Excision of Masson’s Haemangioma Following Suspected Liposarcoma on Imaging
Jayan George1, Duncan Meikle2, Andrew Whitfield3, Susan Hill4
1 Academic Clinical Fellow Specialty Trainee, Department of General Surgery, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom.
2 Foundation Doctor, Department of General Surgery, University Hospital Wales, Cardiff, United Kingdom.
3 Medical Student, Department of General Surgery, Sheffield Medical School, Sheffield, United Kingdom.
4 Consultant Vascular Surgeon, Department of General Surgery, University Hospital Wales, Cardiff, United Kingdom.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jayan George, Academic Clinical Fellow Specialty Trainee, Department of General Surgery, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, S5 7AU, United Kingdom.
E-mail: jayan.george@aol.com
Lipomas are commonly seen in general practice. Lipomas of large size should be investigated for the possibility of a soft tissue sarcoma. Intravascular papillary endothelial hyperplasia (Masson’s haemangioma) is a benign non-neoplastic vascular lesion that can mimic soft tissue sarcomas and can lead to an incorrect diagnosis. We report a case of a 60-year-old male artist who had an 8×8 cm swelling of his left mid-scapular region, without history of injury or trauma. Ultrasound and Magnetic Resonance Imaging (MRI) were suggestive of a lipoma or a liposarcoma. Tissue biopsy revealed fibrous tissue with a dense capillary network suspicious of a vasoformative lesion. The patient was discussed in the sarcoma multidisciplinary team and a surgical excision was decided. At the time of wide local excision, a haematoma and thrombosed veins were seen. Histology revealed a Masson’s haemangioma.
Lipoma, Magnetic, Resonance, Scapula
Case Report
A 60-year-old male presented to a general practitioner with a left sided shoulder swelling of an unknown duration (greater than a year). The patient discovered the mass on palpation which was preceded by increased stiffness in his shoulder. He had no overt pain or other associated symptoms, just an awareness of the mass. There was no trauma or injury to the shoulder and no previous surgery to the area.
His medical history included essential hypertension, gastro-oesophageal reflux disease, hypercholesterolaemia. Surgical history included a mitral valve repair with a concurrent coronary artery bypass graft that required cardiopulmonary bypass (five years back) and an inguinal hernia repair (four years back). His regular medication included ‘Omeprazole’, ‘Bisoprolol’, ‘Simvastatin’, ‘Ramipril’ and ‘Aspirin’. He works as an artist and lives with his wife. He was a non-smoker and drinks a minimal amount of alcohol.
On examination, an 8×8 cm well circumscribed, non-pulsatile, painless, mobile mass in the left mid scapular region was found. There were no overlying skin changes. Given the size of the mass he was then sent for imaging to distinguish whether this was a lipoma or soft tissue sarcoma.
Initial ultrasound scan, performed 11 weeks following presentation to his general practitioner due to service pressures, showed a well-defined, encapsulated, lipomatous intramuscular lesion in the left scapular region. Small hypoechoic areas were noted with mild vascularity.
