Introduction
Various biologic and non biologic graft materials are considered in the past as Intraoral wound dressing material. While autografts have issues related to donor site morbidity, allografts like collagen have limited intraoral usage due to allergenicity and ease of adaptability to the mucosal defect. Bismuth sub-nitrate Iodoform Paraffin Paste (BIPP) dressing is prepared by impregnating sterile gauze with a paste containing one part bismuth sub-nitrate, two parts iodoform, one part sterile liquid paraffin by weight. BIPP is well known for its antiseptic and astringent properties, henceforth serves as a good wound dressing material preventing infection and wound contractures. Its use in intraoral mucosal defects though widely acknowledged has rarely been evaluated.
Aim
The aim of this study was to assess the qualitative properties of BIPPs as an intraoral wound dressing material.
Materials and Methods
A total of 10 patients with oral precancerous lesions of the oral mucosa were included in this study. After excision of the oral lesions, BIPP pack was used to cover the defects that were too large to close primarily. Before use, sterile BIPP gauze was cut into a suitable shape of the defect and was placed directly on the wound and stabilised using vicryl sutures. The dressing was removed after two weeks of the operation. The effectiveness and usefulness of the BIPP dressing was evaluated by scoring the following parameters in the intraoperative and postoperative periods: operability, haemostatic status, pain relief, feeding situation, epithelialisation, scar contracture, and safety.
Results
Out of the 10 patients, in six patients BIPP was used for the buccal mucosal defect, in two patients for labial mucosal defect and in one patient each for tongue and palatal defect. In all the patients the raw wound post resection were covered with BIPP pack and stabilised with vicryl sutures. Postoperatively there was no adverse event, there was no discomfort and all the patients tolerated the BIPP dressing.
Conclusion
BIPP use in covering the defect, post soft tissue resection of the intraoral precancerous lesion has given a satisfactory result in the present study.
Collagen dressing, Mucosal allograft substitutes, Precancerous conditions
Introduction
Research has proven that the concept of an optimum environment for wound repair aids in better healing and reduction in wound contracture. Biocompatible wound dressing helps in establishing and maintaining such an optimal environment [1]. A variety of dressing materials have been used in the past, based upon the suitability, to treat denuded areas and surgical defects and as temporary or permanent cover after burns [2]. Various biologic and non biologic graft materials are considered in the past as wound dressing material. However, biological graft in the form of autograft always has the issues related to the donor site morbidity and often lack in providing suitable environment mimicking that of the oral mucosa [3]. Allografts in the form of collagen have been used however reactivity/allergenicity of the material and adaptability of the graft with the wound bed is the main guarding factor limiting their use [1]. BIPP dressing is prepared by impregnating sterile gauze with a paste containing one part bismuth sub-nitrate, two parts iodoform, one part sterile liquid paraffin by weight. James Morrison Rutherford (Professor of Surgery, Durham) was the first to use BIPP for world war soldier’s wounds [4,5]. BIPP acts as astringent and antiseptic agent at the wound site thus controlling infection and subsequent scarring. BIPP impregnated ribbon gauze, is extensively used by ENT surgeons for packing the nasal cavity for control of epistaxis [6] and packing surgical defects of the jaws as well as post mastoidectomy defects for promoting healing by secondary intention [2,7]. There has always been a need to provide a suitable healing environment for mucosal defects and both allograft and autograft used in the past have their individual pros and cons. Henceforth, this study was designed to assess the qualitative properties of BIPP as intraoral wound dressing material and to substantiate and propose the usefulness of BIPP dressing in covering the oral surgical mucosal defect.
