Introduction
Trauma is a modern day epidemic and a cause of significant morbidity and mortality. Of all the major subsets, Abdominal Trauma (AT) stands third in terms of the incidence and is one of the most common causes of trauma related deaths that is preventable [1]. Approximately 85% of AT is caused by blunt injury [2]. The management of BAT has almost come full circle; from conservative management of all such cases which was professed in the early 20th century to a mandatory surgical exploration and now to a selective NOM in such cases [3,4].
The concept of NOM in BAT originates from attempts at spleen preservation in paediatric patients with splenic injury. This was a result of concerns of overwhelming post spelenctomy sepsis that was reported in the landmark article by Singer DB, in the 1970s [5]. This concept was adopted in adult patients too, and slowly all patients with solid organ injury who were haemodynamically stable and without peritoneal signs were increasingly being managed by NOM with a success rate of about 80% [6,7]. Few significant factors contributing to this is the availability of better cross sectional imaging, better intensive care, easy availability of blood products and emergence of intervention radiology.
While NOM is being extensively applied to liver, splenic and renal injury, it is still controversial when it comes to pancreatic trauma especially for higher grade injuries [8]. Further, previous studies have reported that high grade injuries of solid organs, especially the spleen, in BAT are a risk for failure of NOM [6]. Studies have also shown that failure of NOM is highest with splenic injury due to higher rates of rebleeding [6,9-11]. The decision making is critical in managing high grade solid organ injuries: to go in or not to go in! In present study, we look at the outcomes of high grade solid organ injuries in patients with BAT in whom NOM was attempted.
Materials and Methods
This was a retrospective study of all cases of BAT presenting to the Department of Surgical gastroenterology, Command Hospital Air force, Bangalore, India, between January 2013 to June 2017. Records of all cases of BAT were perused to compile data. Follow-up of the patients was updated till July 2017 either in the form clinical review or telephonic interview for patients who could not turn up for clinical review.
The primary outcome measure of present study was the feasibility and success rate of NOM in abdominal trauma with high grade solid organ injury. The secondary outcome measures were the failure rate of NOM and the morbidity and mortality associated with NOM.
Inclusion Criteria
All cases of BAT abdomen with high grade solid organ injuries (Grade III or more) were included in the study.
Exclusion Criteria
Patients with BAT with peritoneal signs at presentation or with continued haemodynamic instability despite initial resuscitation, and those who died during resuscitation in the emergency.
Departmental Protocol for BAT Patients
The patients with BAT were received at the emergency and evaluated and resuscitated/managed as per the ATLS protocol [12]. Haemodynamically unstable patients received a bolus of crystalloids 1-2 liters (20 mL/Kg body weight in paediatric patients) and repeated once more, if necessary. At the end of this if they did not respond, they were considered unstable and as such not candidates for NOM. All patients who were stable or who were haemodynamically unstable, but attained stability following initial resuscitation were candidates for NOM. All patients underwent a FAST and those who were FAST positive and stable underwent a CECT of the abdomen and pelvis. Those who were FAST positive, but persistently unstable or had peritoneal signs were candidate for operative management. Extra-abdominal injuries were evaluated/managed by the respective specialists.
The NOM candidates were shifted to either ICU or acute surgical ward based on the need for close monitoring, associated comorbidities and concomitant extra-abdominal injuries. They were closely monitored for their haemodynamic parameters, abdominal signs, urine output and a 6-12 hourly haemoglobin (Hb) and haematocrit levels along with other relevant blood investigations. Criteria for abandoning NOM were haemodynamic instability, requirement of blood transfusion in excess of four units or the appearance of peritoneal signs.
Definitions
High grade Solid organ injury: All solid organ injuries were graded as per the organ injury scale given by American Association of Surgery for Trauma (AAST) [13]. All injuries, grade III or more were considered high grade injuries.
Haemodynamically unstable: A systolic BP of <90 mmHg and a pulse rate more than 100/minute.
Injury severity score (ISS): Was calculated as per the method described by Baker et al., [14].
