Sibling Screening of a Case of Pyroglutamic Aciduria Resulting in Normal Development- A Case Report
Bhaskaranand Nalini1, Saritha U Kamath2
1 Former Professor, Department of Paediatrics, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
2 Associate Professor, Department of Medical Laboratory Technology, School of Allied Health Sciences, Manipal Academy of Higher Education, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Saritha U Kamath, Associate Professor, Department of Medical Laboratory Technology, School of Allied Health Sciences, Manipal Academy of Higher Education, Manipal-576104, Karnataka, India.
E-mail: sarithakamath@yahoo.co.in
Pyroglutamic aciduria is a condition usually associated with metabolic acidosis and increased excretion of pyroglutamic acid in urine. It occurs due to metabolic defect in γ-glutamyl cycle. Here we report a case of 5-month-old male baby presented with respiratory symptoms who had a history of two months age sibling death due to pyroglutamic aciduria which was diagnosed by Gas Chromatography Mass Spectrometry (GCMS). Analysis of urine for organic acid by GCMS in the present baby also showed increased excretion of pyroglutamic acid. Hence in the present baby history of sibling death due to pyroglutamic aciduria led to the early diagnosis. Proper medication and timely management during fever and cold resulted in normal development.
Glutathione deficiency, Metabolic acidosis, Organic aciduria, 5-Oxoprolinuria
Case Report
A 5-month-old male baby presented to the Paediatric Department of our hospital with respiratory symptoms. He was suffering from bronchitis and respiratory distress. Detailed clinical history revealed that he had developed decreased feeding, decreased interaction and had vomiting since one day. He was born after uncomplicated pregnancy at term by normal vaginal delivery with good birth weight (3.25 kg), good cry at birth and was sucking at the breast. On family history, it was found that he had a history of sibling death at two months age. The detail about sibling history is as follows.
The elder sibling of the present case was a male baby born by normal vaginal delivery with good birth weight who had good cry immediately after birth. The baby was asymptomatic till two months after which he had cold, developed noisy breathing and cough, subsequently had an episode of rolling up of eyes and altered sensorium. Blood investigation for baseline metabolic workup showed elevated lactate, elevated ammonia and metabolic acidosis. CSF analysis showed hypoglycorhoea. Baseline metabolic workup was suggestive of organic aciduria hence sent urine for detection of organic aciduria by GCMS which showed pyroglutamic aciduria. The child was started on Evion but continued to be in altered sensorium, he became spastic and succumbed. Parents were advised for amniotic fluid analysis for pyroglutamic aciduria during next pregnancy. However, they were unable to do as the test was not available in the center.
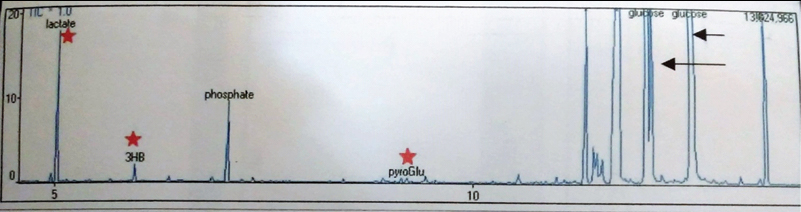
Based on sibling history and pending GCMS report present baby was started on 10% glucose with 25 mEq/L of NaHCO3, 20 mEq/L of KCl at 5 mL/kg/hour to prevent hypoxia and acidosis, along with amoxicillin 75 mg/kg body weight for two weeks according to the body weight (present baby weight was 8 kg). GCMS report showed elevated lactate, 3-hydroxy butyrate and pyroglutamic acid. No abnormality was found in the excretion of other amino acids or organic acids and hence confirmed the diagnosis as pyroglutamic aciduria [Table/Fig-1] and advised vitamin E (400 IU per day), vitamin C (500 mg/day). At the age of one year, growth and development were normal, able to sit and walk without support and was able to speak few words. At the age two and half years had an episode of lethargy during which he was not able to stand lasted for 20 minutes. Parents informed that child had decreased food intake on the previous day. Given glucose with bicarbonate rich intravenous fluids to prevent hypoxia and acidosis and baby was recovered by taking timely medication with proper guidance. After this, in between, he was suffering from recurrent cold and fever, during which he was found to be lethargic and recovered after treating with intravenous fluids as earlier. Presently, he is following dietary advice, and on vitamin E, vitamin C therapy. He is unremarkable, going to school, scored good marks in studies.
Discussion
Pyroglutamic aciduria is a disorder due to deficiency of glutathione or 5 oxoprolinase which occurs either because of inherited cause or due to acquired one [1-3]. There are many Inborn Errors of Metabolism (IEM) which are having effective treatments. Early detection and initiation of therapy if available may improve the chance of better outcome. There are many diagnostic tools for detection of inborn errors of metabolism and it is different for each disorder. In some cases it is possible to detect by clinical symptoms, presentations and in some not [4]. So, there is a need to order panel of tests for its identification along with clinical symptoms, presentation and family history.
