Introduction
For many women with breast cancer, mastectomy is a common form of treatment which has an indirect effect on female beauty, sexuality and feminity. Also, the patients suffer severe arm and shoulder morbidity post surgery which affects their quality of life.
Aim
To determine the arm function and quality of life among patients after mastectomy and find correlation between these two aspects.
Materials and Methods
A quantitative descriptive correlational design with non probability convenience sampling technique was used to collect data from 60 post mastectomy women. The setting used for the study was Gynaecological Oncology OPD at Amrita Institute of Medical Sciences (AIMS), Kochi, Kerala, India. Data collection was done from November 2016 to December 2016. A standardised Quality of Life-Breast Cancer Patient Version (QOL-BCV) questionnaire and DASH (Disability of Arm Shoulder Hand) tool was used for the assessment along with a structured questionnaire to assess sociodemographic and clinical data. Karl Pearson correlation test was used for data analysis.
Results
The study result showed that majority of the patients 48 (80%) had good arm function with less disability. Quality of life of 21 (35%) patients was high and 39 (65%) patients had moderate quality of life. There was a significant correlation found between disability score and quality of life (r=-0.802) and with all the domains of quality of life {physical (r=-0.771), psychological (r=-0.695), social (r=-0.746) and spiritual (r=-0.500)}. Also a significant association was found between arm function and the clinical variables like oedema (p=0.006) and radiation therapy (p=0.017).
Conclusion
Arm disability influences quality of life of patients after mastectomy. The results of this study will help to improve actions to reduce arm disabilities such as lymphoedema as early as possible, through proper assessment and post mastectomy exercises, including special care for patients undergoing radiation therapy. This will improve the quality of life of post mastectomy patients.
Introduction
Breast cancer is one of the most common malignancies affecting women worldwide, both in the developed and less developing countries [1]. Because of its well publicised nature, and potential for lethality, breast cancer is arguably the most frightening type of cancer diagnosis, someone can receive [2]. Breast cancer ranks as the fifth cause of death from cancer overall (5,22,000 deaths) and while it is the most frequent cause of cancer death in women in less developed regions (3,24,000 deaths, 14.3% of total), it is now the second cause of cancer death in more developed regions (1,98,000 deaths, 15.4%) after lung cancer [3].
In Kerala, breast cancer has taken the lead over carcinoma cervix to become the number one malignancy in the women. According to the data available at Trivandrum Cancer Registry, in 2012, the prevalence rate of breast cancer in rural area is 19.8 per one lakh while in the urban areas it is 30.5 per one lakh. According to the latest data available at AIMS, 970 cases of breast cancer were reported including male and female during the year 2013-2014 and 422 (92.3%) patients underwent surgery [4].
During the post mastectomy period, various problems are experienced by women which include limitation of shoulder motion, oedematous arm, numbness of chest wall and arm and depression [1]. Patients who have been treated for breast cancer may be at risk for arm swelling called lymphoedema. It is one of the most common complications that occur after mastectomy which can badly affect the arm function [5]. Lymphoedema following breast cancer surgery is caused by mechanical lesion of the lymphatic system, protein accumulates in the tissues causing fibrosclerosis.
Lymphoedema can lead to severe arm morbidity, which could have a long term effect on the quality of life of patients with breast cancer [6]. Also, breast cancer affects woman identities and therefore studying quality of life in women who lose their breasts is vital. The quality of life is a multidimensional term, which consists of different domains such as physical and social functioning and psychological well being. Although, investigating quality of life as an outcome is challenging because it involves complex, inter-related factors and it is subjective over a year.
Various related studies conducted on this topic shows that radical mastectomy has an influence on the extent of functional limitation, linked to the presence of the lymphoedema. Also, a statistically significant correlation was observed in these studies, between the DASH score and health related quality of life [7-9].
Therefore, evaluating the impact on quality of life is very important. Thus, the present study was conducted to assess the arm function and quality of life in the women after mastectomy and also to find corelation between these two.
