Introduction
India is still among the high IMR countries (44 per 1000 live births in the year 2012 [1]. Out of the total under-five mortality, IMR contributes to 73% [2]. Around 70% of child deaths occur around the time of weaning. Apart from the high mortality the infant also suffer morbidities due to other illnesses like diarrhoeal diseases, respiratory diseases, measles, malaria and malnutrition [2,3].
In general the IMR reflects the socioeconomic development of a country. To achieve Millennium Development Goal-4 of reducing child mortality by two-thirds by the year 2015, it is important to study factors which affect infant health. Of the total infant deaths, about 80% die at home without getting any medical help, which indicates the lack of access to essential health services [4]. There are various factors contributing to this negligence including ignorance of parents, faulty feeding practices, home remedy, faith in supernatural causes and lack of money. Integrated Management of Neonatal and Childhood Illnesses (IMNCI) also envisions that family and community health practices, especially healthcare seeking behaviours, are to be improved to reduce child morbidity and mortality [5]. This can be achieved through communication for behaviour change, which requires in-depth knowledge of the local context [5]. Understanding these practices will also help doctors to modify their approach towards families and develop new methods for gaining confidence in rural people.
People tend to go to private practitioners in the belief that they provide rapid cure [2]. Because of this the infants are devoid of getting high quality healthcare services offered by the hospitals and nurseries. The reason for this may be found by studying the behavioural pattern of parents. A significant gender differences in perception and treatment seeking for illness have been documented by some studies [6,7].
Most of the data available about care seeking behaviour is either for neonates or for under-five age group. Though infancy is a significant contributor of morbidity and mortality the care seeking behaviour and the factors which impede early care seeking in this age group have not been focused in studies. The primary aim of this study was to study the care seeking behaviour of families for their sick infants and factors which impede the early care seeking in rural areas of central India.
Materials and Methods
This was a cross-sectional observational study conducted in the adopted villages of Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences (Deemed University), of Wardha district of Maharashtra in central India over a period of two months of May and June 2014.
Sample Size
Considering the rough estimate [8] of the proportion of children below one year of age who could have one or the other acute morbidity under study to be 0.5; 95% confidence interval, absolute precision of 5% points and response distribution of 50% the sample size was calculated to be 377. However, considering the short duration of study the sample size was kept at 300 and we interviewed 303 families. The power of study falls to 80% if the sample size is taken as <290. With this sample size of 303, power of study remains >80% which is considered acceptable.
The inclusion criterion was families with a child in the age group of 1 month to 12 month. In case of a joint family with more than one child of this age group only one child’s parent was selected by lottery method. Families who had lost a child in the study age group and those families who did not want to participate were excluded.
Data Collection
Data were collected from the three villages Nachangaon, Seloo and Hingni which are adopted for provision of healthcare by Acharya Vinoba Bhave Rural Hospital in Wardha district of Maharashtra, India. The number of houses in Nachangaon, Seloo and Higni as per 2011 census were 4,464, 2458 and 1299 and the population of children between 0-6 year was 1645, 1020 and 549 respectively. The families meeting the inclusion criteria were selected by multistage random sampling to participate in the study after taking the informed consent. We went to the health sub centre of the village. Then a pen was set into circular motion and the direction of tip was selected as the direction for selecting the household. The first household fulfilling the criteria was selected and then subsequent houses were selected by visiting each house in the same direction. A total of 134 were interviewed from Nachangaon and the remaining from Seloo (96) and Hingni (73).
Questionnaire
Data were collected from mothers using a structured questionnaire containing both closed and open ended questions which was designed to capture sociodemographic information, behavioural factors affecting care seeking for sick infants and impeding factors for early care seeking. The questionnaire was designed based on the IMNCI charts and was prevalidated by subject experts from, Department of Paediatrics, Community Medicine and School for Health Professions Education (SHPER). Survey questions were asked in the local language. The questionnaire was filled by the investigators immediately during the interview.
The questionnaire included Sections A-K. Section A dealt with socio economic details. Modified Prasad scale was used to classify the respondents into various socioeconomic classes. Section B dealt with awareness of symptoms of common illness like febrile illness, and respiratory diseases in infancy and preference for seeking healthcare in general. Section C-J further explored the common illnesses with respect to awareness of the causations, complication and care seeking behavior like use of home remedies, medical consultations sought and factors affecting their choice of selecting the level of healthcare facility. Subsequent sections dealt with the impediments for early care seeking and open ended questions exploring the reasons for the preference or non preference for a particular health facility.
