Introduction
Posterior instrumentation with Pedicle Screw Fixation (PSF) has become the current gold standard of care [1] for progressive AIS [2,3]. The correction with PSF helps in three dimensional spinal correction [4]. Fusion length with PSF is shorter in comparison with other fixation techniques [5].
The correction technique has changed over the time from predominantly concave distraction to one of segmental translation. Rod rotation using concave rod or segmental approximation is used for achieving curve correction [6]. However, the role of pedicle screw instrumentation in thoracic curves is still a matter of debate. Some authors report better correction results and a shorter fusion length even in thoracic curves [7,8], while others question the benefits of PSF in thoracic curves due to the different vertebral morphology in scoliosis, the potential risks and the questionable benefits [9,10]. Factors affecting curve correction in AIS surgery include the curve magnitude, the preoperative flexibility, the determination of the stable vertebra, the extent of surgical release, and the number of anchor points. The purpose of the present study was therefore to report on a larger series with a minimum of two years follow-up in order to assess the effectiveness of PSF and fusion.
In the present study the instrumentation technique along with fusion level selection clinicoradiological results and pulmonary function results are discussed using posterior instrumentation adolescent idiopathic scoliosis patients with a minimal two year follow-up.
Materials and Methods
In this retrospective case study, data of all consecutive patients with thoracic AIS, who were operated from posterior with pedicle screw/hook alone constructs in the same institution, with a minimal follow-up of two years were reviewed. Institutional Ethical Committee clearance was obtained for the study. All the patients were treated in the Department of Orthopaedics, during the period between January 2008 and October 2015. Records of anteroposterior and lateral, traction and bending radiographs, pulmonary function test were collected for all cases. Anthropometric data, type of curve, extent of curve, neurological status, surgical approach, fixation method used, complications and outcome were recorded. SRS 30 functional scoring system was used to measure the outcome of surgical treatment. A total of 41 cases met the following criteria: the primary curve was thoracic, only a posterior fusion was performed. The follow up was at least two years.
Inclusion criteria were patients with thoracic scoliosis of AIS only with no neurological deficits. Patients associated with neurological deficits, patients who require neurosurgical intervention for tethered cord patients who were presented with >100 degrees of Cobb’s angle, patients who presented with congenital scoliotic deformity and age group <10 and >19 years were excluded. All the patients were classified according to Kings Classification [11] and Lenke Classification [12].
Surgical Technique
As per the hospital protocol, the preoperative end vertebrae of the thoracic curves were determined by the Cobb method. Fusion was usually carried out from the upper end vertebra to the lower end vertebra. Posterior midline approach was used and posterior elements of the required levels exposed and entry points marked with k-wires at the presumed sites. Under intraoperative fluoroscopy guidance pedicle entry points were confirmed. At this ideal entry point, the pedicle was entered with an awl, checked with a blunt ended probe, and pedicle screws were inserted. Pedicle screws were not inserted into every single vertebra. Following the screw insertion, rigid rod contouring to normal sagittal curve of the instrumented spinal segments was inserted on the concave side. The concave rod was first mounted to the distal and proximal foundations. The main deformity correction was carried out by derotating the apical vertebrae individually by pulling and derotating the concave pedicle screws to the mounted concave rod. The convex side rod was only a stabilising rod which was fixed in situ after final tightening of the concave rod in corrected position. Two rods were then connected by two transverse connectors, at both ends of the construct. Following instrumentation, the posterior fusion was performed. Incentive spirometry exercises were started from secpnd postoperative day. A total body contact bivalve brace support for patients were given for a period of 3-6 months and mobilisation was done accordingly, when the pain subsided.
Determination of fusion level
The distal End Vertebra (EV) of the curve was chosen as the Lowest Instrumented Vertebra (LIV) if the end vertebra touched the Centre Sacral Vertical Line (CSVL). Preoperative supine bending radiographs were used for the selection of the curve to fuse, but they did not influence the choice of the LIV. The Uppermost Instrumented Vertebra (UIV) was the upper end of the curve.