Materials and Methods
The descriptive correlational study was conducted in 60 women aged between 30 years and above whose post mastectomy period was from six weeks onwards. Sample size was calculated based on the prevalence of breast cancer in Kerala population [10]. The study was conducted in Gynaecological Oncology OPD in a multispecialty hospital, Kochi, Kerala, India. Data collection was done from November 2016 to December 2016. The subjects were selected by non probability convenience sampling technique. The data were collected using structured questionnaire.
The following tools were used for the study. Tool I was a structured questionnaire to assess the sociodemographic and clinical variables, which had two sections. Section A sociodemographic data and section B clinical data. Tool II was DASH Questionnaire developed by American Academy of Orthopedic Surgeons and a team at the institute for work and health, which had 30 items to assess the arm function [11]. Tool III was QOL-BCV developed by researchers at the City of Hope National Medical Center, which has 46 items to measure the quality of life [12]. Both tools were freely available. Prior to the commencement of the study, approval was obtained from the Research Committee and institutional ethical committee. After establishing rapport with the subjects, an informed consent was taken prior to data collection explaining the importance of study and the data collection procedure. 60 subjects who met the inclusion criteria were taken. Inclusion criteria for the present study was, all breast cancer patients who underwent mastectomy six weeks and above and those who are willing to participate in the study. Exclusion criteria was patients who are critically ill. The researcher collected some of the clinical data from patient’s record.
Statistical Analysis
The collected data was analysed using descriptive and inferential statistics. The description of sample characteristics based on sociodemographic and clinical variables were computed using descriptive statistics. Pearson’s correlation test was used to find the correlation between arm function and quality of life among patients after mastectomy (p≤0.001).
Results
The study result showed that the majority of subjects 35 (58.3%) were in the age group of 51-70 years. Most of the subjects 59 (98.3%) were married and they 40 (66.7%) belongs to Hindu religion. Other variables are given in the [Table/Fig-1]. Most of the subjects 41 (28%) were treated on the non dominant side [Table/Fig-2]. All the subjects 60 (100%) who underwent surgery had their sentinel lymph nodes removed.
Demographic and clinical variables.
| Demographic variables | Frequency | Percentage (%) |
|---|
| Educational status |
| Illiterate | 2 | 3.3 |
| Primary | 22 | 36.7 |
| Secondary | 16 | 26.7 |
| Higher secondary | 16 | 26.7 |
| Graduate | 2 | 3.3 |
| Postgraduate | 2 | 3.3 |
| Occupation |
| Government employee | 3 | 5.0 |
| Private employee | 6 | 10.0 |
| Daily wages | 1 | 1.7 |
| Unemployed | 50 | 83.3 |
| Monthly family income (based on Kuppuswamy scale) |
| Above Rs. 41,130 | 2 | 3.3 |
| Rs. 20,715-41,429 | 8 | 13.3 |
| Rs. 15,536-20,714 | 15 | 25 |
| Rs. 10,357-15,535 | 32 | 53.33 |
| Rs. 6,214-10,356 | 3 | 5 |
| Rs. 2,092-6,213 | 0 | 0 |
| Below Rs. 2091 | 0 | 0 |
| Clinical variables |
| BMI | | |
| Under weight | 2 | 3.3 |
| Normal | 28 | 46.7 |
| Over weight | 17 | 28.3 |
| Obese | 13 | 21.7 |
| Time since diagnosis |
| <2 Years | 51 | 85.0 |
| 2-4 Years | 4 | 6.7 |
| 4-6 Years | 3 | 5.0 |
| >6 Years | 2 | 3.3 |
| Time since surgery |
| <1 Years | 51 | 85.0 |
| 1-3 Years | 3 | 5.0 |
| 4-6 Years | 4 | 6.7 |
| >6 Years | 2 | 3.3 |
| Chemotherapy | 60 | 100 |
| Radiation therapy | 21 | 35 |
| Lymphoedema | 3 | 5 |
Distribution of subjects based on DASH score and quality of life.