Statistical Analysis
Data were arranged in excel sheets and various percentages related to awareness among mothers about the common illnesses, complications and healthcare seeking behaviour were calculated and appropriate inferential statistics (chi-square test) was applied using SPSS (version 20.0) software.
Results
During the study period a total of 303 mothers were interviewed. Out of total 303 children whose mothers were interviewed 181 (59.73%) were male and 122 (40.26%) were female. Male:female ratio was 1.4:1. Infants below six months were 126 (41.58%).
As depicted in the [Table/Fig-1] all mothers were aware of fever, cough, cold however only very few mothers were aware of symptoms of malnutrition (16.5%) and anaemia (15.8%).
Awareness about the symptoms of illness in infancy: (n=303).
| Illness | Number of mothers aware of symptoms in their infants (%) |
|---|
| Fever | 303 (100) |
| Cough and cold | 303 (100) |
| Diarrhoea | 296 (97.6) |
| Pneumonia | 145 (47.8) |
| Convulsions | 133 (43.8) |
| Dysentery | 132 (43.5) |
| Jaundice | 125 (41.2) |
| Malnutrition | 50 (16.5) |
| Anaemia | 48 (15.8) |
| Others* | 42 (13.8) |
*: malaria, skin infections, ear discharge, urinary complaints, congenital disorders.
As seen in [Table/Fig-2] knowledge and awareness of danger signs of common illnesses was around 60% for respiratory and diarrhoeal diseases, but less than 15% for malnutrition and anaemia.
Knowledge of mothers about the danger signs of common illnesses in their infants (n=303).
| Illness | Knowledge of danger signs (at least one) (%) |
|---|
| Diarrhoea (lethargy, decrease urine output, blood in stools, dehydration) | 210 (69.3) |
| Fever (rash, increased chest movements, convulsions, feeding difficulty) | 203 (66.9) |
| Respiratory illness (lethargy, breathing difficulty, cyanosis,) | 193 (63.6) |
| Malnutrition (infection, stunting, poor IQ) | 42 (13.8) |
| Anaemia (poor neurodevelopment, poor growth, infection) | 38 (12.5) |
For almost all common problems, the initial treatment was taken at home, followed by health care personnel. Treatment from traditional healer was sought most commonly for convulsions, followed by jaundice and respiratory diseases as seen in [Table/Fig-3].
Disease in reference to first treatment sought (n=303).
| Disease | At home | Healthcare personnel | Not sure | Traditional healer |
|---|
| Fever | 193 (63.6) | 110 (36.3) | - | - |
| Diarrhoea/dysentery | 159 (52.4) | 144 (47.5) | - | - |
| Respiratory diseases | 170 (56.1) | 126 (41.5) | - | 7 (2.3) |
| Convulsions | 49 (16.1) | 141 (46.5) | 99 (32.6) | 14 (4.6) |
| Jaundice | 76 (25.08) | 152 (50.1) | 68 (22.4) | 7 (2.3) |
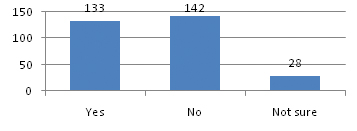
As seen in the [Table/Fig-4], 142 (46.8%) responded, that qualification of doctor did not matter while choosing the health facility.
Responses on ‘whether qualification of doctor matters while choosing a particular health facility’.
Almost 65.67% of mothers used old drugs prescribed earlier without consultation. One third mothers used half or 1/4th of adult dose for infants and only 44.5% continue drug for prescribed time after illness subsides [Table/Fig-5].
Practices about use of medication (n=303).
| Response | Old medicines prescribed earlier used without consultation | Medicines of adult given in half or 1/4th dose without prescription | Medicines continued for prescribed time after illness subsided |
|---|
| Yes | 199 (65.67) | 91 (30.03) | 135 (44.5) |
| No | 104 (34.32) | 184 (60.7) | 137 (45.2) |
| Not sure | 0 | 28 (9.2) | 0 |
| Sometimes | 0 | 0 | 31 (10.2) |
The most common health facility preferred was private clinic/hospital by around 60% of household and 36% preferred public health facility while 4% of household sought treatment from traditional healer.
There was gender difference on the type of healthcare facility sought for common illnesses. For a male infant private hospital/doctor was preferred by 52.4% families as compared to 31.1% for female infant (p=0.004). Anganwadi sevika and mobile clinics were commonly consulted for female infants (p=0.008). These findings suggest that, households were willing to spend more for male infant as compared to female [Table/Fig-6].