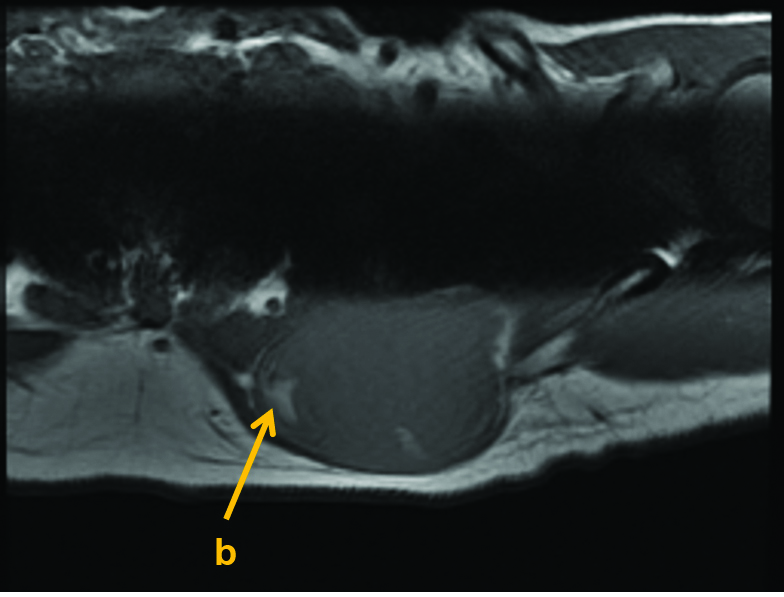
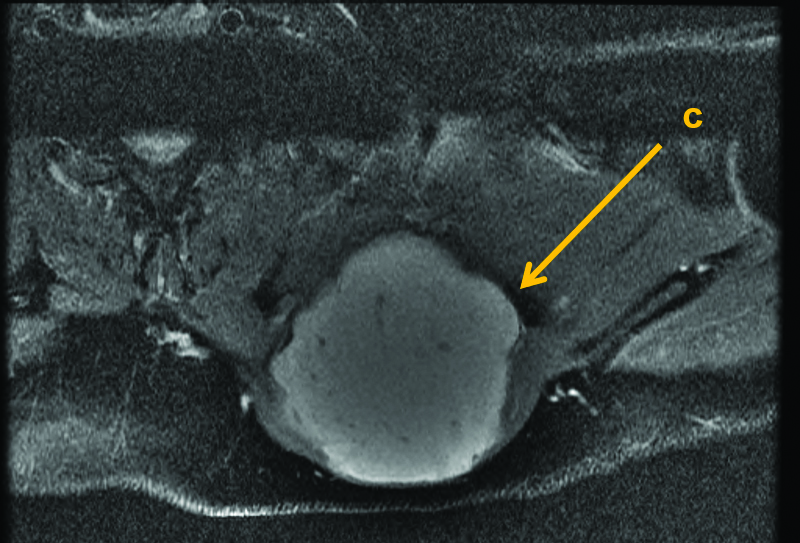
The result was discussed in the sarcoma multidisciplinary team meeting and a MRI scan was performed as per local guidelines one month later. This revealed a well-defined mass in the left scapular region, which is intermediate signal intensity on T1-weighted images with few foci of fat signal. The mass was of high intensity on proton density fat saturation images (fat gives high intensity on T1-weighted images; on fat saturation, fat should appear dark, high intensity could indicate a non-fatty tumour) measured 7.9x6.8 cm on axial plan and approximately 6 cm on sagittal plane. The mass was reported to lie within the latissimus dorsi muscle. Appearances were suspicious for soft tissue liposarcoma [Table/Fig-1,2 and 3]. No metastatic workup was considered at this stage.
MRI Axial T1-weighted imaging showing predominantly intermediate to low internal signal within the mass with sparse enhancing fat signal (b).
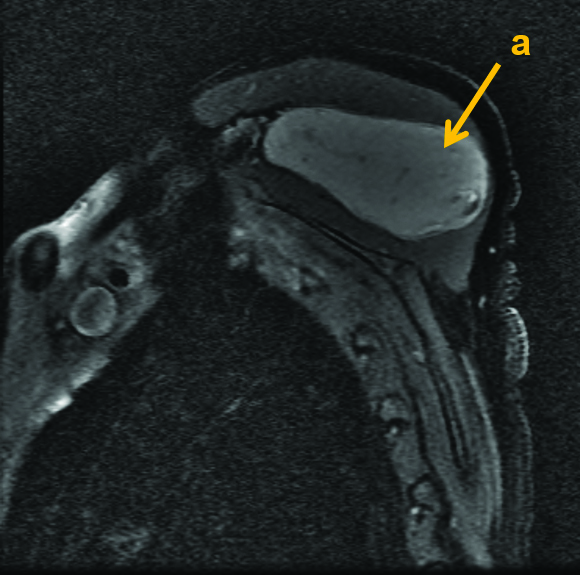
MRI Sagittal PDFS demonstrating large ovoid intramuscular mass (a) close to scapula. It demonstrates high signal on the fat enhanced imaging indicating predominantly a non-fatty tumour.
MRI axial PDFS demonstrating the mass (c) with lobulated margins and internal high signal.
Ultrasound guided biopsy results two weeks following the MRI scan showed tissue cores, mostly containing skeletal muscle, together with fragments of fibrous tissue with a dense capillary network suspicious of a vasoformative lesion but with no cytological atypia.