| Distribution of subjects | Frequency | Percentage (%) | Mean | SD |
|---|
| DASH score |
| Low | 48 | 80.0 | 23.38 | 16.08 |
| Moderate | 11 | 18.3 |
| High | 1 | 1.66 |
| Quality of Life |
| Moderate | 39 | 65.0 | 284.3 | 48.06 |
| High | 21 | 35.0 |
| Sub domains of Quality of Life |
| Physical |
| Moderate | 19 | 31.6 | 57.98 | 10.29 |
| High | 41 | 68.3 |
| Psychological |
| Low | 1 | 1.6 | 118.0 | 25.58 |
| Moderate | 53 | 88.3 |
| High | 6 | 10 |
| Social |
| Low | 1 | 1.6 | 57.37 | 12.67 |
| Moderate | 30 | 50 |
| High | 29 | 48.3 |
| Spiritual |
| Moderate | 12 | 20 | 50.93 | 6.709 |
| High | 48 | 80 |
SD: Standard deviation
The subjects were distributed based on the score obtained in the questionnaires. The minimum and maximum DASH score is 0 and 100 respectively. Therefore, the subjects were distributed as low score 0-33, moderate score 34-67, and high score 68-100. Similarly, minimum and maximum score in QOL scale was 0 and 460 respectively and the scores were divided into 3 equal parts as low, moderate and high. The same method was followed for QOL subdomains. The study results shows that 48 (80.0%) subjects have low DASH score. The mean arm function score was 23.38 with standard deviation 16.08. The minimum and maximum arm function score was 4 and 85 respectively. Almost 39 (65%) of the subjects have moderate quality of life and 35% have high quality of life. The mean quality of life score was 284.3 with standard deviation of 48.06. The minimum and maximum quality of life score was 178 and 416 respectively [Table/Fig-2].
There was a significant negative correlation between DASH score and quality of life (r=-0.802). Low DASH score indicates high arm function with less disability. It concludes that quality of life increases when the arm function is good [Table/Fig-3].
Scatter plot showing correlation between arm function and quality of life.
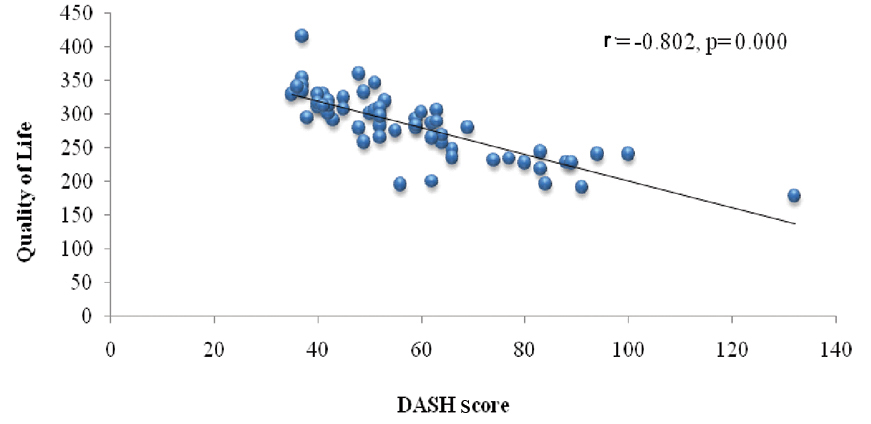
Also, a significant correlation was found between all the domains of quality of life. Physical (r=-0.771), psychological (r=-0.695), social (r=-0.746) and spiritual (r=-0.500). A significant association was observed between presence of oedema (p-value=0.006, significant at 0.05 level) and radiation treatment taken (p-value=0.017, significant at 0.01 level) [Table/Fig-4].