Facility sought for treatment based on gender.
| Healthcare facility | Male (%) | Female (%) | chi-square test p-value* |
|---|
| Primary Health Centre (PHC) | 31 (17.1) | 20 (16.3) | 0.9913, NS** |
| Anganwadi sevika | 20 (11.0) | 28 (22.9) | 0.0087, S*** |
| Private hospital/ doctor | 95 (52.4) | 38 (31.1) | 0.004, S |
| Traditional healer | 14 (4.6) | 14 (11.4) | 0.36, NS |
| ASHA | 7 (3.8) | 7 (5.7) | 0.6301, NS |
| Mobile clinic | 1 (0.5) | 7 (5.7) | 0.016, S |
| Teaching hospital | 13 (7.1) | 8 (6.5) | 0.83, NS |
| Total (n=303) | 181 | 122 |
ASHA: Accredited social health activist
p<0.01=significant; **NS: Not significant; ***S: Significant;
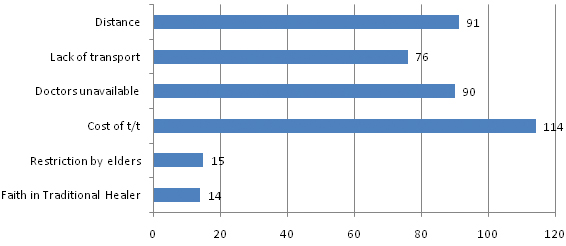
Cost of the treatment was affirmed by 114 (37.6%) of the participants, as the most common factor impeding early care seeking, followed by distance of the healthcare facility by 91 (30%), unavailability of doctors by 90 (29.7%) and lack of transport by 76 (25.08%) [Table/Fig-7].
Various impediments for early care seeking (n=303).
Discussion
In the study total mothers of 303 infants were interviewed. The ratio of male to female infant was 1.4:1. The percentage of male infants was similar to study by Deshmukh PR et al., which was conducted in similar geographical area i.e rural Wardha, where 55.1% were male [9]. The male predominance in such community based study could be due to dwindling sex ratio.
There were no families in the Class I and II, which indicates that the rural population in this part was weak economically.
In the present study, awareness about common illness was high, but that of malnutrition (16.5%) and anaemia (15.8%) was poor. In a study by Ogunlesi TA et al., 69.8% mothers could recognise jaundice in their newborn [10]. This figure is quite high as compared to the present study. Amarasiri de Silva MW et al., in their study in Sri Lanka reported that mother caretakers did not recognise malnutrition as illness; although, it was highly prevalent [11]. Saito K et al., in their study had reported that only 28% of mothers indicated they would seek medical care for malnutrition. Conversely, they considered medical care for diarrhoea, cold and worm infestations [12] These findings are in concordance with our findings. The lack of awareness about malnutrition could be because of high prevalence. A thin and short child might be considered as normal as most other children in the community were similar in physical characters.
Awareness related to complications or danger signs of different illness was poor. In the section of responses in reference to disease for which treatment is sought, maximum number of mothers responded that they would opt for home remedies for common illnesses; except for convulsions, where 46.5% mothers would prefer to visit a healthcare personnel. Similar was the response even in urban area in the study conducted by Friend-du Preez N et al., where the care givers reported that they would resort to home remedies particularly for diarrhoea and constipation [13].
Dongre AR et al., have proposed that the reason for not taking actions even in presence of danger signs/symptoms were ignorance of parents about the cause of diseases, poor socioeconomic status and faith in supernatural causes amongst others. Supernatural cause is suspected for almost all the danger signs/symptoms and hence intervention is sought from traditional healer first and then by doctors of primary health centre and private doctor [14]. In the present study 24.6% of mothers commented that convulsions were due to curse of God.