A wide local excision of the left sided soft tissue mass overlying the scapula was performed under general anaesthesia. An oblique incision was made over the left shoulder. This revealed a cystic lesion in the body of the left lower border of the trapezius. On opening the capsule, a liquefied haematoma and a collection of thrombosed veins were seen. The intraoperative opinion was that these veins might represent a venous malformation, possibly responsible for the inappropriate bleeding. The mass was removed without needing to infiltrate the trapezius with a 1-2 cm margin and the wound was closed primarily.
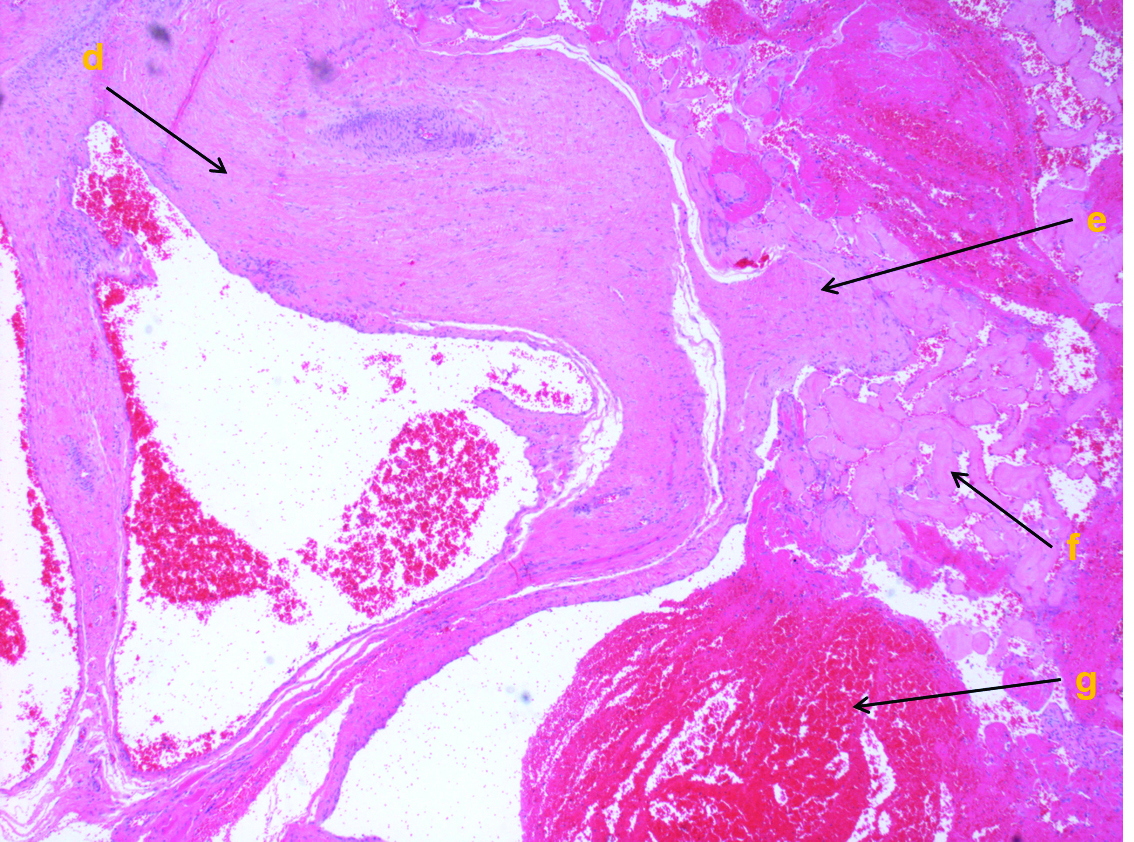
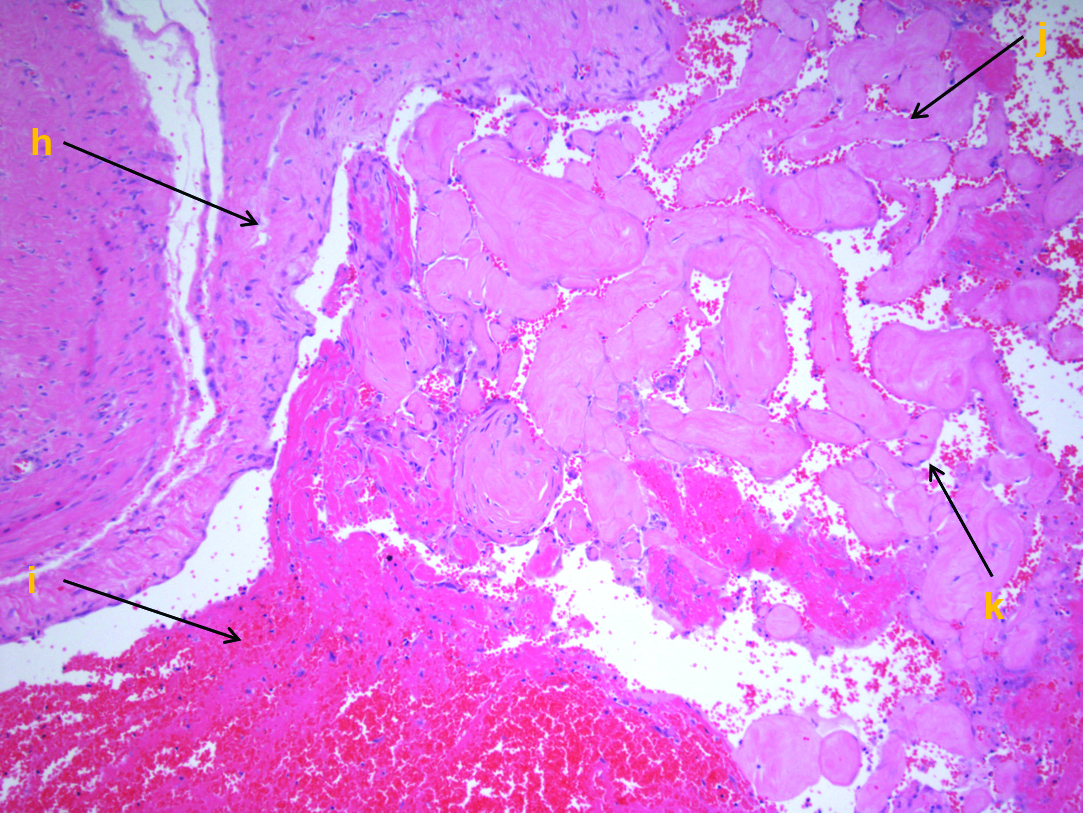
Histology revealed a vessel wall was present with hyaline papillary projections and features of thrombosis. The features were those of intravascular papillary endothelial hyperplasia (Masson’s tumour). The number of blood vessels was also increased, suggesting a pre-existing haemangioma [Table/Fig-4,5]. He was followed-up in clinic with these results six weeks following surgery.
H&E stained tissue section at x40 magnification. H&E stained tissue section at x40 magnification; (d) Blood vessel wall, part of the overall collection of blood vessels/haemangioma; (e) Fragmented vessel wall; (f) Hyaline papillary projections; (g) Red blood cells/thrombus.
H&E stained tissue section at x100 magnification. A higher power view of the hyaline papillary projections lined by endothelium and associated with thrombus; (h) Blood vessel wall; (i) Thrombus; (j) Hyaline papillary projections; (k) Lining endothelial cells on the surface.
Discussion
The present case highlights the difficulties in dealing with patients with ‘lumps and bumps’. This patient had a large mass on his back which took 11 weeks for an ultrasound to be performed. This was mainly due to the pressures on service. This should normally be done within two weeks as per guideline [1].
The present patient had a common presentation of a lipoma but there was a conflict in his investigations. Where there was a discrepancy in diagnosis, the case should be discussed in a sarcoma multidisciplinary team [2]. The present case was difficult to establish a definitive management plan because the MRI had suggested the possibility of a non-fatty tumour; however, the biopsy was encouraging but not definitive. Further investigations would have taken time and as we could operate in a short period of time the decision was taken to be aggressive to perform a wide local excision.
Masson’s haemangioma is also known as an intravascular papillary endothelial hyperplasia. Histologically the following are required for definitive diagnosis of Masson’s haemangioma: Endothelial proliferation within the vessel, multiple papillary projections, fibrin thrombus within and no evidence of necrosis [3].