During the follow-up patients were received in the outpatient department at three months, six months, one year and two years and clinical assessment was done. Pulmonary function was checked using pulmonary function test and radiographs were also taken at regular intervals. For functional results evaluation we have taken the criteria of SRS 30 scoring system. The scoring system described by SRS 30 gives points for function/activity, pain, self-image, mental health, satisfaction with management.
Statistical Analysis
With a standard deviation of 10 degrees and an assumed mean difference of 5 degrees and with the level of significance at 5% and power of 90% the sample size is estimated to be 41. Standard deviation=10, Mean deviation=5 degrees. Aα=0.05, 1-β=90%, Zα=1.96, Zβ=1.282, Formula: n=sd2/md2 (Zα +Zβ), n=41.
Preoperative mean Cobb’s angle, postoperative Cobb’s angle and follow up at the end of two years with preoperative TLC, FVC, FEV1 and postoperative TLC, FVC, FEV1 at the end of two years was calculated. Averages and standard deviations were also measured. The t-test was done and p<0.05 was considered significant.
Results
There were 16 males and 25 female patients and age ranged from 11 years to 19 years with average of 13.5 years at the time of procedure. Of them, 6 patients had left sided scoliosis and 35 of them had right sided scoliosis.
All the patients were classified using Kings Classification [11] and Lenke classification [12], 21 patients were Kings Type 2, 14 were Kings Type 3, 6 were Kings Type 4. We had Lenke subtypes. Fourteen patients were type 1a, 14 were type 1b, 5 were 1c, 1 patient was 2a, 1 was 2b, and 1 was 2c and 5 were 3b.
There was reduction of coronal plane deformity by 72% initially after index surgery with loss of three degrees of correction at follow-up at the end of two years as shown in [Table/Fig-1]. The changes in the pulmonary function immediately after surgery and after two years are shown in [Table/Fig-2], where in there are no significantchange noticed when compared with preoperative status, but there was a significant improvement in SRS 30 score of the patients at immediate postoperative and at 2 year follow up. Of the 41 cases operated there were: all screw construct-28, distal screws and proximal screws and hooks construct-13. Thoracoplasty was carried out in 24 patients as deemed necessary by the operating surgeon.
Degree of pre and postoperative scoliosis and kyphosis.
| Mean preoperative scoliosis | 59°±15° |
| Mean preoperative kyphosis | 25° |
| Mean immediate postoperative scoliosis | 17°±10° (72% reduction) |
| Mean postoperative scoliosis at 2 years follow-up | 19°±9° (68% reduction) |
| Correction loss | 3° (14.8%) |
The FVC, FEV1, TLC and SRS 30 scores.
| Mean pre-op FVC | 90.6 |
| Mean pre-op FEV1 | 86.67 |
| Mean pre-op TLC | 97.8 |
| Mean post-op FVC at 2 year follow-up | 86.2 (p=0.3125) |
| Mean post-op FEV1 at 2 year follow-up | 85 (p=0.5660) |
| Mean post-op TLC at 2 year follow-up | 100 (p=0.6671) |
| SRS- 30 Score at 1 year follow-up | 93±17 |
| SRS- 30 Score at 2 years follow-up | 98±22 |
Complications
There were no deep wound infections after surgery. The implant in one patient had to be removed because of the implant breakage, but on exploration a solid fusion was noted and the correction was well maintained at the most recent follow-up. One patient developed haemothorax in the immediate postoperative period which was managed conservatively. Junctional kyphosis was neither observed at 1 month after surgery nor at the most recent follow-up among the patients. There was no major vascular or neurological complication related to the pedicle screws. Preoperative and postoperative images of few patients are presented below [Table/Fig-3a,b,4a,b,5a,b6a and b].
A 12-year-old female with a preoperative Cobbs angle of 48 degrees and hypo kyphosis.
After correction the Cobbs angle was reduced to 10 degrees, at latest follow-up after 3 years was 12 degrees with a loss of 2 degrees.