Pyroglutamic aciduria is a rare condition which has been rarely discussed. These reports revealed that pyroglutamic aciduria both in adults and children is associated with metabolic acidosis [2,3,5-8]. In our present report baseline metabolic workup in sibling showed metabolic acidosis and hyperammonia which is finding of organic aciduria and GCMS report of urine for organic acid showed elevated pyroglutamic acid. The history of affected sibling warranted us and we could detect elevated pyroglutamic acid in urine by GCMS in the present case which was presented with symptoms of decreased interaction and vomiting. Hence, pyroglutamic aciduria in our report may be because of hereditary as both sibling’s GCMS report showed the same findings. However, we could not confirm it further.
Critical illness, sepsis, renal failure along with medication such as paracetamol precipitate the symptoms of pyroglutamic aciduria [6,7,9,10]. Many studies on adult cases showed administration of antibiotic might cause transient pyroglutamic aciduria which may resolve on the removal of causative agent [3,5,6]. Treatment involves correction of metabolic acidosis by administration of bicarbonate with sodium citrate, which is required to be given in higher doses during acute infections. Vitamin E and vitamin C are the antioxidants which are having therapeutic importance in pyroglutamic aciduria [11]. In present case, we treated the child with intravenous fluid rich in bicarbonate and glucose whenever required and with vitamin C and vitamin E with which we could prevent neurological damage in the present case.
Conclusion
Careful clinical suspicion and evaluation is required for diagnosing pyroglutamic aciduria. Further narrow down the diagnosis is required when there are baseline biochemical investigations such as hyperammonaemia or elevated lactate or metabolic acidosis in any critically ill children. It is crucial to order diagnostic tests when there is a history of sibling death or affected sibling with pyroglutamic aciduria to detect the condition early. Early diagnosis and prompt treatment may lead to normal development in affected children.
[1]. Mayatepek E, 5-Oxoprolinuria in patients with and without defects in the c -glutamyl cycleEur J Pediatr 1999 158:221-26.10.1007/s00431005105410094443 [Google Scholar] [CrossRef] [PubMed]
[2]. Hunter RW, Lawson C, Galitsiou E, Gifford F, Neary JJ, Pyroglutamic acidosis in association with therapeutic paracetamol use CasesClinical Medicine 2016 16(6):524-30.10.7861/clinmedicine.16-6-52427927815 [Google Scholar] [CrossRef] [PubMed]
[3]. Pitt JJ, Hauser S, Transient 5-oxoprolinuria and high anion gap metabolic acidosis: clinical and biochemical findings in eleven subjectsClin Chem 1998 44(7):1497-503. [Google Scholar]
[4]. Chakrapani A, Cleary MA, Wraith JE, Detection of inborn errors of metabolism in the newbornArch Dis Child Fetal Neonatal Ed 2001 84:F205-210.10.1136/fn.84.3.F20511320051 [Google Scholar] [CrossRef] [PubMed]
[5]. Croal BL, Glen ACA, Kelly CJG, Logan RW, Transient 5-oxoprolinuria (pyroglutamic aciduria) with systemic acidosis in an adult receiving antibiotic therapyClin Chem 1998 44(2):336-40. [Google Scholar]
[6]. Brooker G, Jeffery J, Nataraj T, Sair M, Ayling R, High anion gap metabolic acidosis secondary to pyroglutamic aciduria (5-oxoprolinuria): association with prescription drugs and malnutritionAnn Clin Biochem 2007 44:406-09.10.1258/00045630778094576917594793 [Google Scholar] [CrossRef] [PubMed]
[7]. Green TJ, Bijlsma JJ, Sweet DD, Profound metabolic acidosis from pyroglutamic acidemia: an underappreciated cause of high anion gap metabolic acidosisCan J Emerg Med 2010 12(5):449-52.10.1017/S148180350001263X20925168 [Google Scholar] [CrossRef] [PubMed]
[8]. O’Brien LM, Hooper M, Flemmer M, Marik PE, Chronic acetaminophen ingestion resulting in severe anion gap metabolic acidosis secondary to 5-oxoproline accumulation: an under diagnosed phenomenonBMJ Case Rep 2012 2012:02-04.10.1136/bcr.03.2012.602022761219 [Google Scholar] [CrossRef] [PubMed]
[9]. Duewall JL, Fenves AZ, Richey DS, Tran LD, Emmett M, 5-Oxoproline (pyroglutamic) acidosis associated with chronic acetaminophen usechronic acetaminophen useProc Bayl Univ Med Cent 2010 75246(1):19-20.10.1080/08998280.2010.1192857420157498 [Google Scholar] [CrossRef] [PubMed]
[10]. Ristoff E, Larsson A, Inborn errors in the metabolism of glutathioneOrphanet J Rare Dis 2007 2(16):01-09.10.1186/1750-1172-2-1617397529 [Google Scholar] [CrossRef] [PubMed]
[11]. Saudubray JM, Ogier de Baulny H, Charpentier C, Clinical approach to inherited metabolic diseases. In: Fernandes J, Saudubray J-M, van den Berghe G, editors. Inborn metabolic diseases. Diagnosis and treatment 2000 New YorkSpringer-Verlag:05-47.10.1007/978-3-662-04285-4_1 [Google Scholar] [CrossRef]