Blood transfusion trigger: During resuscitation, packed RBCs were transfused to non/transient responders. Beyond the resuscitation phase, in a patient of upto 55 years of age, a Hb of less than 7 g/dL (to maintain Hb between 7 and 9 g/dL) and in older patients with cardiac comorbidities, a Hb of less than 9 g/dL (to maintain Hb between 9 and 11 g/dL) was used as the transfusion trigger.
Successful NOM: The absence of the need for surgical exploration in patients with abdominal trauma during the hospital admission or 30 days since the time of injury, which ever was later.
Failure of NOM: Those patients who were received at the ICU/ Surgical ward for NOM and subsequently were operated upon for abdominal injury for any reason were defined as failures of NOM. If any patient underwent surgery for non-abdominal causes, it was not considered as a failure of NOM.
Statistical Analysis
The Data was tabulated on a Microsoft Excel chart and analysed using an online statistical software calculator ‘Graphpad’ available at www.graphpad.com. Numerical variables were presented as Mean±SD or Median and Range and the categorical variables as frequencies and percentages.
Results
During the study period, 2176 patients were admitted for trauma at hospital. Of these, there were 42 cases of abdominal trauma of which, 17 patients were admitted with high grade solid organ injuries.
The patients were mostly young with a median age of 28.5 years and the majority was males. A road traffic accident was the predominant mode of injury followed by fall from a height and fall on an object. Five patients were haemodynamically unstable at presentation and one patient needed endotracheal intubation as he had a flail chest. All haemodynamically unstable patients responded to fluid challenge and a decision was made to manage them non-operatively. All these five patients were initially managed in the ICU and the rest were closely monitored in the acute surgical ward [Table/Fig-1].
Patient demographics and initial evaluation.
| Variables | n=17 |
|---|
| Age, years* | 28.5 (4-61) |
| Males, n (%) | 14 (82.3) |
| ISS score# | 17.21±8.5 |
| Haemodynamically unstable at presentation, n (%) | 5 (29.4) |
| Endotracheal intubation, n (%) | 01 (5.8) |
| FAST Positive, n (%) | 17 (100) |
| Contrast extravasation on CT scan | 02 (11.8) |
| ICU admission, n (%) | 05 (29.4) |
| Mechanism of Injury, n (%) |
| Road traffic accident | 13 (76.5) |
| Fall from a height | 02(11.8) |
| Fall on an object | 02 (11.8) |
Distribution of Injuries
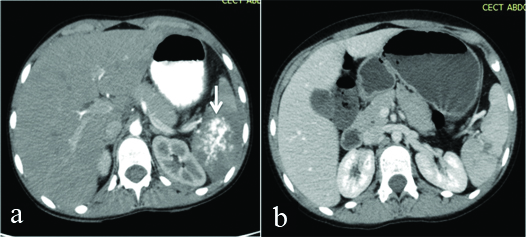
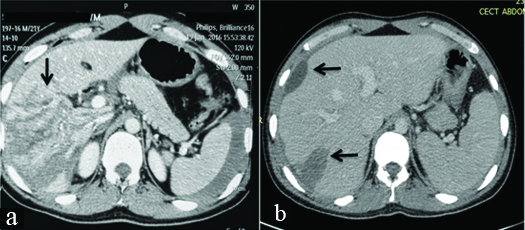
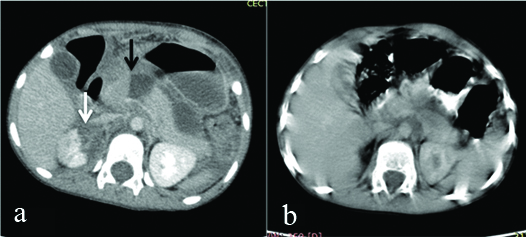
Eight patients had concomitant extra-abdominal injuries one head injury; four chest injuries-flail chest and fracture of ribs; two fracture of long bones-femur and humerus, and one spinal cord injury with paraplegia). Ten patients had isolated solid organ injury whereas seven patients had multiple solid organ injuries. Spleen was the predominant organ involved-11 patients (64.8 %) followed by Liver-10 (58.8 %) [Table/Fig-2a,b,3a,b]. There was one pancreatic trauma [Table/Fig-4a,b,5].