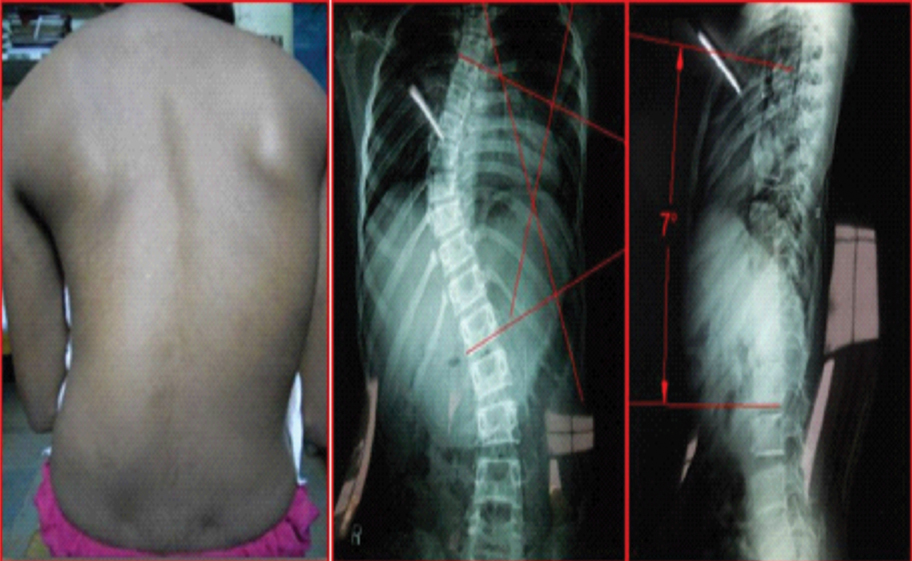
An 11-year-old female with rapidly growing deformity, with a Cobbs angle of 64 degrees and kyphosis of 11 degrees.

Postoperative clinical image and X-ray showing correction to 16 degrees immediate postoperatively which had a correction loss of 2 degrees at latest follow-up of 2.5 years.

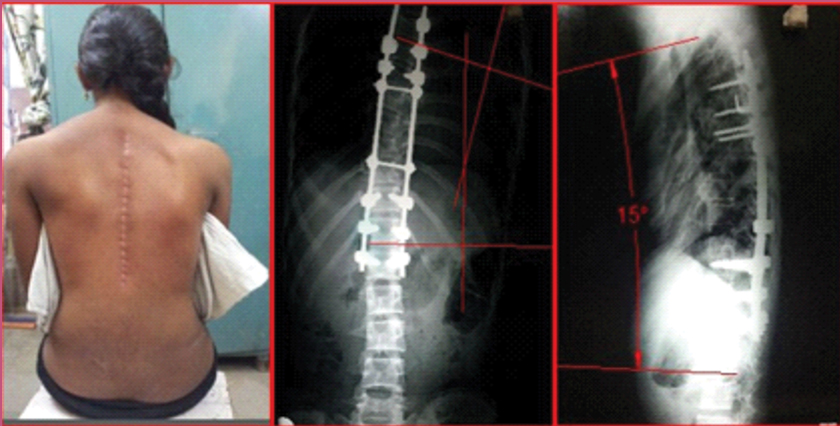
A 13-year-old female with thoracic scoliosis with 62 degrees of preoperative Cobbs angle.

Correction of the deformity to 14 degrees immediate postoperative followed by a correction loss of 3 degrees at 3 year follow-up.

A 12-year-old male with a cobbs angle of 58 degrees preoperatively with hypokyphosis.

Deformity corrected to 21 degrees immediate postoperative, with loss of 4 degrees and maintained at 25 degrees at 3 years follow-up.

Discussion
In the present study, an initial Cobb angle correction of 72% of the instrumented thoracic curves was achieved. There was some loss of correction during the two year follow-up period and the correction was 68% at two years. Various studies on instrumented correction of idiopathic adolescent scoliosis have reported some loss of correction in series of 3 to 5-year follow-up, in agreement with the here presented results [13-15]. No direct vertebral rotation was done. The apical vertebra was derotated individually by derotating the concave apex and pulling it to the concave rod. The spontaneous improvement of clinical rib hump was achieved with this method in many of the cases. Mario Di Silvestre et al., evaluated 52 patients clinically and radiographically, outcome of surgical treatment for thoracic scoliosis treated with posterior spinal fusion with a hybrid construct versus pedicle screw instrumentation [7]. They concluded that there was 52.4% of correction with a loss of 1.9 degrees.