Materials and Methods
A retrospective study of patients reporting to the Department of Dental and Oral Surgery, Christian Medical College and Hospital, Vellore, Tamil Nadu, India between January 2015-December 2016 with precancerous lesion of the oral cavity and who underwent excisional biopsy with intraoral BIPP pack dressing, was conducted from the patients records saved in electronic database. Only patients who had biopsy proven dysplastic lesion or lesion with premalignant features and those who underwent excision with BIPP pack dressing were included in the study. Biopsy proven malignancies were excluded from the study. After excision of the oral lesions, BIPP pack was used to cover the defects that were too large to close primarily. Before use, sterile BIPP gauze was cut into a suitable shape of the defect and was placed directly on the wound and stabilised using vicryl sutures. Suturing was done in interrupted fashion around the margin of the defect to the BIPP dressing. The BIPP pack was prepared as follows; sterile gauze was impregnated with paste of bismuth sub nitrate (one part by weight), iodoform (two parts by weight), and sterile liquid paraffin (one part by weight). The dressing was removed after two weeks of surgery. All the patients were reviewed after one and two months postoperatively to assess the healing. Records of 10 patients with precancerous lesions of the oral mucosa were evaluated from the database and wound site and size were documented. The effectiveness and usefulness of the BIPP dressing was evaluated during the intraoperative and postoperative periods. The intraoperative parameters included operability and haemostatic status. Postoperative parameters included pain relief, diet, epithelialisation, scar contracture, and reactivity. These parameters were documented from the details in the patient’s record. The scoring pattern for the BIPP dressing was determined by referring to the criteria described by Rastogi S et al., Bessho K and Murakami K, and Arai N et al., [3,8,9]. The result of each parameter was judged as good (2 points), fair (1 point), or poor (0 point). The criteria for the judgment in this study are presented in [Table/Fig-1].
Criteria for judgment of BIPP pack.
| Score | Definition |
|---|
| Operability |
| Good | easy to use |
| Fair | acceptable |
| Poor | impractical |
| Hemostatic status |
| Good | no bleeding |
| Fair | no hemostasis required/slight bleeding |
| Poor | bleeding that required hemostasis |
| Pain relief |
| Good | none to mild |
| Fair | slight to moderate |
| Poor | severe |
| Feeding |
| Good | oral feeding, normal diet within 2 week |
| Fair | oral feeding, normal diet within 4 week |
| Poor | combination of tube diet |
| Mucosalisation |
| Good | entire wound |
| Fair | nearly entire wound |
| Poor | inadequate |
| Scar contracture |
| Good | None or little (0-25%) |
| Fair | Slight (26-50%) |
| Poor | Serious (>50%) |
| Reactivity |
| Good | no adverse effect |
| Poor | any adverse events |
| Usefulness |
| Very useful | 11-14 points, no adverse events |
| Useful | 7-10 points, no adverse events |
| Useless | 0-6 points |
Score: [Good-2; Fair-1; Poor-0]
Operability-of the BIPP dressing was evaluated based on the operators’ impressions on the handling properties in cutting and shaping and adherence to the wound surface.
Haemostatic status was assessed intraoperatively. An absence of bleeding was categorised as good, mild bleeding such as oozing was categorised as fair, and bleeding that required haemostatic intervention or re-exploration was categorised as poor.
Pain relief- was categorised based on the patients’ subjective signs as good (none to mild), fair (slight to moderate), or poor (severe).
Diet- was soft to normal during postoperative period. It was rated as good (throughout the postoperative course oral feeding is continued, normal diet started within two weeks after surgery), fair (throughout the postoperative course oral feeding is continued, normal diet started within two weeks), or poor (nasogastric tube diet required, or normal diet started later than two weeks).
Epithelialisation- was rated at one month postoperative as good (entire wound), fair (almost the entire wound), or poor (insufficient).
Scar contracture-of the wound was assessed at two months after surgery and categorised as good (none or little), fair (50%), or poor (>50%). This was evaluated by comparing the degree of mouth opening before and after the operation.
The effectiveness of the BIPP pack was judged by the total scores of these six parameters. A score of 10 to 12 was considered very effective, 7 to 9 effective, and 0 to 6 ineffective. The reactivity of membrane was assessed as good (2 points) or poor (0 point), depending on the absence or presence of an allergenic reaction and wound infection after placing the pack at the site of the defect. When there were no signs of tissue reaction and infection, it was judged good. Otherwise, it was considered poor.
The usefulness of the material was evaluated by adding the effectiveness and safety scores; 11 to 14 points was rated very useful, 7 to 10 points as useful, and 0 to 6 points as useless.
