Primary Intraarticular and Extraarticular Synovial Chondromatosis at Foot and Ankle: A Case Report and Review of Literature
Raghavendra S Kembhavi1, Boblee James2
1 Assistant Professor, Department of Orthopaedics, Sree Lakshmi Narayana Institute of Medical Sciences, Puducherry, India.
2 Professor and Head, Department of Orthopaedics, Sree Lakshmi Narayana Institute of Medical Sciences, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Raghavendra S Kembhavi, Plot No 8, Rajaannamalai Nagar, Behind Police Quaters, Puducherry-605006, India.
E-mail: kembhavi.raghavendra@gmail.com
Synovial chondromatosis is a benign condition in which the synovial tissue undergoes metaplastic changes into cartilagenous or osteocartilagenous bodies within joints, bursae or tendon sheaths. Knee, hip, shoulder, elbow are the commonly involved joints whereas foot and ankle joints are rare joints to be involved. They are classified into primary or secondary form depending on whether disease develops in apparently normal joint or in a pre-existent pathology like arthritis. Synovial chondromatosis can be intraarticular or extraarticular or combined. Here we report about a 52-year-old female presented with the history of mild swelling over right ankle associated with painful and terminal restriction of movement at ankle joint. She was operated with open excision of loose bodies and synovectomy. Postoperative histopathological examination confirmed the diagnosis of synovial chondromatosis without cellular atypia. Twelve months postoperative, patient was asymptomatic with no signs of recurrence.
Malignancy, Osteocartilagenous body, Recurrence, Synovectomy, Tendon sheath
Case Report
A 52-year-old female presented to the Orthopaedic department with mild swelling over medial aspect of right ankle, dull aching pain which aggravates on walking, also had a clicking sensation on movement at ankle joint. There were no similar complaints seen over other joints. History of trivial trauma was present a year back which was managed with crape bandage and analgesics by local physician.
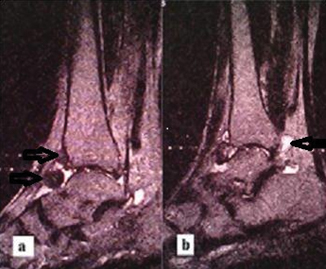
On examination, there were multiple palpable hard nodular swellings over anteromedial aspect of ankle joint which was medial to tibialis anterior tendon mainly [Table/Fig-1]. Similar minute swellings were found on lateral side of tendon. Swellings were associated with minimal tenderness, joint crepitus and ankle dorsiflexion was restricted terminally by 10 degrees. On radiological examination, there were multiple calcific bodies of less than centimetre size on anterior aspect of ankle joint [Table/Fig-2]. Magnetic Resonance Imaging (MRI) T2 weighted images showed hypointense structures corresponding to osteocartilagenous bodies anteriorly and synovial herniation at ankle joint posteriorly which was seen as hyperintense structure [Table/Fig-3a,b]. Clinicoradiologically diagnosis of synovial chondromatosis was made.