a) Axial section from CECT abdomen in a nine-year-old boy with blunt injury abdomen showing Grade V splenic injury with contrast blush (white arrow); b) Imaging finding after 2 months in the same patient showing an almost healed spleen with no pseudoaneurysm.
a) Axial section from CECT abdomen in a 19-year-old male with blunt injury abdomen showing Grade V liver injury (black arrow); b) Imaging finding after 1 month in the same patient showing a well regenerated liver with resolving haematomas (black arrows).
a) Axial section from CECT abdomen in a four-year-old girl with a cycle handle injury abdomen showing Grade IV Pancreatic injury (black arrow) and a grade III right renal injury (white arrow). She also had a grade III liver injury; b) Imaging finding after 5 weeks in the same patient showing resolving peripancreatic fluid collection with no duct dilatation or pancreatic atrophy
Severity and frequency of abdominal solid organ injury according the organ injury scale.
| Variables | n=17 |
|---|
| High grade Abdominal solid organ Injuries, n (%) |
| Isolated Spleen | 5 (29.4) |
| Isolated Liver | 5 (29.4) |
| Combined Pancreas, Liver and Kidney | 1 (5.9) |
| Combined Liver and Spleen | 4 (23.5) |
| Combined Spleen and kidney | 2 (11.8) |
| Grade III |
| Spleen | 6 |
| Liver | 5 |
| Kidney | 3 |
| Pancreas | 0 |
| Grade IV |
| Spleen | 4 |
| Liver | 3 |
| Kidney | 0 |
| Pancreas | 1 |
| Grade V |
| Spleen | 1 |
| Liver | 2 |
| Kidney | 0 |
| Pancreas | 0 |
| Associated extra-abdominal injuries (n=08) |
| Head | 01 |
| Chest | 04 |
| Long bones | 02 |
| Spine | 01 |
Hospital course
Six patients needed blood transfusions and the mean transfusion requirement was 0.94±1.1 units of packed red blood cells. All 17 patients were managed non-operatively and none failed NOM. Three patients, all with splenic injuries, had rebleeding. One on day six and the other two on day seven following trauma, respectively All three could be managed non-operatively. There were three morbidities; two abscesses-one each in a patient with liver and splenic trauma, respectively and another patient with liver trauma developed basal atelectasis. There were no mortalities and the median hospital stay was 14.5 days (range; 9-36 days) [Table/Fig-6].
Hospital course of the patients.
| Variables | n=17 |
|---|
| Operative management for abdominal injuries, n (%) | 0 |
| Non-operative management, n (%) | 17 (100) |
| Failure of non-operative management, n (%) | 0 |
| Extra-abdominal surgeries, n (%) | 04 (23.5) |
| Blood transfusion# | 0.94±1.1 |
| Rebleeding, n (%) | 03 (17.6) |
| Morbidity | 03 (17.6) |
| Mortality, n (%) | 0 |
| Hospital stay* | 14.5 days (9-36) |
Discussion
Globally, trauma has assumed epidemic proportions and BAT constitutes 6-31% of all trauma cases [15,16]. What is of concern is that the majority of these patients are in the productive age group, thus causing a colossal loss to the family and the society [17]. Road traffic accidents are the predominant cause of trauma. All these aspects are echoed in the finding of present study.
In the present, four and a half year’s study, we have shown that NOM for BAT is possible even in high grade injuries. To be more precise, we have never had to operate on any patient with BAT in that period. By this, we do not mean to state that all patients with high grade solid organ injury should be managed by NOM. What we would like to stress is that the approach should shift from selective NOM to selective operative management using diligent, repeated clinical examination, backed by cross sectional imaging, advanced critical care, interventional radiology and blood bank support. This translates into better patient outcomes at the cost of increased burden on the surgical team.