Care Seeking Behaviour
Out of the 303 mothers interviewed, 108 (35.6%) preferred to go to Public health facility, 181(59.7%) endorsed private health provider and 4.6% i.e., 14 preferred traditional healer. Willis JR et al., in their study reported that, 75% of the mother stated that private healthcare providers (qualified or otherwise) were best. Whereas only 16% said that public care providers are best [6]. The percentage of mother preferring private health provider over public health provider was very high in the study of Willis JR et al., as compared to our study (75% vs 59.7% in the present study). Corresponding percentage for preference of public health provider in present study (35.6%) was more than twice of that observed by Willis JR et al., (16%) [6]. The reason could be better organisation of referral hospitals in Wardha district of Maharashtra. There are two medical colleges in this district and also a civil hospital. Also the study was carried out in villages adopted by DMIMS as a part of comprehensive health services. Hence frequent visits by the social worker and Medical and Dental students might have helped in developing confidence in healthcare facilities. When asked to explain about why they prefer a particular health facility, those who preferred private practitioners felt that the private doctors treat fast (fast response to treatment), easy access to specialist doctors in private set up. Some preferred them because private doctors were near their village. Also, it was perceived that the private practitioner gives time to patient and provide better treatment. Whereas those who preferred public or government health facility felt that it is less costly, doctors are available in emergency medical services. Others had previous good experience at public health facilities and as diagnostic facilities are available at hospitals, patient do not have to go to other places. The common reasons stated for not choosing public health facility were improper care of patient in the government hospitals. They felt that the government doctors ignore patient’s complaints, requirements and the medicines supplied at government facilities are ineffective. On the other hand cost of consultation, unavailability of doctors all the time, lots of investigations and rush, these were the deterrents to seek private doctor’s expertise. Deshmukh PR et al., in their post survey Focus Group Discussions (FGDs) with mothers have mentioned that one of the important cause for not accessing government health facilities was lack of faith in government health services. And the reasons stated being unavailability of doctors at the primary healthcare level like subcentres/ primary health centres, at the tertiary level poor care by doctors and nurses, lack of medicines and equipments and finally no relief with the treatment offered at these centers. The paid services of doctors at private clinics were reported to be good as they were available when required; and people felt that unlike government healthcare providers, private providers treated the case in less time period, without further referring the sick child. So rural people preferred to borrow and spend money for the sick child’s treatment at private health providers rather than visiting the government facilities [9]. Many other studies have similar conclusions [8,15,16].
Most of the mothers did not consider qualification of a doctor before seeking treatment. Srivastava NM et al., in a study of care seeking behaviour among urban poor in Lucknow also found that mothers sought care outside the home (83.4%) for neonatal illness and Non Government Dispensers (NGD’s) were the leading health providers (37.6%), however more than half of the NGD’s in Lucknow may not have a recognised medical degree [17].
Around 1/3rd mothers used old drugs prescribed earlier without consultation and almost half of them do not continue treatment for the advised duration. Dongre AR et al., during focused group discussion of mothers in their study observed that nowadays mothers immediately access healthcare and prefer to take syrup, injections and tablets even though they are aware of safe home remedy for cough such as honey, tulsi, ginger, herbal tea etc. And most of them kept the left over medicines after treatment of illness and used them during the next episode before seeking medical care [8].
There was statistically significant difference in the preferred healthcare facility for male and female infant, with male infant more likely to get treatment at private health care facility. These findings are in concordance with findings of Pandey A et al., from the study in rural community of West Bengal, where they concluded that parents travelled longer distances (3.3 km for boys vs. 1.6 km for girls) to consult qualified health professionals more often (p=0.0094) for boys. The consultation was also sooner for boys as compared to girls (8.3±4.5 hours vs. 21.2±9.5 hours). Expenditure per treated episode for boys was also significantly higher than for girls (Rs. 76.76±69.23 for boys and Rs. 44.73±67.60) (p=0.023) [18]. In the study by Willis JR et al., in Uttar Pradesh, the rate of use of healthcare provider was 40% and 39% for households with sick female and male newborn infants respectively. Considering the type of healthcare provider first sought, there was no overall statistically significant (p=0.34) gender difference. However, for male neonate perceived to be sick, the households tended to use private unqualified providers more often than for female neonate (65% vs. 43%, p=0.08). On the other hand public care providers were consulted more frequently (32%) for female neonate perceived to be sick, than male neonates (21%). (p=0.04) [6]. In a study by Ghosh N et al., regarding factors affecting the healthcare-seeking behaviour of mothers in a rural community of Darjeeling district of West Bengal, they found that there is no gender difference in the preventive healthcare seeking behaviour; however, there was significant difference in the case of curative healthcare-seeking behaviour, with 68.3% males receiving treatment in Public sector and 15.5% in private sector. The corresponding figures for female were 44.7% and 7.5% respectively. This indicated the concern, utmost care and promptness in seeking treatment for male child [19]. Almost similar were the observations of Chandwani H et al., in their study from tribal community of Gujarat, India [20].
