Abdominal Aggressive Fibromatosis: Diagnostic and Therapeutic Features
Houcine Maghrebi1, Amine Makni2, Amine Sebai3, Asma Labidi4, Feriel Ksantini5, Mohamed Jouini6, Montassar Kacem7, Zoubeir Bensafta8
1 Associate Professor, Department of Surgery, Rabta Hospital, Tunis, Tunisia.
2 Professor, Department of Surgery, Rabta Hospital, Tunis, Tunisia.
3 Student, Department of Surgery, Rabta Hospital, Tunis, Tunisia.
4 Associate Professor, Department of Gastroenterology, Rabta Hospital, Tunis, Tunisia.
5 Associate Professor, Department of Surgery, Salah Azaiez Institute, Tunis, Tunisia.
6 Professor, Department of Surgery, Rabta Hospital, Tunis, Tunisia.
7 Professor, Department of Surgery, Rabta Hospital, Tunis, Tunisia.
8 Professor, Department of Surgery, Rabta Hospital, Tunis, Tunisia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Houcine Maghrebi, Department of Surgery, Rabta Hospital, Djebel Lakhdhar Street, Tunis-1007, Tunisia.
E-mail: houcine.maghrebi@gmail.com
Desmoid tumours are rare soft tissue tumours developed from myofibroblasts. They usually infiltrate into adjacent muscle bundles and are characterised by the absence of metastatic potential. However, a high local aggressiveness is seen with a high rate of recurrence after surgical excision. We hereby attempt to present a series of patients with desmoid tumours and review treatment options and management strategies. Ten tumours occurred in the abdominal wall, five in the mesentery, and one was presacral tumour. The mean diameter of the tumour was 6 cm (range, 2.3-40 cm). Associated Familial Adenomatous Polyposis (FAP) was found in five patients. The margin of surgical resection was healthy in five patients. During follow up period, two patients returned with recurrence of tumours.
Desmoid tumours, Oncology, Surgery
Desmoid tumours, also known as aggressive fibromatosis, are rare soft tissue tumours. They represent 3.5% of fibrous tumours and less than 0.03% of all tumours. They occur sporadically or as part of FAP. They are characterised by local malignancy with a high tendency to recur [1,2]. Aim of this series was to report a 10-years experience of 16 desmoid tumours and review some facts with symptoms, investigation, and therapeutic aspects of this rare entity.
Case Series
From the hospital case record, a total of 16 consecutive desmoid tumours (8 patients) were identified over a duration of 10 years from January 2005 to December 2015 [Table/Fig-1].
Demographic data of treated patients.
| Case | Age (years) | Gender | Number of tumours | Tumour site | Tumour size (cm) | FAP | Teatment | Recurrence |
|---|
| 1 | 42 | M | 5 | Abdominal wall (4) | 5 | + | Tamoxifen | Stable |
| Mesenteric (1) | 3 |
| 2 | 17 | F | 2 | Abdominal wall | 8 | + | NSAID+ Tamoxifen | Stable |
| Mesenteric | 6 |
| 3 | 39 | M | 1 | Mesenteric | 5 | + | Surgery | - |
| 4 | 58 | M | 1 | Presacal | 2.3 | + | Tamoxifen | Stable |
| 5 | 30 | F | 1 | Abdominal wall | 5 | - | Surgery | - |
| 6 | 25 | F | 1 | Mesenteric | 7 | - | Surgery | - |
| 7 | 53 | F | 2 | Abdominal wall | 6 | - | Surgery | + (4 years) |
| Abdominal wall | 5 |
| 8 | 23 | F | 3 | Abdominal wall | 5 | + | Surgery | + (2 years) |
