 14 | ≤0.001 |
| 26-35 | 24 | 2 | 4 | 12 | 2 | 44 |
| 36-49 | 14 | 5 | 13 | 8 | 2 | 42 |
| Total | 50 | 7 | 19 | 20 | 4 | 100 |
The parity status was correlated with the type of ovarian cyst as shown in [Table/Fig-8]. The laterality of ovarian cysts was found to be significantly associated with the incidence; however, the sidedness was associated with the prevalence (p-value ≤0.001 and 0.22 respectively) as shown in [Table/Fig-9]. It was observed that POC mostly affected both ovaries (45%), follicular cysts were more common in the left ovary than the right ovary (10% vs. 8%) and theca lutein cysts affected ovaries bilaterally more than unilaterally (10 %). The factors that may affect the classification and occurrence of ovarian cysts are age, occupation, the size of the cysts and their location within the ovaries. Age, Size of the cyst and laterality were highly significantly correlated with the classification and occurrence of ovarian cysts (p-value ≤0.001). It was observed that size of the cysts has the strongest significant correlation (r=0.79, p-value ≤0.001) [Table/Fig-10].
Effect of parity on ovarian cysts and their distribution among the participants.
| Ovarian cysts | Parity | Total | p-value |
|---|
| Nulliparous | Multiparous |
|---|
| Polycystic ovary | 38 | 12 | 50 | 0.02 |
| Corpus Luteal | 3 | 4 | 7 | 0.66 |
| Follicular cyst | 13 | 6 | 19 | 0.18 |
| Theca Luteal cyst | 16 | 4 | 20 | 0.42 |
| Haemorrhagic cyst | 2 | 2 | 4 | NA |
| Total | 72 | 28 | 100 | |
Comparison of laterality and side which influence occurrence ovarian cysts.
| Parameter | Frequency | Chi-square | p-values |
|---|
| Number | Percentage |
|---|
| Laterality | Bilateral | 56 | 56% | 26.087 | ≤0.001 |
| Unilateral | 44 | 44% |
| Side | Left ovary | 21 | 21% | 3.315 | 0.22 |
| Right ovary | 23 | 23% |
Chi-square for a one-dimensional “goodness of fit” test is used. Calculations done at df=1
the result is significant at p≤0.05
Correlation of maternal demographic factors, location and size of the cysts with prevalence of ovarian cysts.
| Variable | Correlation coefficient (r) | Significance p-values |
|---|
| Age | 0.27 | ≤0.001** |
| Occupation | -0.18 | 0.134 |
| Laterality in ovaries | -0.55 | ≤0.001** |
| Size of cysts | 0.79 | ≤0.001** |
Spearman correlation was used. Calculations done at df=1
**the result is significant at p≤0.05
Discussion
In the present study, it was observed that the prevalence of POC was 50% and was most common in patients aged 26-36 years. Ramanad SJ et al., reported that the prevalence of PCO was 5-10% [8]. In other studies, the prevalence of PCO was found to affect 8% and 20% of women of reproductive age worldwide [9]. However, the prevalence in present study was much higher than those finding since the sample size was not large enough. It was observed the incidence decreased with increasing age. Johnstone EB et al., assessed the effect of age on the prevalence of PCO and reported that the prevalence was 32% and reduced with age [10]. This reduction indicates that age was a significant factor affecting the incidence of PCO among ovulatory women.
The present study revealed that PCO is more common among nulliparous women than multiparous women. The results show that parity was a statistically significant factor for the incidence of ovarian cysts especially the POC (p-value=0.02). This finding agrees with Mandiwa C et al., who reported that increased parity had a lower risk of ovarian cysts [11]. It was found that theca luteal cysts, follicular cysts, and haemorrhagic cysts were not statistically associated with parity. This finding agrees with those of Abdulgabbar HS et al., who studied 244 cases of ovarian cysts and found that parity was not a significant factor (p-value=0.750) [12].
Follicular cysts are a type of simple physiological ovarian cyst. The current study revealed that follicular cysts mostly affected women 36-49-years-old. This finding contradicts to those of a survey conducted by Alcazar JL et al., who reported that simple ovarian cysts are relatively common among postmenopausal women, although others have stated that they are common in premenopausal women [13,14]. In the present study, the incidence of corpus luteal cysts among the study population was 7%. These cysts formed as a result of a failure of the corpus luteum to regress and enlarge with or without haemorrhage. The majority of these cysts spontaneously involute at the end of the 2nd trimester [15]. In the present study, these cysts were more common in multiparous than nulliparous women because they were always associated with pregnancy. They involved the left ovary more than the right ovary (4 vs. 3).