Bradford DS and Tribus CB achieved an average scoliosis correction of 59%, using combined approaches [16]. Similar results 59% were achieved by Suk SL et al., for rigid scoliosis with vertebral column resection with severe complications in four of the patients [8]. Min K et al., in their study on 48 patients with 10 year follow-up reported a correction of 63% immediate postoperative from 58°±12° preoperative to 21°±9° at six weeks and Cobb angle was 23°±10° at two years follow-up [17]. Similar conclusion were given by Se-Il Suk with a mean preoperative Cobb angle of 51°±12° (40°-94°) and immediate postoperative correction up to 15°±6° (72% correction) and at two years follow-up with 17°±7° (68% reduction) [8].
The results obtained in present study were similar to the above mentioned studies in terms of Cobb angle correction and correction loss at two year follow-up with only complication of implant breakage in one patient and haemothorax in one patient.
PSF in AIS offers an enhanced three column fixation as well as three dimensional deformity correction and preservation of motion segments by reducing the number of levels fused. However, use of pedicle screws in thoracic spine is cautioned because of the fear of causing permanent neurological injuries due to delicate anatomy, despite the biomechanical advantages of pedicle screws over other forms of spinal instrumentation. For the thoracic pedicle screws used in the treatment of spinal deformities, the incidence of screw misplacement ranges from 1.5-25.0% with screw related neurological complication in 0-0.9% [12,17-20]. The most important step in the prevention of complications is the confirmation of an accurate pedicle screw starting point within the confines of the pedicle. Also, surgeons performing PSF of the thoracic spine must be highly experienced. The thoracic kyphosis was not influenced by posterior instrumentation initially after the operation with posterior pedicle screw instrumentation. This is in accordance with a previous report [6]. There were no acute infections. In particular, there were no complications related to thoracic pedicle screws.
Previous studies done by Muirhead A, Conner AN on 51 patients with adolescent idiopathic scoliosis [21] and by Upadhyay SS et al., on 35 patients showed no significant relation between degree of scoliosis and kyphosis and lung function [12,18]. Kim YJ et al., studied 118 adolescent patients with idiopathic scoliosis and found that there was negative correlation between Cobb angle and number of vertebrae involved with their percentage predicted FVC and FEV1 [19]. Both were identified as significant independent predictors of lung function. Twelve adolescent idiopathic patients were studied prospectively by Chen SH et al., for pulmonary function before surgery and three months, one year, two years postoperatively [20]. The indication for thoracoplasty in their series was more than 10 degree of rib hump and an average 4.4 ribs were resected. The average correction rate of scoliosis was 56% and kyphosis was 44.8%. The absolute values of pulmonary function (FVC, FEV1) and percentage predicted values returned to baseline in one year.
The same results were reported by Lenke LG et al., in a study conducted on 19 adolescents [22]. They evaluated the patients for pulmonary function before the surgery and also at the end of one year and two years after index surgery. After two years none of the values differed significantly from the preoperative values. We tried to study the relation between lung function and various curve characteristics and degree of scoliosis and kyphosis. FEV1 showed significant negative correlation with the degree of scoliosis, however, on regression analysis, the association is found to be insignificant. The influence of other factors as suggested by previous studies, as explained above, could not be made out, probably because the number of patients in present study was small. In our case series patients had lower pulmonary function (74% of predicted forced vital capacity) preoperatively consistent with the literatrure [23,24]. The pulmonary function did not change significantly in the immediate postoperative or follow-up period contrary to the findings of Pehrsson K et al., who reported improvement of FVC. Our study also showed that correction of scoliosis is not associated with improvement in FVC when adjusted to age and weight [21]. There was also no decline in pulmonary function during the two year follow-up period.
In present study, only absolute values are taken into consideration for comparison of preoperative and postoperative values. Preoperative corrected height, percentage predictions were calculated for the study of relation of scoliosis with pulmonary function. The absolute values of all the three parameters did not differ significantly from the preoperative values. This is in accordance with the earlier studies.