Five patients were haemodynamically unstable at presentation and all responded to fluid resuscitation and thus a decision was made to manage them non-operatively. We had three patients with rebleeding around the day 6-7, all involving spleen. Fortunately, in all three patients, we could pursue NOM with only one patient requiring blood transfusion. One study reported 12 patients of splenic trauma with delayed bleeding which were managed with NOM and achieved a success rate of 83% [18]. Rebleeding rates are the highest with spleen with reported rates upto 25% [3,6]. The present protocol did not include doing a CT scan at a planned interval. Instead, we repeated the imaging as and when the clinical condition warranted. Splenic Artery Embolization (SAE) is increasingly being used for spleen salvage. However, we did not have to resort to SAE for any patient [19].
Two patients, both with splenic injury, had contrast extravasation seen on the CT scans. Both were paediatric patients and we proceeded to manage them non-operatively despite this. Trauma protocols mandate an angioembolisation in a stable patient with contrast extravasation and surgery in an unstable patient. This is based on the fact that 80% of such adult patients with contrast extravasation on CT scan would fail a non-operative management. But in a paediatric patient, there is some emerging evidence that this does not necessarily need an intervention [20]. We believe that patients with contrast extravasation can be assigned to a trial of NOM though they may have a higher chance of failing it especially the adult patients.
While NOM is increasingly being adopted for trauma involving spleen, liver and kidney, it is less common when it comes to pancreas especially in the event of a disrupted pancreatic duct [8,21]. We had one case of Grade 4 pancreatic injury in a child of four years of age with an associated Grade III liver injury, Grade III renal injury and fracture of the femur. Traditionally, this would have entailed a surgery. Since, she was haemodynamically stable and did not show sign of generalised peritonitis, we decided to manage her non-operatively. It was also felt that operating for the pancreatic injury could worsen her bleeding from the liver injury due to the handling of the liver. On the other hand, if the NOM failed, we would be operating in a hostile abdomen due to traumatic pancreatitis. Predictably, she did develop a peripancreatic fluid collection but it needed no intervention. On a follow up CT scan done three months after the injury, the fluid collection had resolved with no pancreatic ductal dilatation or parenchymal atrophy or fistula. One study, with the largest cohort of pancreatic injury, attempted NOM in high grade pancreatic injury. Out of 26 patients, 10 could be managed non-operatively [8].
None of the present patients failed NOM. According to one large prospective study, approximately 10% of BAT patients will fail NOM [6]. When the authors analysed their organ specific failure rates, they found that spleen (28%) had the highest failure rates followed by kidney (11%) and none with liver injuries failed NOM. Others report a NOM failure rate between 2-33% [22].
Traditionally, it has been a practice to err on the side of laparotomy when dealing with high grade solid organ injuries. The issue of Non-Therapeutic Laparotomy (NTL) has been discussed in literature. While it was felt that NTL was a procedure with minimum morbidity and that it was better to explore and rule out significant injuries, it has been shown that it has its own set of complications [23-26]. Thus, it would be apt to state that with advanced imaging available today, NTLs should be avoided as far as possible.
Three patients developed complications. A patient with liver injury and another with splenic injury developed abscesses with persistent fever and had to undergo pig tail drainage and resolved thereafter. Another patient with liver injury developed basal atelectasis. We had no mortality. In literature, a mortality rate upto 7% has been reported [6,27]. Studies report higher morbidity in operated patient group as compared to the NOM group though the mortality is not significantly different [3,6,27].
Hospital stay was 14.5 days (range: 9-36 days). Patients with head injury, those operated for extra-abdominal injuries, those that developed rebleeding and those with abscess needing pigtail drainage required longer hospitalisation. Studies report a longer hospital stay with operative management as compared to the NOM group [3,6,27].
The advantage of NOM in these high grade injuries would be preservation of the organ(s) and its functions; avoiding of the risk of anaesthesia and surgery; avoiding NTLs; lower morbidity; and a shorter hospital stay. It also avoids additional surgical stress to a patient with an already compromised physiology. Further, in a patient with more than one abdominal organ injury, there is a potential risk of worsening the grade of injury/dislodging the clot from one organ while operating for an injury in another organ.