Results
A total of 10 patients were included in the study between the age range of 48 years to 62 years, only two patient having buccal mucosal defect were females and rest of the patients were males. Six patients had defect on the buccal mucosa, two patients had defect on the labial mucosa and one patient each had the defect over the tongue and palate. The size of surgical defect in the oral subsites varied from 1.5 cm×1.5 cm at the labial mucosa (minimum) to 3.5 cm×4 cm at the buccal mucosa (maximum). Operability of the BIPP dressing pack was good with overall score of 2. Haemostasis was achieved intraoperatively with none of the case showing any event of postoperative bleeding. One patient with tongue defect had a pain score of severe (0), rest of the patients had mild to moderate pain postoperatively, however all the patients were managed with analgesics effectively. Diet was not affected either and most of the patients took semi-solid diet postoperatively and normal diet was encouraged after second week following initial mucosalisation. There was acceptable scarring with adequate mouth opening in all the case. The effectiveness score was found to be between 7 to 11 (effective). No tissue reactivity to the BIPPS was noted. Eight out of ten patients had overall score between 11-13 (very useful). In one patient scarring was found to be more in the labial mucosal site presenting with decreased mouth opening with overall score of 10 (useful). One other patient had suboptimal mucosalisation at the labial mucosal site and had an overall score of 10 (useful), however rest all the patient eventually showed more than 50% mucosalisation in four weeks. Henceforth BIPP dressing was found to be effective and very useful overall [Table/Fig-2].
Results obtained in each case.
| Case | Age | Sex | Site | Size (mm approx.) | Operability | Haemostasis | Pain | Feed | Mucosalisation | Scar | Reactivity/allergy | Total | Usefulness |
|---|
| 1. | 52 | M | bm | 25×30 | 2 | 2 | 1 | 1 | 1 | 2 | 2 | 11 | Very useful |
| 2. | 49 | M | bm | 15×25 | 2 | 2 | 1 | 2 | 1 | 1 | 2 | 11 | Very useful |
| 3. | 59 | M | t | 30×30 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 12 | Very useful |
| 4. | 56 | F | bm | 25×30 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 13 | Very useful |
| 5. | 62 | M | bm | 35×40 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 13 | Very useful |
| 6. | 46 | F | bm | 35×35 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 13 | Very useful |
| 7. | 51 | M | p | 30×30 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 13 | Very useful |
| 8. | 59 | M | lm | 15×15 | 2 | 2 | 1 | 1 | 1 | 1 | 2 | 10 | useful |
| 9. | 48 | M | lm | 20×15 | 2 | 2 | 2 | 1 | 0 | 1 | 2 | 10 | useful |
| 10 | 52 | M | bm | 30×30 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 13 | Very useful |
Discussion
An open wound is prone to infection, scarring and contraction, along with various other clinical complications. Raw wounds of the oral cavity, like any other wound, heal by epithelialisation and granulation [10,11]. However, in the oral cavity the healing of raw wounds presents special problems. The oral environment is always moist with contamination from salivary secretion and food ingestion henceforth the risk of infection in the oral cavity is quite high, which may result in scarring and contraction [12]. Poor oral hygiene along with constant masticatory forces resulting in movement of the cheek and tongue interferes with graft adherence and acceptance hence causing residual scarring, which undergoes ulceration and act as a constant source of irritation [13]. The fact that grafted wounds heal faster with fewer complications than open wounds has been recognised in general surgery for almost a century.
Mucosal grafts are the best option because they fulfil the requirements necessary for an ideal graft material, with its ability to replace lost structures as well as inducing the formation of mucosal tissues. There is, always limited quantity of oral mucosa for grafting, and thicker texture of mucosa taken from the cheek often results in scarring. Henceforth there is always a degree of donor-site morbidity present. Skin graft is the next solution, but such graft used in the mouth will always retain the colouration of the skin and never attain the texture or the resiliency of the oral mucosa. Also seen is the growth of adnexal structures such as hair and sweat glands are also seen. In elderly persons the skin is atrophic and inelastic, making it unsuitable [14,15].
In past several material has been tried including dermis, [8] amniotic membrane, [9] and collagen [10] but none has outweighed and still disparity exists. BIPP pack has been in use for long especially for packing the maxillary defect and for antral and nasal packing. The initial healing takes place under the BIPP as the raw surface gets covered with slough and is later replaced by granulation tissue and the defect gets mucosalised subsequently. As seen in all the cases, [Table/Fig-3,4,5,6, and 7] the BIPP acts as an adequate intraoral dressing material, as none of the patients developed any allergenicity as seen with allograft materials. The adaptability of the gauze impregnated with BIPP is also adequate and patient compliance post surgery is acceptable. None of the patient had complaint of discomfort or severe pain following the dressing with BIPP. Oral hygiene maintenance as well as feeding did not get affected with the dressing in place. After initial mucosalisation, in two weeks the BIPP was removed and the wound site was left for complete mucosalisation that takes place by four weeks. Though BIPP has shown promising results in current study further comparative study with other allografts and a larger sample size needs to be considered.