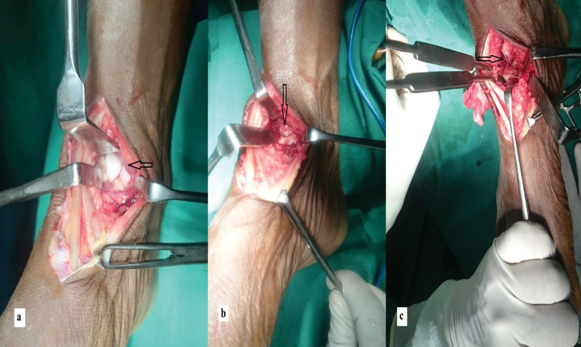
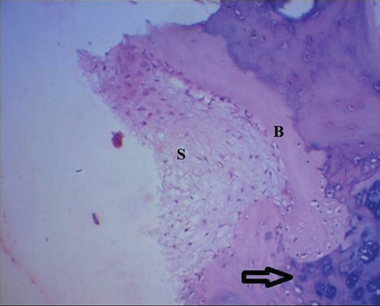
Patient was thoroughly worked up preoperatively with complete haemogram, Erythrocyte Sedimentation Rate (ESR), C-reactive protein, liver function tests, renal function tests and viral markers. All the tests were found to be normal. Due to lack of facility, we did not opt for arthroscopic excision of osteocartilagenous loose bodies but planned for open surgical excision with synovectomy after taking proper consent. Under tourniquet, anterior approach to ankle was used and plane was made between extensor hallucis longus and extensor digitorum longus. Intraoperatively, multiple whitish loose bodies of varying sizes measuring under 1×1×1 cm were noted along with hypertrophic synovium [Table/Fig-4a]. Few cartilagenous bodies seemed to be intraarticular were attached to tibio-talar surface [Table/Fig-4b]. Disease also seemed to be eroding dorsal surface of neck of talus [Table/Fig-4c]. Gross specimen was sent for histopathologic examination and diagnosis of synovial chondromatosis was confirmed without cellular atypia ruling out malignancy [Table/Fig-5].
Postoperatively patient was immobilised for three weeks with below knee plaster of paris for pain relief, three weeks, ankle joint was mobilised and patient was allowed to bear weight. With gradual physiotherapy, patient achieved full range of movement. Patient was followed up for 12 months postoperatively and was completely asymptomatic with no radiological features of recurrence [Table/Fig-6].
Picture showing prominent swelling (arrow) at anteromedial aspect of ankle joint.

Ankle radiograph lateral view showing multiple calcific loose bodies (arrows) at anterior aspect of ankle joint.

a) MRI T2 weighted image showing multiple hypointense osteocartilagenous bodies anterior to ankle joint; b) synovial herniation seen posteriorly to the ankle as hyperintense structure (arrow).
Intraoperative pictures: a) multiple osteocartilagenous loose bodies of different sizes with hypertrophic synovium around (arrow); b) Arrow showing calcific bodies over dome of talus where they appeared to be embedded in tibio-talar space; c) disease seemed to be eroding neck of talus (arrow).
Histopathology with haematoxylin and eosin stain (with magnification 10X) showed synovium with nonspecific inflammation. Section from osteocartilagenous tissue showed immature, mature cartilage (arrow) and bone arising from soft tissue component.
(S-Soft tissue, B-Bone).
Ankle radiograph lateral view showing no recurrence of anterior loose bodies at one year follow-up.

Discussion
Synovial chondromatosis is a benign pathology in which synovial tissues of the joint undergoes metaplasia resulting in multiple loose cartilagenous or osteocartilagenous bodies within joints, bursae or tendon sheaths. Commonly involved synovial joints include knee, hip, shoulder and elbow [1]. On the other hand, synovial chondromatosis is rarely seen at foot and ankle joints [2]. Presenting features of synovial chondromatosis of a joint which can be intraarticular or extraarticular include swelling, vague dull aching pain which aggravates on physical exertion and palpable nodules. Limitation of movements and locking sensations are particularly seen in intraarticular synovial chondromatosis.
Synovial chondromatosis is generally seen in the age group of 30-50 years and is more common in males than females. It is monoarticular disease but can be polyarticular in 5% of cases. Aetiology is unknown but trauma is considered to be initiating factor for both primary and secondary form of synovial chondromatosis. In our case too we had trivial trauma which probably acted as initiating factor. Though foot and ankle joints are less commonly involved when compared to other large synovial joints, there are few reports where ankle joints are involved [3-5].
