Sarcomatoid Lung Carcinoma-A Rare Entity
Jyoti Bajpai1, Surya Kant2, Abhishek Verma3, Darshan Kumar Bajaj4, Ved Prakash5
1 Senior Resident, Department of Respiratory Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
2 Professor and Head, Department of Respiratory Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
3 Junior Resident, Department of Respiratory Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
4 Assistant Professor, Department of Respiratory Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
5 Associate Professor, Department of Respiratory Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Surya Kant, Professor and Head, Department of Respiratory Medicine, King George’s Medical University, Lucknow-226003, Uttar Pradesh, India.
E-mail: skantpulmed@gmail.com
Sarcomatoid Carcinoma (SARC) of lung is an uncommon poorly differentiated variant of lung cancer. It is biphasic neoplasm and combination of malignant epithelial and mesenchymal cells. Most of the cases are associated with advanced disease and metastasis. It is aggressive form of non small cell lung cancer. Here we report a case of sarcomatoid lung cancer in 65-year-old smoker male.
Histopathology, Non small cell carcinoma, Sarcoma, Smoking
Case Report
A 65-year-old male farmer by occupation with a history of beedi smoking (60 pack year) presented in the Department of Respiratory Medicine with dyspnea on exertion, loss of appetite and dry cough for last two months. There was no history of haemoptysis, dysphagia, fever, and chest pain. His symptoms were not associated with any seasonal variation. There was no history of diabetes mellitus, hypertension, any past medical and surgical history, and no significant family history. Informed consent was obtained from patient regarding the use of his case details. On physical examination, he was looking ill, pallor, clubbing and right axillary lymphadenopathy was present. On respiratory system examination, decreased movement of right hemithorax and bilateral wheez was present.
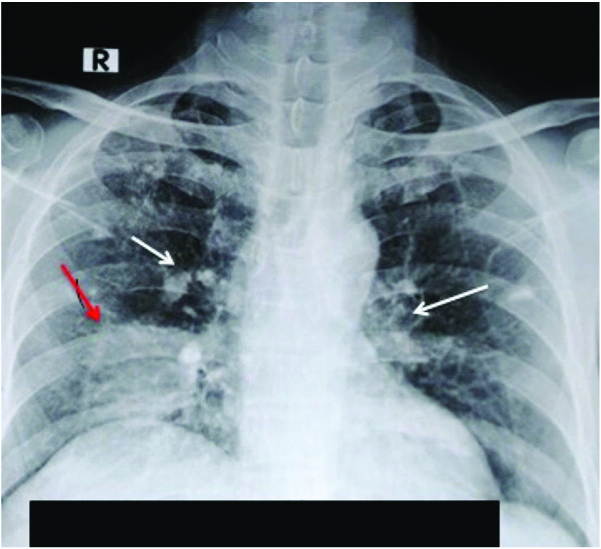
On chest radiograph, there was an intrathoracic mass in right lower zone with bilateral hilar calcifications [Table/Fig-1].
Chest radiograph (posteroanterior view) showed intrathoracic mass in right lower zone (red arrow) with bilateral hilar calcifications (white arrow).
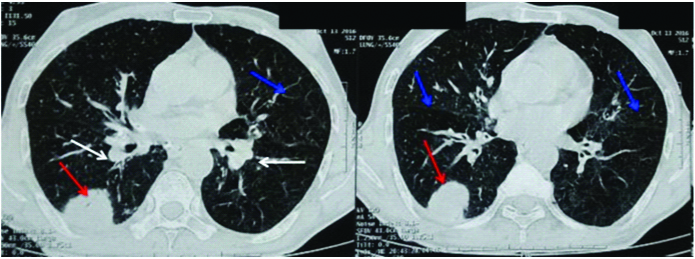
Chest CT scan showed a mass in right lower lobe with speculated (calcified) contour that measured 36×24 mm. The mass was associated with subcarinal and bilateral hilar lymphadenopathy with centriacinar emphysematous changes [Table/Fig-2].
Chest CT scan lung window showed a mass in right lower lobe (red arrow) with bilateral hilar lymphadenopathy (white arrow) with centriacinar emphysematous changes (blue arrow).