The disadvantages would be that it leads to additional burden on the trauma team as it needs repeated, close monitoring which is labor intensive. Also, in case the NOM failed, the surgeon would be operating on a patient who might be physiologically worse than he was at the initial period of admission and surgery could be rendered, more difficult due to inflammation in the abdomen like in pancreatic trauma or bowel injury.
Limitation
The present study has certain limitations. First, it a retrospective study though we had maintained a database. Second, the number of patients was not large. We could manage all such patients non-operatively. However, it’s not difficult to predict that some of them would eventually fail NOM. Third, there was only one case of pancreatic injury in our cohort. Pancreatic injury is a difficult subset and more numbers would be needed to draw firm conclusions.
Conclusion
We would like to say that NOM is feasible and safe even in high grade injuries in BAT. This decision is based on a sound clinical judgment and should be attempted at centers with facilities for critical care, interventional radiology and adequate blood bank facilities and would entail repeated close monitoring of patient to pick up any deterioration in the condition. The patient condition and not the grade of injury on imaging should dictate the line of management. Thus, we would like to reiterate: Treat the patient, not the image.
[1]. Yeo A, Abdominal trauma. In Chih HN, Ooi LL, editors. Acute Surgical Management 2004 World Scientific Publishing Company:327-33.10.1142/9789812563033_002014656904 [Google Scholar] [CrossRef] [PubMed]
[2]. Burch JM, Franciose RJ, Moore EE, Trauma. In: Brunucardi FC, editor. Principles of surgery 2005 2New YorkMcGraw Hill:129-87. [Google Scholar]
[3]. McCormack J, Royal Soc. Medicine. 84th edition. Derbyshire Royal Infirmary Derby DEI 2 QY: 555 JDC Bennett FRCS DCH Department of ENT 1991 [Google Scholar]
[4]. Raza M, Abbas Y, Devi V, Prasad K, Rizk KN, Nair PP, Non operative management of abdominal trauma-a 10 years reviewWorld J Emerg Surg 2013 8-52.10.1186/1749-7922-8-1423561288 [Google Scholar] [CrossRef] [PubMed]
[5]. Singer DB, Postsplenectomy sepsisPerspect Paediatr Pathol 1973 1:285-311. [Google Scholar]
[6]. Velmahos GC, Toutouzas KG, Radin R, Chan L, Demetriades D, Non-operative treatment of blunt injury to solid abdominal organs: a prospective studyArch Surg 2003 138(8):844-51.10.1001/archsurg.138.8.84412912742 [Google Scholar] [CrossRef] [PubMed]
[7]. Giannopoulos GA, Katsoulis EI, Tzanakis NE, Panayotis AP, Digalakis M, Nonoperative management of blunt abdominal trauma. Is it safe and feasible in a district general hospital? ScandJ. Trauma Resuscitation &. Emerg Med 2009 17:22-28.10.1186/1757-7241-17-2219439091 [Google Scholar] [CrossRef] [PubMed]
[8]. Koganti SB, Kongara R, Boddepalli S, Mohammad NS, Thumma V, Nagari B, Predictors of successful non-operative management of grade III & IV blunt pancreatic traumaAnnals of Medicine and Surgery 2016 10:103-09.10.1016/j.amsu.2016.08.00327594995 [Google Scholar] [CrossRef] [PubMed]
[9]. Velmahos GC, Chan LS, Kamel E, Murray JA, Yassa N, Kahaku D, Nonoperative management of splenic injuries: have we gone too far?Arch Surg 2000 135(5):674-79.10.1001/archsurg.135.6.67410843363 [Google Scholar] [CrossRef] [PubMed]
[10]. Ochsner MG, Factors of failure for nonoperative management of blunt liver and splenic injuriesWorld J Surg 2001 25(11):1393-96.10.1007/s00268-001-0138-911760740 [Google Scholar] [CrossRef] [PubMed]