| Abdominal wall | 7 |
| Mesenteric | 40 |
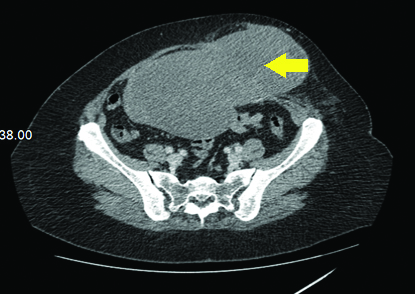
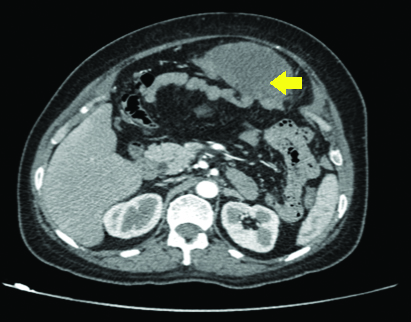
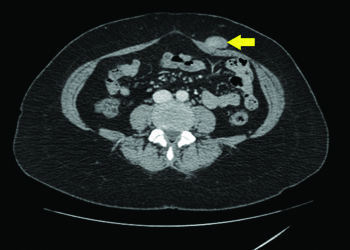
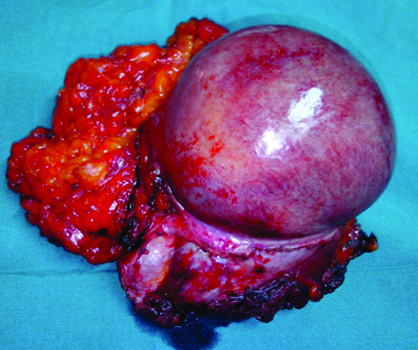
The mean age of patients was 35±14.6 years (17-58 years). The male to female ratio was 3:5. All patients underwent a CT-scan [Table/Fig-2,3 and 4] and a colonoscopy. In three cases, fibromatosis was isolated. Associated FAP was found in five patients. Polyposis was discovered by colonoscopies in two patients. In the other three patients, fibromatosis appeared after surgery for FAP with an average delay of two years after surgery. The desmoid tumours were multiple in 4 (50%) cases. A total of 10 tumours occurred in the abdominal wall [Table/Fig-5], five in the mesentery [Table/Fig-6,7], and one was presacral tumour. The mean diameter of the tumours was 6 cm (range, 2.3-40 cm). Surgical resection with wide surgical margins was the treatment of choice whenever possible. Excised specimens were all subjected to pathological evaluation.
Axial CT-scan showing abdominal desmoid tumour.
Axial CT-scan showing abdominal desmoid tumour.
CT-scan showing a desmoid tumour of the rectus abdominis muscle.
Gross appearance of a resected desmoid tumour.
Voluminous intraperitoneal desmoid tumour of the mesentery.

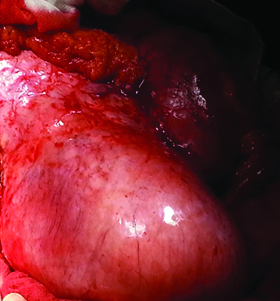
Intraoperative view of a voluminous desmoid tumour.
In two cases, treatment given was tamoxifene and/or nonsteroidal anti-inflammatory drugs. The margin of surgical resection was healthy in five patients. Soft tissue reconstruction following resection was required in two cases. No patient had surgery-related complications. During follow up (4.25 years) period, two patients returned with recurrence of tumours. Because of the nonresectable character of the tumour, they had treatment with nonsteroidal anti-inflammatory drugs and tamoxifen.
Discussion
Desmoid tumours are soft tissue tumours which develop from myofibroblasts and infiltrate into adjacent muscle bundles. They are proliferations of well-differentiated fusiform conjunctive cells associated with abundant clusters of collagen. They are characterised by the absence of metastatic potential. However, a high local aggressiveness is seen with a high rate of recurrence after surgical excision. They occur sporadically or associated to FAP [1]. Overall annual incidence is 2.4 to 4.3/100,000 inhabitants. They can appear at any age with a predilection for the third and fourth decades of life. In the present case series, the mean age was 35 years. Female predominance had been reported [2], consistent with the present case series (3 men and 5 females). Frequency in the FAP varies according to the authors between 4 to 32% [3,4]. In the present case series, the association of FAP was found in five patients because the center to which the patients presented is a reference center in the treatment of polyposis.
According to the anatomical site, desmoid tumours can be divided into extra-abdominal fibromatosis (58%); intra-abdominal fibromatosis (8-15%) and fibromatosis of the abdominal wall [1,2].