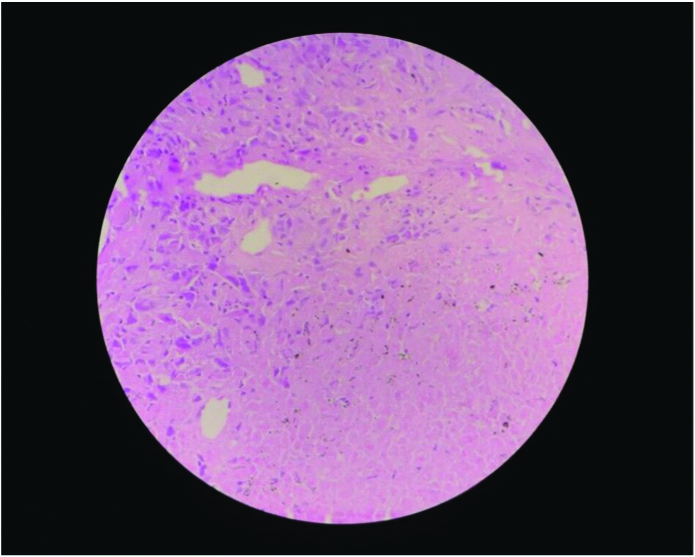
However, no visceral lesion was observed after abdominal ultrasonographic examination. CT-scan guided intrathoracic mass biopsy was done. Histopathological examination of biopsy tissue showed area of necrosis in between sheets of tumour cells. Tumour cells are polygonal to spindle shaped with elongated hyperchromatic nuclei [Table/Fig-3]. Histopathology evidences supported the dignosis of SARC, with carcinomatous proliferation of pleomorphic spindle cells. On Immunohistochemistry (IHC) tumour cells were positive for vimentin, pancytokeratin. However, they were negative for p63, Thyroid Transcription Factor-1 (TTF-1), cytokeratin 7, 20 and calretinin and EMA was not done. The tumour was classified as clinical stage IV (T2N3M1b) and the patient received following platinum based chemotherapy: gemcitabine (1250 mg/m2 D1, D8) and cisplatin (80 mg/m2 D1). Patient completed first cycle of chemotherapy and then was lost to follow-up in the outpatient department.
Histopathological examination from right mass showed area of necrosis in between sheets of scattered tumour cells. Tumour cells are polygonal to spindle shaped with elongated hyperchromatic nuclei (H&E, 40X).
Discussion
Lung cancer is very heterogenous in respect of histology pattern. Pulmonary SARC is one of them. The SARC is high grade tumour occurring in lung. The diagnosis of SARC of the lung includes a group of poorly differentiated non small cell lung tumours, which include a component with sarcomatoid differentiation like spindle cell and giant cell population or a sarcoma component. The SARC is very rare and has very poor prognosis than conventional non small cell carcinoma. The incidence is only 0.1-1.3% of all malignant lung tumours [1]. There are very few case reports are reported in literature. They affect more frequently males than females, average age at diagnosis is 60 years [2]. They are strongly associated with smoking. SARC is rapid growing, invasive tumour. Recurrence and metastasis are most commonly seen in sarcomatoid lung cancer. Pulmonary SARC is bizarre tumours known as “miniature monsters” in which the activation of an Epithelial–Mesenchymal Transition (EMT) program is likely to play a relevant role in their development [3]. Carcinomas containing variable amounts of sarcomatous or sarcomatoid elements (in the form of spindle and/or giant cells) or entirely made up of these tissues are rare but well recognised entities in lung cancer pathology [4].
In 2004, WHO classified SARC into pleomorphic carcinoma, spindle cell carcinoma, carcinosarcoma, giant cell carcinoma, pulmonary blastoma [5]. Lung carcinosarcoma is a high grade dual phase tumour with both epithelial and mesenchymal component. Metastasis is usually seen frequently at the time of diagnosis. Most of SARC has diagnosed in late stage. In SARC 27% is the survival rate at six months [6]. Four major hypotheses emerged to explain sarcomatoid neoplasms: the embryonic rest hypothesis, suggesting derivation from misplaced “mini organs” that are complete with epithelium and stroma, the collision hypothesis, implicating separate but concomitant proliferations of malignant epithelium and mesenchyme, the stromal induction/metaplasia hypothesis, proposing that sarcomatous elements are an atypical response to the growth of a carcinoma rather than neoplastic, and the totipotential hypothesis, which is based on tumour origin from a single stem cell that differentiates into separate epithelial and mesenchymal components [7]. Dyspnea, cough, haemoptysis, and chest pain are common symptoms. In proximal sarcomatoid lung cancer haemoptysis is a common symptom seen in 50% cases [8]. Presence of Keratin and Epithelial Membrane Antigen (EMA) markers are strongly supportive of epithelial component. In the present case tumour cells were positive for pancytokeratin, cytokeratin, vimentin, carcinoembryonic antigen. The EMA was not done. In the present case pancytokeratin, keratin and carcinoembryonic antigen are in favour of epithelial component while vimentin support sarcoma component. The TTF-1 may be positive in giant cell carcinoma variants. The SARC has also been evaluated for Epidermal Growth Factor Receptor (EGFR) and K-ras mutation.