The factors identified as impediment for early care seeking in our study are similar to those of Dongre AR et al., and Mbonye AK They found that late referral to health units was complicated by, long distances to health units, unaffordable healthcare in terms of cost, pitiable attitude of health workers, unavailability of drugs at health units, and limited involvement of other family members especially fathers in care of sick children [14,21]. Lack of finances (49.6%) was also reported to be a major reason for failure to seek treatment by Taffa N and Chepngeno G [22], Awasthi S et al., in their study in Lucknow, Northern India observed that care seeking for some danger signs related to illness were influenced by ‘local beliefs’, which considered these illnesses to be untreatable by modern medicines alone. Care seeking from unqualified providers (spiritual/traditional) was 23.5% for pneumonia and 33.3% for persistent diarrhoea. They inferred that care seeking from multiple providers and use of traditional/ home remedies are important factors which leads to delay in timely and appropriate medical care [23].
The strength of this study was that this study was conducted in community setting and it threw light on the vulnerable population of infants with regards to care seeking behaviour and its hindrances.
Limitation
The limitations of the study were that there might have been an investigator effect. The mothers might have told mostly the desirable things about traditional practices and that the possibility of misunderstanding of common local terms while entering it into the questionnaire.
Conclusion
In present study, it was found that the overall awareness of mothers about common illness was good except for malnutrition and anaemia. However, mothers were unaware of danger signs of common illnesses. Mothers prefer to try home remedies before seeking medical care. Private practitioner was the most preferred healthcare provider in general and for male infants in particular. Cost and accessibility are the major hurdles for early care seeking.
Training of community health workers and ASHAs could be recommended in order to provide awareness to the mothers about recognition of danger signs in common illness and to stress upon mothers the importance of malnutrition and anaemia. Accessibility to healthcare may be improved by bringing healthcare to the doorstep through more mobile clinics and better connectivity to healthcare facilities.
Training of doctors working in public sector in communication skills for better doctor-patient relationship and mass campaigning and continuous efforts should be carried out for gender equality.
*: malaria, skin infections, ear discharge, urinary complaints, congenital disorders.
ASHA: Accredited social health activistp<0.01=significant;
**NS: Not significant;
***S: Significant;
[1]. UNICEF, Committing to Child Survival, A Promise Renewed. Annual Progress Report. September, 2013. Available from: https://www.unicef.org/publications/files/APR_Progress_Report_2013_9_Sept_2013.pdf [Google Scholar]
[2]. WHO, Global Health observatory (GHO), Infant mortality, 2012. Available from : http://apps.who.int/gho/data/node.main.526 [Access date 15th January 2014] [Google Scholar]
[3]. Winch PJ, Leban K, Casazza L, Walker L, Pearcy K, An implementation framework for household and community integrated management of childhood illnessHealth Policy Plan 2002 17:345-53.10.1093/heapol/17.4.34512424206 [Google Scholar] [CrossRef] [PubMed]
[4]. United Nations Children Fund. Millennium development goals, 2000. Available from: http://www.unicef.org/mdg/childmortality [Access date 15th January 2014] [Google Scholar]
[5]. Government of India, Ministry of Health and Family Welfare. Integrated Management [5]of Neonatal and Childhood illness: Training modules for medical officers. New Delhi:2005. pp. 03. Available from: http://www.nihfw.org/Doc/Facility%20Based%20IMNCI%20F%20IMNCI%20Facilitators%20Guide-1161.pdf [Google Scholar]
[6]. Willis JR, Kumar V, Mohanty S, Singh P, Singh V, Baqui AH, Gender differences in perception and care-seeking for illness of newborns in rural Uttar PradeshIndia J Health Popul Nutr 2009 27(1):62-71.10.3329/jhpn.v27i1.331819248649 [Google Scholar] [CrossRef] [PubMed]