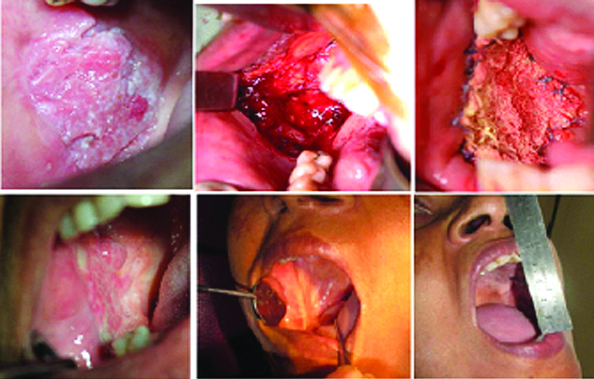
a) Premalignant lesion of buccal mucosa; b) Excised mucosal defect; c) BIPP in place; d) Immediate post removal of BIPP dressing; e) Postoperative review after 2 months; f) Mouth opening after 2 months.
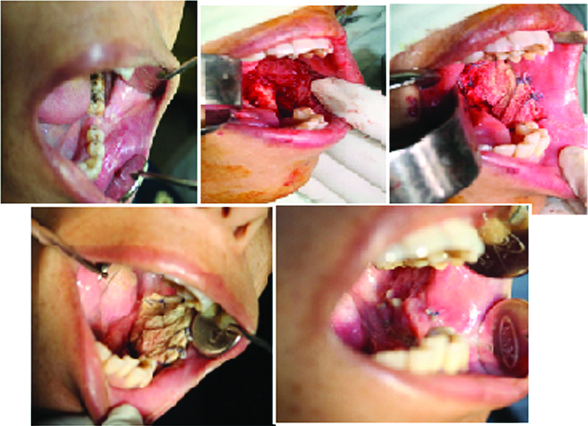
a) Premalignant lesion over the labial mucosa; b) Intraoperative BIPP dressing in place; c) Postoperative 2 months healing.

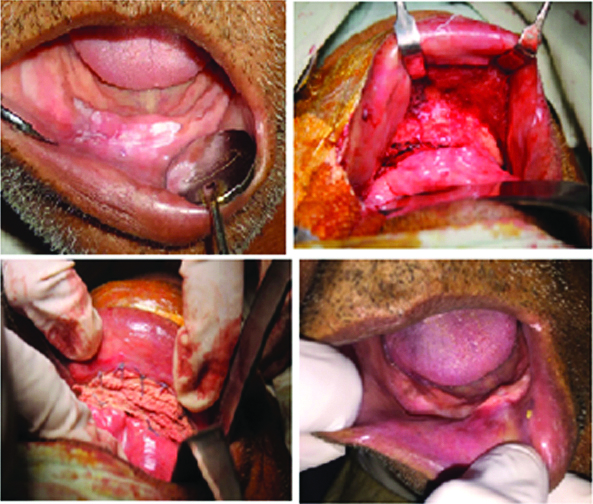
a) Premalignant lesion on the tongue; b) Excised lesion; c) BIPP dressing sutured across the defect with 3-0 vicryl; d) Two week postoperative mucosalisation after BIPP removal.

a) Premalignant lesion of the left side buccal mucosa and gingivo-buccal sulcus; b) Intraoperative defect at the excision site; c) Intraoperative BIPP in place; d) 1 week postoperative BIPP in place; e) 2 weeks postoperative at time of BIPP removal showing normal healing.
a) premalignant lesion over the labial mucosa and anterior gingivobuccal sulcus; b) Intraoperative excision defect; c) Defect site covered with BIPP pack; d) 2 months follow-up shows normal healing.
Conclusion
Bismuth sub-nitrate iodoform paraffin paste has the adequate features required for its use as an intraoral wound dressing material. BIPP does not initiate or promote wound healing however, provides an adequate environment for the healing to take place. It has advantage over other autografts in avoiding donor site morbidity, its easy adaptability to the wound site and patient compliance makes it one of the favoured wound dressing material for intraoral defect sites.
