Extramedullary Plasmacytoma Presenting as Lung Cancer
Gajanan S Gaude1, Avya Bansal2
1 Professor and Head, Department of Pulmonary Medicine, Jawaharlal Nehru Medical College, Belgaum, Karnataka, India.
2 Senior Resident, Department of Pulmonary Medicine, Jawaharlal Nehru Medical College, Belgaum, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gajanan S Gaude, Professor and Head, Department of Pulmonary Medicine, Jawaharlal Nehru Medical College, Belgaum-590010, Karnataka, India.
E-mail: gsgaude922@gmail.com
Extramedullary Plasmacytoma (EMP) is a rare plasma cell tumour without any other systemic characteristics of multiple myeloma. They are commonly observed in tissues of the upper aerodigestive tract and are extremely rare tumours. Herein, we report an extremely unusual presentation of EMP as endobronchial mass without any bone involvement.
Bone marrow, Endobronchial mass, Multiple myeloma
Case Report
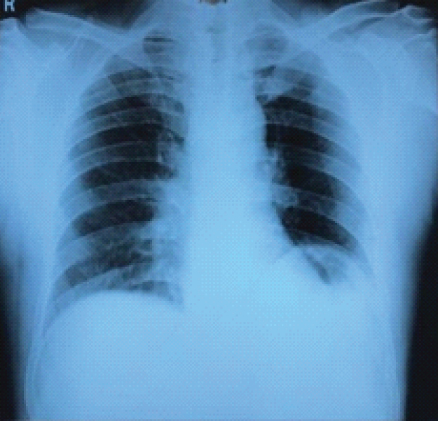
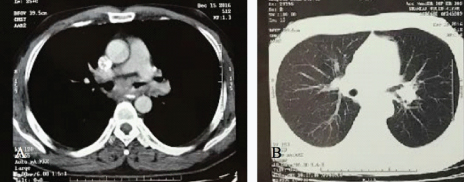
A 42-year-old man presented to the Department of Pulmonary Medicine with haemoptysis of 20 days duration. No fever, chest pain, breathlessness or weight loss was noted. He took some medicines at a local clinic to control his haemoptysis and was started on Anti-Tubercular Therapy (ATT) empirically. However, there was no relief. No bone pain, anaemia, clubbing or lymphadenopathy was noted on examination. Patient was a non smoker with no history of environmental exposure. There was no previous history of tuberculosis or any other ailments or comorbidities. No similar complaints were seen in any of the family members. His breathing was slightly coarse without crepitations or rhonchi on auscultation. A chest radiograph [Table/Fig-1] revealed an elevated left dome of diaphragm with a prominent left bronchus. Computed Tomography (CT) of thorax [Table/Fig-2] revealed a circumferential thickening of left main bronchus of about 15-16 mm resulting in narrowing of the lumen.
Chest X-ray showing elevated left dome of diaphragm with a prominent left bronchus.
Chest CT scan: a) Mediastinal window; b) Lung window.
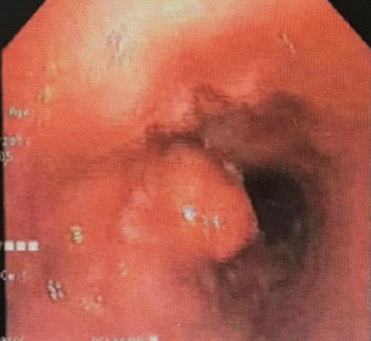
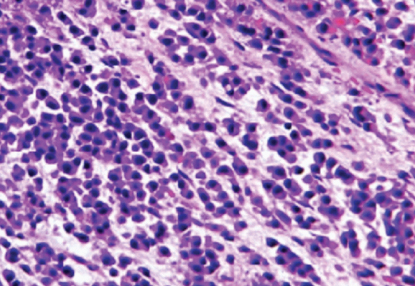
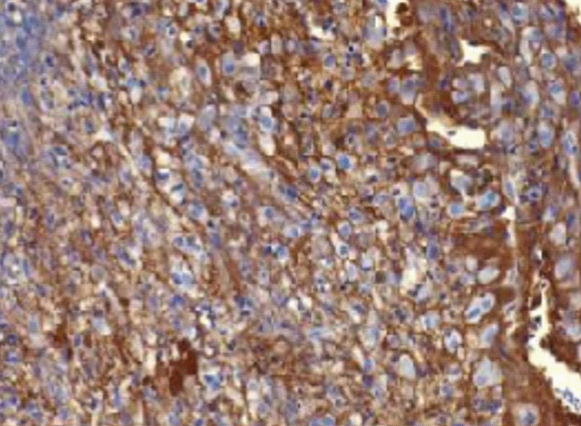
After admission, blood investigations revealed a normal haemogram, liver and renal function tests. Viral markers were negative and HBA1c was normal. Sputum for Acid Fast Bacilli (AFB) and cytology was negative. Bronchoscopic examination [Table/Fig-3] revealed a nodular growth in the lower end of the trachea extending into the carina with complete obstruction of the left main stem bronchus. Bronchial aspirate fluid was negative for bacterial culture, malignant cells and AFB culture. Histopathology of the biopsy specimen revealed a solid mass made up mostly of plasma cells [Table/Fig-4]. These tumour cells stained positively for lambda light chains [Table/Fig-5], but negatively for kappa chains. Immunohistochemistry (IHC) examination showed cells to be positive for CD45, Ki-67, Neuron Specific Enolase (NSE) and Epithelial Membrane Antigen (MUCI).