[11]. Schwab CW, Selection of nonoperative management candidatesWorld J Surg 2001 25(11):1389-92.10.1007/s00268-001-0137-x11760739 [Google Scholar] [CrossRef] [PubMed]
[12]. American College of Surgeons: ATLS Advanced Trauma Life Support Program for Doctors 2004 7th EditionChicago, IL USA [Google Scholar]
[13]. AAST Injury Scaling and Scoring System. http://www.aast.org/Library/dynamic.aspx?id=1322 [Google Scholar]
[14]. Baker SP, O’Neill B, Haddon W, Long WB, The injury severity score: a method for describing patients with multiple injuries and evaluating emergency careJ Trauma 1974 14(3):187-96.10.1097/00005373-197403000-000014814394 [Google Scholar] [CrossRef] [PubMed]
[15]. Santos R, Abdominal Trauma Data Trauma Registry 2017 Melbourne: The Royal Melbourne Hospital (available at https://www.thermh.org.au) [Google Scholar]
[16]. Committee on Trauma, American College of Surgeons: National Trauma Data Bank annual report 2009 2009 ChicagoAmerican College of Surgeons [Google Scholar]
[17]. Sauaia A, Moore FA, Moore EE, Moser KS, Brennan R, Read RA, Epidemiology of trauma deaths: a reassessmentJ Trauma 1995 38(2):185-93.10.1097/00005373-199502000-000067869433 [Google Scholar] [CrossRef] [PubMed]
[18]. Liu PP, Liu HT, Hsieh TM, Huang CY, Ko SF, Nonsurgical management of delayed splenic rupture after blunt traumaJ Trauma Acute Care Surg 2012 72(4):1019-23.10.1097/TA.0b013e3182464c9e22491620 [Google Scholar] [CrossRef] [PubMed]
[19]. Branco BC, Tang BC, Rhee P, Fraga GP, Nascimento B, Rizoli S, Selective nonoperative management of high grade splenic traumaRev Col Bras Cir 2013 40(3):246-50.10.1590/S0100-6991201300030001523912375 [Google Scholar] [CrossRef] [PubMed]
[20]. Lutz N, Mahboubi S, Nance ML, Stafford PW, The significance of contrast blush on computed tomography in children with splenic injuriesJ Paediatr Surg 2004 39(3):491-94.10.1016/j.jpedsurg.2003.11.04215017576 [Google Scholar] [CrossRef] [PubMed]
[21]. Kao LS, Bulger EM, Parks DL, Byrd GF, Jurkovich GJ, Predictors of morbidity after traumatic pancreatic injuryJ Trauma 2003 55(5):898-905.10.1097/01.TA.0000090755.07769.4C14608163 [Google Scholar] [CrossRef] [PubMed]
[22]. Mohapatra S, Pattanayak SP, Rao KRRM, Bastia B, Options in the management of solid visceral injuries from blunt abdominal traumaIndian J Surg 2003 65:263-68. [Google Scholar]
[23]. Sosa JL, Baker M, Puente I, Sims D, Sleeman D, Ginzburg E, Negative laparotomy in abdominal gunshot wounds: a potential impact of laparoscopyJ Trauma. 1995 38:194-97.10.1097/00005373-199502000-000077869434 [Google Scholar] [CrossRef] [PubMed]
[24]. Schnuriger B, Lam L, Inaba K, Kobayashi L, Barbarino R, Demetriades D, Negative laparotomy in trauma: are we getting better?Am Surg 2012 78(2):1219-23. [Google Scholar]
[25]. Renz BM, Feliciano DV, The length of hospital stay after an unnecessary laparotomy for trauma: a prospective studyJ Trauma 1996 40(11):187-90.10.1097/00005373-199602000-000028637063 [Google Scholar] [CrossRef] [PubMed]
[26]. Renz BM, Feliciano DV, Unnecessary laparotomies for trauma: a prospective study of morbidityJ Trauma 1995 38:350-56.10.1097/00005373-199503000-000077897713 [Google Scholar] [CrossRef] [PubMed]
[27]. Gaspar B, Negoi I, Paun S, Hostiuc S, Ganescu R, Beuran M, Selective nonoperative management of abdominal injuries in polytrauma patients: a protocol only for experienced trauma centersMaedica (Buchar) 2014 9(2):168-72. [Google Scholar]