Three aetiopathogenic factors are often incriminated: trauma, hormonal influence and genetics [2]. Macroscopically, it appears as a well circumscribed hard mass, elongated in the axis of the muscle. Histologically, there is proliferation of fusiform cells corresponding to fibroblasts and myofibroblasts arranged in long divergent beams without nuclear anomaly. The main distinguishing feature with fibrosarcoma is the absence of necrosis. However, it is essentially the immunohistochemistry which makes it possible to plead for the myofibroblastic origin of these tumours. It also makes it possible to differentiate desmoid tumours from Gastrointestinal Stromal Tumours (GIST) by showing a negativity of CD-34 and S-100, whereas they are positive in GIST. Similarly, the positivity of anti-desmin and anti-alpha-actin antibodies make it possible to eliminate the fibrosarcoma for which it is generally negative [5].
Desmoid tumour has no specific symptoms. It is a firm, painless lesion that usually progresses slowly. Its size varies from 1 to 30 cm. Desmoid tumours are often hypoechogenic on ultrasound. They usually have a homogeneous appearance with a tissue density on CT scan. An hypo or iso-intense aspect in T1 and a variable signal in T2 are usually noted on MRI. This examination makes it possible to well appreciate the extension and tumour resectability [6,7].
Positive diagnosis is made possible by histological examination. We must search for a FAP with a systematic colonoscopy [8]. As for the present patients, a polyposis was discovered by colonoscopies in two patients.
Treatment is not strictly codified [9]. Different therapeutic modalities can be used: surgical resection, radiotherapy, anti-inflammatory agents, hormonal treatment and chemotherapy. Surgery with healthy resection margins remains the ideal therapeutic option for these tumours. The resection must be complete without being mutilating. Adjuvant treatments, dominated by hormonal therapy and radiotherapy, are indicated in the event of recurrence or an unresectable tumour [10] as in two cases of the present case series.
Conclusion
Desmoid tumours are rare mesenchymal neoplasm with local aggressiveness. Despite the absence of metastatic potential, these tumours remain doubtable due to their invasive potential and their high rate of recurrence. Although, histologically identical to other desmoid tumours, abdominal forms are particular by their locations, occurrence circumstances and therapy. Treatment is not strictly codified. Surgery remains the reference treatment. In case of inoperable or recurrent lesions other therapeutic alternatives remain possible with modest efficiency.
[1]. Makni A, Rebai W, Mizouni H, Fetiriche F, Jouini M, Kacem M, Desmoid tumors associated with polyposis familial adenomatousTun Med 2013 91(4):285-86. [Google Scholar]
[2]. Mignot L, Desmoid tumorsOncologie 2002 4:163-170. [Google Scholar]
[3]. Montagliani L, Duverger V, Desmoid tumorsJ Chir 2008 145:20-26.10.1016/S0021-7697(08)70288-6 [Google Scholar] [CrossRef]
[4]. Akorafas G, Nissotakis C, Peros G, Abdominal desmoid tumorsSurg Oncol 2007 16(1):131-42.10.1016/j.suronc.2007.07.00917719772 [Google Scholar] [CrossRef] [PubMed]
[5]. Leithner A, Gapp M, Radl R, Pascher A, Krippl P, Leithner K, Immunohistochemical analysis of desmoid tumoursJ Clin Pathol 2005 58(11):1152-56.10.1136/jcp.2005.02627816254103 [Google Scholar] [CrossRef] [PubMed]
[6]. Teo HEL, Peh WCG, Shek TWH, Case 84: desmoid tumor of the abdominal wallRadiology 2005 236:81-84.10.1148/radiol.236103103815987965 [Google Scholar] [CrossRef] [PubMed]
[7]. Casillas J, Sais GJ, Greve JL, Iparraguirre MC, Morillo G, Imaging of intra- and extra abdominal desmoid tumorsRadiographics 1991 11(1):959-68.10.1148/radiographics.11.6.17498591749859 [Google Scholar] [CrossRef] [PubMed]
[8]. Cotte E, Glehen O, Monneuse O, Cotton F, Vignal J, Desmoid tumors in familial adenomatous polyposisGastroenterol Clin Biol 2004 28:574-81.10.1016/S0399-8320(04)95014-2 [Google Scholar] [CrossRef]
[9]. Elias D, Prezioso G, Goharin A, Cavalcanti A, Lasser P, Treatment of desmoid tumors of the mesenteric rootPresse Med 2000 29:408-12. [Google Scholar]
[10]. Boisselier P, Foucher F, Boucher E, Raoul JL, Medical treatment of a large desmoid tumor of the mesenteric rootGastroenterol Clin Biol 2003 27(4):428 [Google Scholar]