Limitation
All the postoperative values were nearer to the preoperative values. Even if over estimation was taken into account, it is highly probable that the corrected values will be within the acceptable range of the preoperative values. The main limitation of this study was its retrospective nature, and the sample size of the present study was small to come to a concrete conclusion regarding the changes in the pulmonary function and also only thoracic scoliosis patients were taken into the study. Further prospective study with a larger cohort may be needed to validate the present results.
Conclusion
Posterior instrumentation for correction of thoracic idiopathic adolescent scoliosis is a safe procedure using pedicle screws. Multidimensional correction can be achieved with lesser implant density and also offers long-term patient satisfaction along with maintenance of correction achieved. Pedicle screw instrumentation enables limited fusion with preservation of motion segments along with restoration of coronal and sagittal alignment. The preoperative pulmonary function does not change during the two year follow-up period.
[1]. Kepler CK, Meredith DS, Green DW, Widmann RF, Long-term outcomes after posterior spine fusion for adolescent idiopathic scoliosisCurrent Opinion in Pediatrics 2012 24(1):68-75.10.1097/MOP.0b013e32834ec98222157365 [Google Scholar] [CrossRef] [PubMed]
[2]. Olgun ZD, Yazici M, Posterior instrumentation and fusionJ Child Orthop 2013 7(1):69-76.10.1007/s11832-012-0456-524432062 [Google Scholar] [CrossRef] [PubMed]
[3]. Suk SI, Kim JH, Kim SS, Lim DJ, Pedicle screw instrumentation in adolescent idiopathic scoliosis (AIS)European Spine Journal 2012 21(1):13-22.10.1007/s00586-011-1986-021874625 [Google Scholar] [CrossRef] [PubMed]
[4]. Sarlak AY, Atmaca H, Buluç L, Tosun B, Musaoglu R, Juvenile idiopathic scoliosis treated with posterior arthrodesis and segmental pedicle screw instrumentation before the age of 9 years: a 5-year follow-upScoliosis 2009 4(1):110.1186/1748-7161-4-119123957 [Google Scholar] [CrossRef] [PubMed]
[5]. Kim SS, Lim DJ, Kim JH, Kim JW, Um KS, Ahn SH, Determination of the distal fusion level in the management of thoracolumbar and lumbar adolescent idiopathic scoliosis using pedicle screw instrumentationAsian Spine J 2014 8(6):80410.4184/asj.2014.8.6.80425558324 [Google Scholar] [CrossRef] [PubMed]
[6]. Cao Y, Xiong Q, Li F, Pedicle screw versus hybrid construct instrumentation [6]in adolescent idiopathic scoliosis: meta-analysis of thoracic kyphosisSpine 2014 39(13):E800-10.10.1097/BRS.000000000000034224732847 [Google Scholar] [CrossRef] [PubMed]
[7]. Di Silvestre M, Bakaloudis G, Lolli F, Vommaro F, Martikos K, Parisini P, Posterior fusion only for thoracic adolescent idiopathic scoliosis of more than 80: pedicle screws versus hybrid instrumentationEuropean Spine Journal 2008 17(10):1336-49.10.1007/s00586-008-0731-918696126 [Google Scholar] [CrossRef] [PubMed]
[8]. Suk SL, Lee SM, Chung ER, Kim JH, Kim SS, Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-upSpine 2005 30(14):1602-09.10.1097/01.brs.0000169452.50705.6116025028 [Google Scholar] [CrossRef] [PubMed]
[9]. Liljenqvist UR, Link TM, Halm HF, Morphometric analysis of thoracic and lumbar vertebrae in idiopathic scoliosisSpine 2000 25(10):1247-53.10.1097/00007632-200005150-0000810806501 [Google Scholar] [CrossRef] [PubMed]
[10]. Liljenqvist UR, Allkemper T, Hackenberg L, Link TM, Steinbeck J, Halm HF, Analysis of vertebral morphology in idiopathic scoliosis with use of magnetic resonance imaging and multiplanar reconstructionJBJS 2002 84(3):359-68.10.2106/00004623-200203000-0000511886904 [Google Scholar] [CrossRef] [PubMed]