Association of arm function with quality of life.
| Clinical data | DASH | p-value |
|---|
| Low (n=48) | Medium (n=12) |
|---|
| BMI |
| Under weight | 2 (100.0%) | 0 (0.0%) | 0.898 (ns) |
| Normal | 23 (82.1%) | 5 (17.9%) |
| Over weight | 13 (76.5%) | 4 (23.5%) |
| Obese | 10 (76.9%) | 3 (23.1%) |
| Time since diagnosis |
| <2 Years | 42 (82.4%) | 9 (17.6%) | 0.236 (ns) |
| 2-4 Years | 2 (50.0%) | 2 (50.0%) |
| 4-6 Years | 2 (66.7%) | 1 (33.3%) |
| >6 Years | 2 (100.0%) | 0 (0.0%) |
| Time since surgery |
| <1 Years | 41 (80.4%) | 10 (19.6%) | 0.398 (ns) |
| 1-3 Years | 3 (100.0%) | 0 (0.0%) |
| 4-6 Years | 2 (50.0%) | 2 (50.0%) |
| >6 Years | 2 (100.0%) | 0 (0.0%) |
| Radiation |
| Yes | 13 (61.9%) | 8 (38.1%) | 0.017* |
| No | 35 (89.7%) | 4 (10.3%) |
| Oedema |
| Yes | 0 (0.0%) | 3 (100.0%) | 0.006** |
| No | 48 (84.2%) | 9 (15.8%) |
| Side of treatment |
| Dominant side | 14 (73.7%) | 5 (26.3%) | 0.493 (ns) |
| Non dominant side | 34 (82.9%) | 7 (17.1%) |
** Association is significant at 0.01 level; *Association is significant at 0.05 level; ns: Association is not significant
Discussion
The first objective of the study was to determine the arm function among patients after mastectomy. The study result showed that majority of subjects 48 (80.0%) had low DASH score. There by disability is less among them. This shows that their arm function was good. Only one subject (1.66%) had high DASH score which indicates poor arm function.
The study findings were supported by a correlational study conducted by Smoot B et al., at San Francisco among 148 breast cancer survivors to identify the upper extremity impairments in women with and without lymphoedema [13]. The study results shows that women with lymphoedema had high DASH score and had greater upper extremity impairment and limitation in activities than women without (p<0.001) [14]. In the present study, only three (5%) subjects had lymphoedema. It is believed to be one of the 3reasons for having good arm function (DASH score low in 80% of subjects).
In the present study, majority of the subjects 39 (65%) had not undergone radiation therapy. This gives the reason for good arm function among patients after mastectomy in the current study. Also, various study results shows that post mastectomy exercises decrease the incidence of arm oedema after mastectomy. And in the current setting all patients were performing post mastectomy exercises.
The second objective of the study was to determine the quality of life of patients after mastectomy. The present study shows that 39 (65%) subjects had moderate quality of life and 21 (35%) subjects had high quality of life. While considering the sub domains of quality of life it was found that in the psychological domain only few 6 (10%) subjects had high score and majority 53 (88.3%) of the subjects had moderate psychological well being.
A study by Tobin MB et al., in London with 50 patients reveals that patients with oedema due to axillary lymph node dissection had more psychosocial and adaptation problems than a comparable group of patients without oedema. Patients with arm swelling in relation to breast cancer experienced functional impairment, psychosocial maladjustment, and increased (p≤0.001) psychological morbidity that affected the quality of life. This study supports the above findings [14].
The third objective of the study was to find correlation between the arm function and quality of life. In the present study, the result shows that there is a strong negative correlation between DASH score and quality of life (r=-0.802) and also with the sub domains of quality of life. Since, high DASH score indicates poor arm function, quality of life decreases when arm function is poor and quality of life increases when the arm function is good. The results of the present study and the previous studies reviewed revealed that there is a significant correlation found between DASH score and quality of life [15].
Limitation
The present study has some limitations as it was conducted in a single setting which reduces the generalisability of the findings in larger population.
Conclusion
The study results brings into a conclusion that arm function is a major aspect that affects the quality of life of women after mastectomy. Also, presence of oedema and radiation therapy contributes more to this issue. The results of this study will help in prevention and early detection of lymphoedema which will help to improve the quality of life of post mastectomy patients. Hence, this study depicts the need and importance of assessment of arm function in patients after mastectomy and also it depicts the importance of post mastectomy exercises to prevent lymphoedema.