For localised tumours, surgery is primary treatment; for metastatic and advanced tumour they are treated as per non small cell lung cancer guideline. Chemotherapy agents for the SARC are same as those used for non small cell lung carcinoma [9]. Doxorubicin and ifosfamide is also been used in treatment of metastatic SARC in 15 patients in which 50% showed partial responses to short term chemotherapy with doxorubicin and ifosfamide. However, all patients experienced disease progression and died despite continuous treatment [10].
Conclusion
The SARC of the lung has very less research data. The histological and immunohistochemical characteristics of this tumour type are very specific. They are chemorefractory tumour with poor prognosis. Surgery is main management for localised tumour. Mean survival of 9-12 month after complete resection of tumour. Platinum based chemotherapy as used in non small cell carcinoma is treatment for advanced disease. Conventional chemotherapy is not promising in management of SARC further study and research needed in this field for better outcome.
[1]. Rossi G, Cavazza A, Sturm N, Migaldi M, Facciolongo N, Longo L, Pulmonary carcinomas with pleomorphic, sarcomatoid, or sarcomatous elements: a clinicopathologic and immunohistochemical study of 75 casesAm J Surg Pathol 2003 27(3):311-24.10.1097/00000478-200303000-0000412604887 [Google Scholar] [CrossRef] [PubMed]
[2]. Venissac N, Pop D, Lassalle S, Berthier F, Hofman P, Mouroux J, Sarcomatoid lung cancer (spindle/giant cells): an aggressive disease?J Thorac Cardiovasc Surg 2007 134(3):619-23.10.1016/j.jtcvs.2007.05.03117723808 [Google Scholar] [CrossRef] [PubMed]
[3]. Pelosi G, Sonzogni A, De Pas T, Galetta D, Veronesi G, Spaggiari L, Review article: pulmonary sarcomatoid carcinomas: a practical overviewInt J Surg Pathol 2010 18(2):103-20.10.1177/106689690833004919124452 [Google Scholar] [CrossRef] [PubMed]
[4]. Travis WD, Brambilla E, Muller-Hermelink KH, Harris CC, Tumours of the lung, pleura, thymus and heart 2004 Lyon, FranceIARC Press:344 [Google Scholar]
[5]. Travis WD, Sarcomatoid neoplasms of the lung and pleuraArch Pathol Lab Med 2010 134:1645-58. [Google Scholar]
[6]. Vidal-Losada MJ, Bernal-Monterde V, Amores-Arriaga B, Ferrer Pérez AI, Serrano Solares S, Tobeña Puyal M, Lung carcinosarcomaClin Transl Oncol 2010 12(4):303-05.10.1007/s12094-010-0508-6 [Google Scholar] [CrossRef]
[7]. Padgett DM, Cathro HP, Wick MR, Mills SE, Podoplanin is a better immunohistochemical marker for sarcomatoid mesothelioma than calretininAm J Surg Pathol 2008 32:123-27.10.1097/PAS.0b013e31814faacf18162779 [Google Scholar] [CrossRef] [PubMed]
[8]. Yoshino N, Kubokura H, Yamauchi S, Ohaki Y, Koizumi K, Shimizu K, A true pulmonary carcinosarcoma that required diagnostic differentiation from a pleomorphic adenoma: a case reportAnn Thorac Cardiovasc Surg 2009 15:42-45. [Google Scholar]
[9]. Mason RJ, Broaddus VC, Martin T, King T, Schraufnagel D, John F, Rare malignant primary pulmonary epithelial tumours. Ch. 48, Part 4. Primary Pulmonary SarcomasMurray and Nadel’s Textbook of Respiratory Medicine 2010 5th ed [Google Scholar]
[10]. Staddon AP, Crawford EA, Hartner L, Lackman RD, Ogilvie MC, Treatment of metastatic sarcomatoid carcinoma with doxorubicin and ifosfamideJ Clin Oncol 2008 26:2151810.1200/jco.2008.26.15_suppl.21518 [Google Scholar] [CrossRef]