There are several case reports which have identified Masson’s haemangioma. The majority are in the upper and lower limbs and head [4,5]. We could only identify one case of a 29-year-old male with a scapular swelling of four month history associated with pain and no other co-morbidities or trauma which was treated with a surgical excision [6]. It was investigated using ultrasound but the case does not state whether it was discussed in a multidisciplinary team.
Another published case was of a 60-year-old with a suspected sarcoma of the thigh that was investigated with computed tomography and MRI which suggested a soft-tissue sarcoma. The patient underwent a radical resection and histology revealed Masson’s haemangioma [7].
A recent case focussed on the imaging aspects of a Masson’s tumour reported a 45-year-old female with a painful right sided neck swelling. The MRI imaging showed similar findings to the present case in particular heterogenous fat enhancement [8]. In the present case we felt that this could be a liposarcoma and the imaging supported this, given the eventual diagnosis the darkened areas seen in the [Table/Fig-3] demonstrate the capillary networks and this was something that can be taken into account when assessing present imaging.
These cases have all advocated a surgical excision but highlight the difficulties in trying to establish a diagnosis despite advance imaging modalities. On reflection, the discrepancy in the present case was the imaging but with a greater awareness of a Masson’s haemangioma, these possibilities can be raised preoperatively. The sarcoma multidisciplinary team can use this information to decide on a surgical excision. The present case highlights the complexities in dealing with these patients but also offers other diagnostic possibilities for simple “lumps and bumps”.
Conclusion
Magnetic resonance imaging is the modality of choice for sarcomas as it is better at delineating soft tissue. Suspected sarcomas should be discussed in a dedicated multidisciplinary team. Surgical excision is the mainstay of treatment. A Masson’s haemangioma is a rare differential for an intramuscular swelling. The diagnosis is made histologically and should be in the mind of the clinician where a patient presents such as this.
[1]. Bone and soft tissue sarcoma-recognition and referral. Clinical Knowledge Summaries. Available from: http://cks.nice.org.uk/bone-and-soft-tissuesarcoma-recognition-and-referral#!diagnosissub [Accessed 15 August 2016] [Google Scholar]
[2]. Trans-Atlantic RPS Working Group. Management of Recurrent Retroperitoneal Sarcoma (RPS) in the Adult: A Consensus Approach from the Trans-Atlantic RPS Working GroupAnn Surg Oncol 2016 23(11):3531-3540.10.1245/s10434-016-5336-727480354 [Google Scholar] [CrossRef] [PubMed]
[3]. Barr RJ, Graham JH, Sherwin LA, Intravascular papillary endothelial hyperplasia. A benign lesion mimicking angiosarcomaArch Dermatol 1978 114(5):723-26.10.1001/archderm.1978.01640170023003565619 [Google Scholar] [CrossRef] [PubMed]
[4]. Tarallo M, Spagnoli AM, Fino P, Torto LO, Scuderi F, Masson’s tumor: a soft tissue tumor simulating a tendon cyst: case reportG Chir 2012 33(1-2):34-37. [Google Scholar]
[5]. Sarda A, Nachiappan M, Masson’s haemangioma presenting as a fibrolipomaJ Clin Diagn Res 2016 10(5):Pd07-Pd08.10.7860/JCDR/2016/19670.780827437299 [Google Scholar] [CrossRef] [PubMed]
[6]. Korkolis DP, Papaevangelou M, Koulaxouzidis G, Zirganos N, Psichogiou H, Vassilopoulos P, Intravascular papillary endothelial hyperplasia (Masson’s hemangioma) presenting as a soft-tissue sarcomaAnticancer Res 2005 25(2B):1409-12. [Google Scholar]
[7]. Konda P, Bavle RM, Makarla S, Muniswamappa S, Intramuscular sinusoidal haemangioma with secondary Masson’s phenomenonBMJ Case Rep 2016 :bcr201320145710.1136/bcr-2013-20145726729822 [Google Scholar] [CrossRef] [PubMed]
[8]. Yucesoy C, Coban G, Yilmazer D, Oztürk E, Hekimoglu B, Intravascular papillary endothelial hyperplasia (Masson’s hemangioma) presenting as a lateral neck massJBR-BTR 2009 92(1):20-22. [Google Scholar]