Score: [Good-2; Fair-1; Poor-0]
[1]. Abbenhaus JL, MacMahon RA, Rosenkrantz JG, Collagen sheets as a dressing for large excised areasSurg Forum 1965 16:477 [Google Scholar]
[2]. Freedman M, Stassen LF, Commonly used topical oral wound dressing materials in dental and surgical practice-a literature reviewJ Ir Dent Assoc 2013 59:190-95. [Google Scholar]
[3]. Rastogi S, Modi S, Sathian B, The efficacy of collagen membrane as a biodegradable wound dressing material for surgical defects of oral mucosa: A prospective studyJ Oral Maxillofac Surg 2009 67:1600-06.10.1016/j.joms.2008.12.02019615570 [Google Scholar] [CrossRef] [PubMed]
[4]. Chevretton EB, McRae RD, Booth JB, Mastoidectomy packs Xerofoam or BIPP?The Journal of Laryngology and Otology 1991 105:916-17.10.1017/S00222151001178031842220 [Google Scholar] [CrossRef] [PubMed]
[5]. Sharma RR, Cast IP, Redfern RM, O’Brien C, Extradual application of BIPP paste causing Bismuth encephalopathy a case reportJournal of Neuro and Neurosurgery. 1994 57:990-93.10.1136/jnnp.57.8.9908057127 [Google Scholar] [CrossRef] [PubMed]
[6]. Gurd FB, Laurie H, McKim LH, The use of B.I.P.P. and liquid paraffin in the treatment of woundsAmerican Journal of Surgery 2011 51:584-600.10.1016/S0002-9610(41)90197-6 [Google Scholar] [CrossRef]
[7]. Chacko R, Kumar S, Paul A, Arvind. Spontaneous bone regeneration after enucleation of large jaw cystsJournal of Clinical and Diagnostic Research 2015 9(9):ZC84-ZC89.10.7860/JCDR/2015/13394.652426501020 [Google Scholar] [CrossRef] [PubMed]
[8]. Bessho K, Murakami K, The use of a new bilayer dermis for vestibular extensionBr J Oral Maxillofacial Surg 1998 36:457-772.10.1016/S0266-4356(98)90463-6 [Google Scholar] [CrossRef]
[9]. Arai N, Tsuno H, Okabe M, Yoshida T, Koike C, Noguchi M, Clinical application of a hyperdry amniotic membrane on surgical defects of the oral mucosaJ Oral Maxillofac Surg 2012 70:2221-28.10.1016/j.joms.2011.09.03322197005 [Google Scholar] [CrossRef] [PubMed]
[10]. Doillon EJ, Porous collagen sponge wound dressing; in vivo and in vitro studiesJ Biomaterial Appl 1988 2:562-78.10.1177/0885328287002004043058927 [Google Scholar] [CrossRef] [PubMed]
[11]. Gao ZR, Hao ZQ, Li Y, Im MJ, Spence RJ, Porcine dermal collagen as a wound dressing for skin donor sites and deep partial skin thickness burnsBurns 1992 18:492-96.10.1016/0305-4179(92)90183-U [Google Scholar] [CrossRef]
[12]. Gungormuş M, Kaya O, Evaluation of the effect of heterologous type I collagen on healing of bone defectsJ Oral Maxillofac Surg 2002 60:541-45.10.1053/joms.2002.3185211988933 [Google Scholar] [CrossRef] [PubMed]
[13]. Chung KM, Salkin LM, Stein MD, Freedman AL, Clinical evaluation of a biodegradable collagen membrane in guided tissue regenerationJ Periodontol 1990 61:732-36.10.1902/jop.1990.61.12.7322269914 [Google Scholar] [CrossRef] [PubMed]
[14]. Gupta RL, Jain RK, Kumar M, Role of collagen sheet cover in burns-A clinical studyIndian J Surgery 1978 40:646-49. [Google Scholar]
[15]. Bertolami CN, Ellis DG, Healing of cutaneous and mucosal wounds grafted with collagen-Glycosaminoglycan/silastic bilayer membranes: A preliminary reportJ Oral Maxillofacial Surg 1988 11:971-78.10.1016/0278-2391(88)90334-5 [Google Scholar] [CrossRef]