SD: Standard deviation
** Association is significant at 0.01 level;
*Association is significant at 0.05 level; ns: Association is not significant
[1]. Fann J, Thomas AM, Katon WJ, Cowley D, Pepping M, McGregor BA, Major depression after breast cancer- a review of epidemiology and treatmentGan Hosp Psychiatry 2008 30(2):112-26.10.1016/j.genhosppsych.2007.10.00818291293 [Google Scholar] [CrossRef] [PubMed]
[2]. Gerber LH, A review of measures of lymphedemaCancer 1998 83(12):2803-804.10.1002/(SICI)1097-0142(19981215)83:12B+<2803::AID-CNCR29>3.0.CO;2-W [Google Scholar] [CrossRef]
[3]. http://globocan.iarc.fr/old/FactSheets/cancers/breast-new.asp [Google Scholar]
[4]. Hospital cancer registry 2013-2014Amrita Inst of Medical Sciences, Kochi 2016 :104-106. [Google Scholar]
[5]. Pinto M, Gimigliano F, Tatangelo F, Megna M, Izzo F, Gimigliano R, Upper limb function and quality of life in breast cancer related lymphedema: A cross-sectional studyEur J Phys Rehabil Med 2013 49(5):665-73. [Google Scholar]
[6]. Weissleder H, Schuchhardt C, Bocking M, Lymphedema-diagnosis and therapy verlag 3rd ed Viavital Verlag, Kğln 2001 [Google Scholar]
[7]. Brennan MJ, Lymphedema following surgical treatment of breast cancer. a review of pathophysiology and treatmentJ Pain Symptom Manage 1992 7(2):11010.1016/0885-3924(92)90122-X [Google Scholar] [CrossRef]
[8]. Márcia R, Angela G, Luis A, Ferrigno I, Late morbidity in upper limb function and quality of life in women after breast cancer surgeryBraz J Phys Ther 2013 17(3)10.1590/S1413-3555201200500008823966141 [Google Scholar] [CrossRef] [PubMed]
[9]. Manandhar S, Shrestha DS, Taechaboonsermsk P, Siri S, PiSuparpnkham J, Quality of life among breast cancer patients undergoing treatment in national cancer centers in NepalAsian Pac J Cancer Prev 2014 15(22):9753-57.10.7314/APJCP.2014.15.22.975325520099 [Google Scholar] [CrossRef] [PubMed]
[10]. Jayalekshmi AP, Sebastian P, Burden of Cancers - Registry based data from Kerala, IndiaJournal of Health Systems 2016 2(1):3-7. [Google Scholar]
[11]. The Institute for Work & Health. DASH outcome measures. Available from: https://www.myoptumhealthphysicalhealth.com/Documents/Forms/DASH.pdf [Google Scholar]
[12]. Ferrell B.R, Dow K.H., Grant M, Quality of Life Instrument - Breast Cancer Patient Version (QOL-BC) 2012 Available from: http://www.midss.org/content/quality-life-instrument-breast-cancer-patient-version-qolbc [Google Scholar]
[13]. Smoot B, Wong J, Cooper B, Wanek L, Topp K, Byl N, Upper extremity impairments in women with or without lymphedema following breast cancer treatmentJ Cancer Surviv 2010 4(2):167-78.10.1007/s11764-010-0118-x20373044 [Google Scholar] [CrossRef] [PubMed]
[14]. Tobin MB, Lacey HJ, Meyer L, Mortimer PS, The psychological morbidity of breast cancer-related arm swellingTetracyclineTeratology 1993 72(11):3248-52.10.1002/1097-0142(19931201)72:11<3248::AID-CNCR2820721119>3.0.CO;2-Z [Google Scholar] [CrossRef]
[15]. Sreedevi A, Cherkil S, Kuttikattu DS, Kamalamma L, Oldenburg Brian. Validation of WHOQOL-BREF in Malayalam and determinants of quality of life among People with Type 2 diabetes in Kerala, IndiaAsia Pac J Public Health 2016 28:62S-69S.10.1177/101053951560588826419636 [Google Scholar] [CrossRef] [PubMed]