[7]. Malhotra N, Upadhyay RP, Why are there delays in seeking treatment for childhood diarrhoea in India Acta Paediatr 2013 102(9):e413-18.10.1111/apa.1230423718747 [Google Scholar] [CrossRef] [PubMed]
[8]. Dongre AR, Deshmukh PR, Garg BS, Childhood morbidity, household practices and health care seeking for sick children in a tribal district of Maharashtra, IndiaIndian J Med Sci 2010 64(1):07-16.10.4103/0019-5359.9248222301804 [Google Scholar] [CrossRef] [PubMed]
[9]. Deshmukh PR, Dongre AR, Sinha N, Garg BS, Acute childhood morbidities in rural Wardha: some epidemiological correlates and health care seekingIndian J Med Sci 2009 63(8):345-54.10.4103/0019-5359.5588619770525 [Google Scholar] [CrossRef] [PubMed]
[10]. Ogunlesi TA, Oqunlesi FB, Family socio-demographic factors and maternal obstetric factors influencing appropriate health-care seeking behaviours for newborn jaundice in Sagamu, NigeriaMatern Child Health J 2012 16(3):677-84.10.1007/s10995-011-0765-121365297 [Google Scholar] [CrossRef] [PubMed]
[11]. Amarasiri de Silva MW, Wijekoon A, Hornik R, Hornik J, Care seeking in Sri Lanka: one possible explanation for low childhood mortalitySoc Sci Med 2001 53(10):1363-72.10.1016/S0277-9536(00)00425-1 [Google Scholar] [CrossRef]
[12]. Saito K, Korzenik JR, Jekel JF, Bhattacharji S, A case-control study of maternal knowledge of malnutrition and health-care-seeking attitudes in rural South IndiaYale J Biol Med 1997 70(2):149-60. [Google Scholar]
[13]. Friend-du Preez N, Cameron N, Griffiths P, “ So they belive that if the baby is sikc you must give drugs...” The importance of medicines in health-seeking behaviourfor childhood illnesses in urban South AfricaSoc Sci Med 2013 92:43-52.10.1016/j.socscimed.2013.05.01423849278 [Google Scholar] [CrossRef] [PubMed]
[14]. Dongre AR, Deshmukh PR, Garg BS, Perceptions and health care seeking about newborn danger signs among mothers of rural WardhaIndian J Paediatric 2008 75:325-29.10.1007/s12098-008-0032-718536884 [Google Scholar] [CrossRef] [PubMed]
[15]. de Zoysa R, Bhandari S, Akhtari S, Bhan R, Care seeding for illness in young Infants in an urban slum in IndiaSoc Sci Med 1998 47(12):2101-11.10.1016/S0277-9536(98)00275-5 [Google Scholar] [CrossRef]
[16]. Syed U, Khadka N, Khan A, Wall S, Care-seeking practices in South Asia: using formative research to design program interventions to save newborn livesJ Perinatol 2008 28(Suppl 2):S9-13.10.1038/jp.2008.16519057572 [Google Scholar] [CrossRef] [PubMed]
[17]. Srivastava NM, Awasthi S, Agarwal G, Care seeking behaviour and out- of- pocket expenditure for sick newborns among urban poor in Lucknow, northern India: a prospective follow-up studyBMC Health Services Research 2009 9:6110.1186/1472-6963-9-6119341473 [Google Scholar] [CrossRef] [PubMed]
[18]. Pandey A, Sengupta PG, Mondal SK, Gupta DN, Manna B, Ghosh S, Gender differences in healthcare-seeking during common illnesses in a rural community of West Bengal, IndiaJ Health Popul Nutr 2002 20(4):306-11. [Google Scholar]
[19]. Ghosh N, Chakrabarti I, Chakraborty M, Ghosh R, Biswas C, Factors affecting the healthcare-seeking behavior of mothers regarding their children in a rural community of Darjeeling district, West BengalInternational Journal of Medicine and Public Health 2013 3(1):12-16.10.4103/2230-8598.109307 [Google Scholar] [CrossRef]
[20]. Chandwani H, Pandor J, Healthcare-seeking behaviors of mothers regarding their children in a tribal community of Gujrat, IndiaElectron physician 2015 7(1):990-97. [Google Scholar]
[21]. Mbonye AK, Prevalence of childhood illnesses and care-seeking practices in rural UgandaScientific World Journal 2003 3:721-30.10.1100/tsw.2003.5212941972 [Google Scholar] [CrossRef] [PubMed]
[22]. Taffa N, Chepngeno G, Determinants of health care seeking for childhood illnesses in Nairobi slumsTrop Med Int Health 2005 10(3):240-45.10.1111/j.1365-3156.2004.01381.x15730508 [Google Scholar] [CrossRef] [PubMed]
[23]. Awasthi S, Srivastava NM, Pant S, Symptom-specific care seeking behavior for sick neonates among urban poor in Lucknow, Northern IndiaJournal of Perinatology 2008 28:S69-S75.10.1038/jp.2008.16919057571 [Google Scholar] [CrossRef] [PubMed]