[11]. King HA, Moe JH, Bradford DS, Winter RB, The selection of fusion levels in [11]thoracic idiopathic scoliosisJ Bone Joint Surg Am 1983 65(9):130210.2106/00004623-198365090-000126654943 [Google Scholar] [CrossRef] [PubMed]
[12]. Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesisJBJS 2001 83(8):1169-81.10.2106/00004623-200108000-00006 [Google Scholar] [CrossRef]
[13]. Potter BK, Kuklo TR, Lenke LG, Radiographic outcomes of anterior spinal fusion versus posterior spinal fusion with thoracic pedicle screws for treatment of Lenke Type I adolescent idiopathic scoliosis curvesSpine 2005 30(16):1859-66.10.1097/01.brs.0000174118.72916.9616103856 [Google Scholar] [CrossRef] [PubMed]
[14]. Yang X, Xu H, Li M, Gu S, Fang X, Wang J, Clinical and radiographic outcomes of the treatment of adolescent idiopathic scoliosis with segmental pedicle screws and combined local autograft and allograft bone for spinal fusion: a retrospective case seriesBMC Musculoskeletal Disorders 2010 11(1):15910.1186/1471-2474-11-15920630050 [Google Scholar] [CrossRef] [PubMed]
[15]. Clement JL, Chau E, Geoffray A, Vallade MJ, Simultaneous translation on two rods to treat adolescent idiopathic scoliosis: radiographic results in coronal, sagittal, and transverse plane of a series of 62 patients with a minimum followup of two yearsSpine 2012 37(3):184-92.10.1097/BRS.0b013e318215510421336234 [Google Scholar] [CrossRef] [PubMed]
[16]. Bradford DS, Tribus CB, Vertebral column resection for the treatment of rigid coronal decompensationSpine 1997 22(14):1590-99.10.1097/00007632-199707150-000139253094 [Google Scholar] [CrossRef] [PubMed]
[17]. Min K, Sdzuy C, Farshad M, Posterior correction of thoracic adolescent idiopathic scoliosis with pedicle screw instrumentation: results of 48 patients with minimal 10-year follow-upEuropean Spine Journal 2013 22(2):345-54.10.1007/s00586-012-2533-323064806 [Google Scholar] [CrossRef] [PubMed]
[18]. Upadhyay SS, Ho EK, Gunawardene WM, Leong JC, Hsu LC, Changes in residual volume relative to vital capacity and total lung capacity after arthrodesis of the spine in patients who have adolescent idiopathic scoliosisJBJS 1993 75(1):46-52.10.2106/00004623-199301000-000078419390 [Google Scholar] [CrossRef] [PubMed]
[19]. Kim YJ, Lenke LG, Bridwell KH, Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedureJ Bone Joint Surg Am 2005 87:1534-41.10.2106/00004623-200507000-00016 [Google Scholar] [CrossRef]
[20]. Chen SH, Huang TJ, Lee YY, Hsu RW, Pulmonary function after thoracoplasty in adolescent idiopathic scoliosisClinical Orthopaedics and Related Research 2002 399:152-61.10.1097/00003086-200206000-0001812011704 [Google Scholar] [CrossRef] [PubMed]
[21]. Muirhead A, Conner AN, The assessment of lung function in children with scoliosisJ Bone Joint Surgery Br 1985 67:699-702.10.1302/0301-620X.67B5.4055863 [Google Scholar] [CrossRef]
[22]. Lenke LG, Bridwell KH, Blanke K, Baldus C, Analysis of pulmonary function and chest cage dimension changes after thoracoplasty in idiopathic scoliosisSpine 1995 20(12):1343-50.10.1097/00007632-199520120-000047676331 [Google Scholar] [CrossRef] [PubMed]
[23]. Pehrsson K, Danielsson A, Nachemson A, Pulmonary function in adolescent idiopathic scoliosis: a 25 year follow up after surgery or start of brace treatmentThorax 2001 56(5):388-93.10.1136/thorax.56.5.38811312408 [Google Scholar] [CrossRef] [PubMed]
[24]. Kearon C, Killian J, Fadors determining pulmonary fundion in adolescent idiopathic thoracic scoliosisAm Rev Respir Dis 1993 148:288-94.10.1164/ajrccm/148.2.2888342890 [Google Scholar] [CrossRef] [PubMed]