In the present study, haemorrhagic ovarian cysts were the least frequent (4%). These cysts usually occur as a result of haemorrhage within the corpus luteum or other functional cysts. These cysts cause acute pelvic pain in premenopausal women and can occur during pregnancy. They may be asymptomatic and are found incidentally [16,17]. On US examination, they reveal different appearances depending on the stage and chronicity of the blood products and clotting, such as lace-like reticular echoes, intracystic solid clots, and fluid-fluid levels [18]. The present study showed that they were present in working women, and the majority was located in the right ovary.
Theca lutein cysts were the second type of benign ovarian cysts evaluated in present study. They are functional cysts, typically present in multiples and are seen bilaterally. They have a very high association with gestational trophoblastic disease and multifetal pregnancy [19]. In the current study, these cysts were common at reproductive age (26-35-year-old), and they affected both ovaries, consistent with the results of Chiang G and Levine D, who found that these cysts were always seen bilaterally and were associated with hydatidiform moles [20]. It was observed that these cysts were more common in nulliparous than in multiparous women (16 vs. 4). This elevation could be attributed to the fact that nulliparous women consume hormone therapy to enhance and accelerate pregnancy [21]. These cysts involved both ovaries because the secreted hormone, equally stimulated both ovaries.
In the present study, we found parity; age and laterality were significant factors affecting the incidence and classification of benign ovarian cysts. Parity was a considerable factor for PCO cysts (p-value=0.02), most of the cysts were more common in nulliparous than multiparous women (73% vs. 27%). This finding agreed with previous studies that reported the risk of ovarian cysts was reduced with increased parity [11]. In previous studies, high parity levels were inversely associated with a lower risk of ovarian cancer [22]. Age was found to be significantly associated with benign ovarian cysts (p-value ≤0.001). This result was inconsistent with Emeksiz HC et al., who reported that the frequency of ovarian cysts increased with advancing age [23]. On the other hand, the occupation had no statistical correlation with the occurrence of ovarian cysts (p-value=0.576). In previous studies, the epidemiological data has much discussed the ovarian cancer [24]. However, we did not find epidemiologic data demonstrating a relationship between occupation and the incidence of ovarian cysts.
The current study revealed that the location of ovarian cysts (laterality and sidedness) was a statistically significant factor in the occurrence of ovarian cysts (p-value ≤0.001). The Present finding contradicted with Vercellini P et al., who reported no significant difference between the left and right-sided ovarian cysts among the groups [25]. The disparity in result between the two studies is attributed to the criteria taken for diagnosing the ovarian lesions. In the present study, it was observed PCO, and theca lutein cysts always affected both ovaries, while follicular, and corpus luteal cysts involved a unilateral ovary. It was found that 45 out of 50 cases of PCO affected both ovaries, while follicular and corpus luteal cysts involved unilateral ovaries, especially the left ovary. These findings supported that laterality is a significant factor which influences benign ovarian cysts.
The present study revealed that the size of ovarian cysts significantly affects cyst classification (p-value ≤0.001) and is strongly correlated with the type of ovarian cyst (r=0.79). A previous study conducted by Ganjei P et al., investigating the accuracy of cytology to differentiate neoplastic and non-neoplastic ovarian cysts concluded that overall diagnostic efficiency was improved from 63% to 69% when cyst size was taken into consideration [26]. Although, they studied benign and malignant ovarian cysts and present study emphasised benign cysts only, the results strongly support present finding that the size of the cyst could be used as an indicator of ovarian cyst classification.
Limitation
The major limitation facing the present study that some participants refused to be investigated since they thought that ultrasound may cause biological hazards as X-rays do.
Conclusion
The benign ovarian cysts were well characterised and classified as follicular cysts, corpus luteal cysts, theca lutein cysts or PCO. Polycystic ovarian cysts were more frequent in housewives than in employed women. Theca lutein cysts were the second most common type, and simple follicular cysts were the third most common. Age and parity were statistically significant factors for the classification and occurrence of ovarian cysts. Further studies were recommended to confirm the impact of parity and age on incidence of ovarian cysts.
Chi-square for a one-dimensional “goodness of fit” test is used. Calculations done at df=1
the result is significant at p≤0.05
Spearman correlation was used. Calculations done at df=1
**the result is significant at p≤0.05