Disease process classically involves three stages. In Stage I, there will be active synovial disease without loose bodies, in Stage II loose bodies as well as active synovial disease can be found and in Stage III, there will be only loose bodies without active synovial disease. In present case, disease seemed to be in later Stage II as there were calcified and uncalcified loosed bodies as well as active synovial disease as found out microscopically. Primary synovial chondromatosis is different from secondary form in that, primary form develops in apparent normal joint whereas secondary form develops in pre-existent arthritic joint. Synovial chondromatosis in joints with rheumatoid arthritis, tubercular arthritis, degenerative arthritis and osteochondritis dessicans are examples of secondary form [6]. However, due to long standing intraarticular disease, even primary form can lead to secondary arthritic changes in the joint due to articular cartilage erosion by mechanical wear [7]. In present case, though loose bodies were attached to tibiotalar surface, there was no articular damage in distal tibial surface or talar surface. However, disease seemed to be eroding dorsal surface of talar neck which was extraarticular[Table/Fig-4c]. Considering the history of swelling followed by pain in the patient, our assumption was that disease might have developed in apparently normal joint and hence the diagnosis of primary synovial chondromatosis was made.
Diagnosis is mainly based on history, examination and clinicoradiological assessment as tissue biopsy prior to surgery is rarely required unless in doubtful cases of malignant transformation. History involves dull aching pain, palapable nodules, clicking sensation and restriction in joint movement if loose bodies are intraarticular. Plain radiographs are helpful in diagnosing however, only when loose bodies are calcified which is seen in Stage III. In present case, though intraoperatively multiple loose bodies were found, radiologically the numbers appeared less which can be explained by possible transition from uncalcified bodies of Stage II to calcified loose bodies of Stage III. Computed Tomography (CT) will be helpful in identifying bony erosions, intraarticular loose bodies and early calcified bodies which are difficult to see in plain radiographs [8]. MRI is particularly helpful in diagnosing early stages of disease when unmineralised lesions are present in synovium and also helpful in knowing extent of synovial involvement. However, tissue biopsy is always confirmatory and will be helpful in differentiating it from other differential diagnoses which include synovial chondrosarcoma, pigmented villonodular synovitis, tenosynovial giant cell tumour and soft tissue chondroma [9]. In present case, history and examination associated imaging studies did not point out at any of these pathologies and hence we did not perform preoperative tissue biopsy. Malignant transformation into synovial chondrosarcoma is seen in 5% of cases of primary synovial chondromatosis [10]. Histopathological examination postoperatively in present case did not reveal cellular atypia ruling out malignancy.
Treatment depends on extent of symptoms since in asymptomatic patients conservative treatment will be sufficient since spontaneous resorption of nodules is possible. In symptomatic patients, open or arthroscopic removal of loose bodies with synovectomy is recommended. Recurrence chances following surgery are variable from 3.2 to 22.3% [10]. Few studies have highlighted on long term outcomes and chances of recurrence. Urbach D et al., showed two cases of recurrence out of five patients following arthroscopic excision of loose bodies and synovectomy in shoulder synovial chondromatosis [11]. In another study of nine patients with hip synovial chondromatosis who were managed both arthroscopically as well as open excision, only one patient had recurrence who later developed osteoarthritic changes in the hip in a mean follow-up of 24.9 months [12]. In a study of two cases of synovial chondromatosis involving ankle, both the patients had no recurrence with follow-up of more than two years [13]. In present case, there was no recurrence of anterior loose bodies 12 month postoperatively.
When it comes to managing synovial chondromatosis by excision of loose bodies alone and excision with extensive synovectomy, it is found that latter has no added advantages than former [14]. However, we opted for excision of loose bodies with synovectomy procedure.
Conclusion
Primary synovial chondromatosis at ankle and foot is a rare condition. When treated with surgery in a symptomatic patient, it is possible to get good outcome without any recurrence.