Bronchoscopy examination showed a nodular growth at the lower end of the trachea.
Microscopy examination showed plenty of plasma cells distribution (haematoxylin and eosin staining, at 100X).
Immunohistochemistry staining showing positive staining for lambda chains.
After confirming the diagnosis, the patient was evaluated for serum calcium, urine Bence Jones protein and plasma electrophoresis for Monoclonal protein (M protein) detection. All of the above examinations were negative. The skull, spine and pelvis X-ray revealed no osteolytic lesions. The bone marrow biopsy revealed normal patterns of cell distribution. The patient was unwilling to undergo any treatment and decided to pursue alternate medicine.
Discussion
Plasma cell tumours are classified into the following types: multiple myeloma, solitary myeloma (bone plasmacytoma), extramedullary (soft tissue) plasmacytoma, and plasmablastic sarcoma [1]. EMP comprises approximately 3-5% of all plasma cell neoplasms. About 80% of EMP occurs in the head and neck, and rest cases involve the upper aerodigestive tract [2]. Primary pulmonary plasmacytoma is a rare type of EMP. EMP affects males three to four times more often than females, with an average age of 55. Recently, Nie S et al., reviewed all the cases of EMP presenting in the lungs in English literature and they could only find out only 11 cases in world literature and they summarised these cases with clinical therapy and prognosis [3].
In present case, the clinical presentation was similar to pulmonary tuberculosis or lung cancer. Radiologically, the presentation was similar to lung cancer. There was central mass on left side near the hilum with compression of the left main stem bronchus. There was no involvement of mediastinal lymph nodes. On bronchoscopy examination, there was presence of intraluminal mass which was friable and highly vascular in nature. So, the intrabronchial mass was mimicking as lung cancer. Haemoptysis in present case can be explained due to the tumour invasion in the bronchus. The present case had isolated lung lesion with less clear boundaries which makes it difficult to differentiate from lung cancer. Only on histopathological examination the diagnosis of EMP was confirmed. In order to differentiate solitary EMP from multiple myeloma, bone marrow examination is required and in present case the bone marrow examination was normal. Unlike multiple myeloma, EMPs does not have serum M protein or Bence Jones light chains in the urine.
The clinical staging of primary pulmonary plasmacytoma is generally based on the Wilshaw method, divided into three stages as follows: Stage I: the tumour is confined to the primary site; Stage II: the tumour has invaded local lymph nodes; Stage III: there are obvious widespread metastases [3]. Therefore, in the present case, the clinical staging should be classified as Stage I disease.
There are no standard guidelines for the management of EMP. Primary pulmonary plasmacytoma consisting of a solitary lesion is usually treated by either surgical resection alone or resection followed by radiation therapy [4]. Various treatment strategies adopted in the past include radiotherapy, surgical resection of tumour, chemotherapy or combination of these modalities [5]. In a review of 19 cases of pulmonary plasmacytoma by Joseph G et al., has shown equal efficacy of radiotherapy and surgery as a treatment modality of these tumour [6]. In present case the patient was unwilling to undergo any treatment modality. Survival rate of pulmonary plasmacytoma is poorer as compare to head and neck plasmacytoma. Koss MN et al., reported a 2 and 5 years survival of 66% and 40%, respectively among 19 pulmonary plasmacytoma patients [7].
Conclusion
We present a case of EMP with an intrabronchial lesion without any mediastinal lymph nodes involvement and no systemic manifestations, which after reviewing literature is an extremely rare clinical manifestation of EMP.
[1]. Fanning SR, Hussain MA, Perez-Zincer F, Plasmacytoma extramedullaryE medicine 2006 :27-33. [Google Scholar]
[2]. Fletcher CDM, Diagnostic histopathology of tumours 2007 3rd EditionLondonChurchill Livingstone:214-16. [Google Scholar]
[3]. Nie S, Peng DC, Gong HH, Ye CL, Nie X, Li HJ, World J Surg Oncol 2016 14:205-09.10.1186/s12957-016-0948-827487779 [Google Scholar] [CrossRef] [PubMed]
[4]. Kim SH, Kim TH, Sohn JW, Primary pulmonary plasmacytoma presenting as multiple lung nodulesKorean J Intern Med 2012 27(1):111-13.10.3904/kjim.2012.27.1.11122403510 [Google Scholar] [CrossRef] [PubMed]
[5]. Niitsu N, Kohri M, Hayama M, Primary pulmonary plasmacytoma involving bilateral lungs and marked hypergammaglobulinemia:differentiation from extranodal marginal zone B-cell lymphoma ofmucosa-associated lymphoid tissueLeuk Res 2005 29(11):1361-64.10.1016/j.leukres.2005.04.00915878199 [Google Scholar] [CrossRef] [PubMed]
[6]. Joseph G, Pandit M, Korfhage L, Primary pulmonary plasmacytomaCancer 1993 71:721-24.10.1002/1097-0142(19930201)71:3<721::AID-CNCR2820710311>3.0.CO;2-U [Google Scholar] [CrossRef]
[7]. Koss MN, Hochholzer L, Moran CA, Frizzera G, Pulmonary plasmacytomas: A clinicopathologic and immunohistochemical study of five casesAnn Diagn Pathol 1998 2:01-11.10.1016/S1092-9134(98)80029-4 [Google Scholar] [CrossRef]