[1]. Kiritsi O, Tsitas K, Grollios G, A case of idiopathic bursal synovial chondromatosis resembling rheumatoid arthritisHippokratia 2009 13:61-63. [Google Scholar]
[2]. Galat DD, Ackerman DB, Spoon D, Turner NS, Shives TC, Synovial chondromatosis of the foot and ankleFoot Ankle Int 2008 29(3):312-17.10.3113/FAI.2008.031218348828 [Google Scholar] [CrossRef] [PubMed]
[3]. Ozmeric A, Aydogan NH, Kocadal O, Kara T, Pepe M, Gozel S, Arthroscopic treatment of synovial chondromatosis in the ankle jointInternational Journal of Surgery Case Reports 2014 5(12):1010-13.10.1016/j.ijscr.2014.10.08325460460 [Google Scholar] [CrossRef] [PubMed]
[4]. Doral Nedim M, Arthroscopic treatment of synovial chondromatosis of the ankleJournal of Foot and Ankle Surgery 2007 46(3):192-95.10.1053/j.jfas.2007.01.00117466247 [Google Scholar] [CrossRef] [PubMed]
[5]. Lee DK, Louk L, Bell BL, Synovial osteochondromatosis involvement in post-traumatic ankle injuryJournal of the American Podiatric Medical Association 2008 98(1):70-74.10.7547/098007018202338 [Google Scholar] [CrossRef] [PubMed]
[6]. Chillemi C, Marinelli M, de Cupis V, Primary synovial chondromatosis of the shoulder: clinical, arthroscopic and histopathological aspectsKnee Surg Sports Traumatol Arthrosc 2005 13:483-88.10.1007/s00167-004-0608-315726326 [Google Scholar] [CrossRef] [PubMed]
[7]. Ackerman D, Lett P, Galat DD, Parvizi J, Stuart MJ, Results of total hip and total knee arthroplasties in patients with synovial chondromatosisJ Arthroplasty 2008 23(3):395-400.10.1016/j.arth.2007.06.01418358378 [Google Scholar] [CrossRef] [PubMed]
[8]. McKenzie G, Raby N, Ritchie D, A pictorial review of primary synovial osteochondromatosisEur Radiol 2008 18:2662-69.10.1007/s00330-008-1024-818491106 [Google Scholar] [CrossRef] [PubMed]
[9]. Fetsch JF, Vinh TN, Remotti F, Tenosynovial (extraarticular) chondromatosis: an analysis of 37 cases of an underrecognized clinicopathologic entity with a strong predilection for the hands and feet and a high local recurrence rateAm J Surg Pathol 2003 27:1260-68.10.1097/00000478-200309000-0001012960811 [Google Scholar] [CrossRef] [PubMed]
[10]. Davis RI, Hamilton A, Biggart JD, Primary synovial chondromatosis: A clinicopathologic review and assessment of malignant potentialHuman Pathology 1998 29:683-38.10.1016/S0046-8177(98)90276-3 [Google Scholar] [CrossRef]
[11]. Urbach D, McGuigan FX, John M, Neumann W, Ender SA, Long-term results after arthroscopic treatment of synovial chondromatosis of the shoulderArthroscopy 2008 24(3):318-23.10.1016/j.arthro.2007.08.03418308184 [Google Scholar] [CrossRef] [PubMed]
[12]. Yu Yi H, Chan Yi S, Lee MS, Shih HN, Open and arthroscopic surgical management of primary synovial chondromatosis of the hipChang Gung Med J 2011 34:101-08. [Google Scholar]
[13]. Saxena A, St. Louis M, Synovial chondromatosis of the ankle: report of two cases with 23 and 126 loose bodiesJournal of Foot & Ankle Surgery 2017 56:182-86.10.1053/j.jfas.2016.02.00927066867 [Google Scholar] [CrossRef] [PubMed]
[14]. Shpitzer T, Ganel A, Engelberg S, Surgery for synovial chondromatosis: 26 cases followed up for 6 yearsActa Orthopaedica Scandinavica 1990 61(6):567-69.10.3109/174536790089935852281768 [Google Scholar] [CrossRef] [PubMed]