A Rare Case of Primary Leiomyosarcoma of the Ovary
Vishwanath1, Neetham Vyas2, Shreeja Goripally3, Supriya Rai4
1 Consultant, Department of Surgical Oncology, K.S. Hegde Medical Academy, NITTE University, Mangalore, Karnataka, India.
2 Associate Professor, Department of Obstetrics and Gynaecology, K.S. Hegde Medical Academy, NITTE University, Mangalore, Karnataka, India.
3 Juinor Resident, Department of Obstetrics and Gynaecology, K.S. Hegde Medical Academy, NITTE University, Mangalore, Karnataka, India.
4 Professor, Department of Obstetrics and Gynaecology, K.S. Hegde Medical Academy, NITTE University, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Neetha M Vyas, ‘Ashraya’ 1st, Main 3rd Cross, Subashnagar, Mangalore-575001, Karnataka, India.
E-mail: nvyas_21@yahoo.com
Ovarian leiomyosarcoma is a very rare tumour representing less than 1% of all ovarian tumours. Primary sarcoma of ovary is about 3% of all ovarian tumours. Fibrosarcoma, chondrosarcoma, angiosarcoma, rhabdomyosarcoma and leiomyosarcoma have been reported. They have an aggressive behaviour and poor prognosis. Till date less than 100 cases have been reported. Because of their rarity, there is no case series to establish definitive treatment guidelines. Even the type of adjuvant therapy which could be beneficial has not yet been established. We present a case of ovarian leiomyosarcoma in which patient underwent total abdominal hysterectomy with bilateral salphingo-ophorectomy, pelvic lymphadenectomy and omental biopsy. Microscopy and Immunohistochemistry (IHC) established the diagnosis.
Adjuvant therapy, Soft tissue sarcoma, Tumour
Case Report
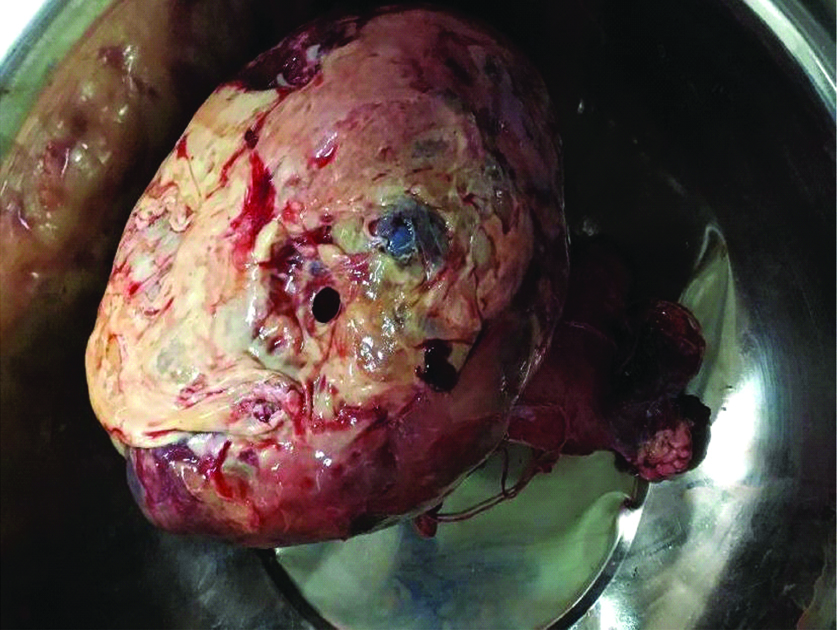
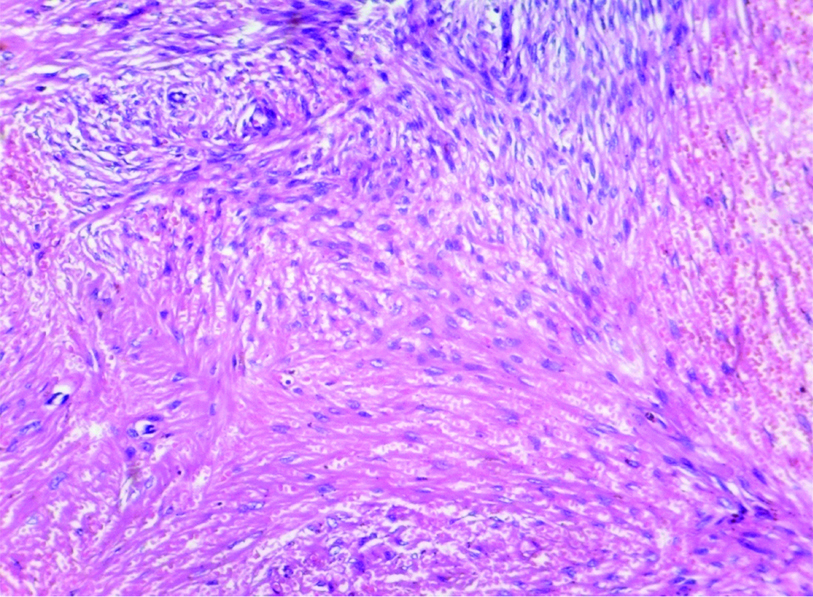
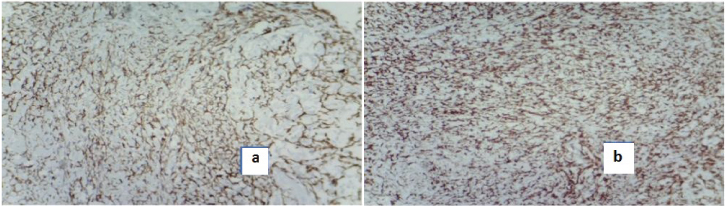
A 55-year-old parous postmenopausal woman presented to us with pain in abdomen and abdominal distension since two months. She had significant loss of appetite. On abdominal examination, a hard mobile mass of 15×15 cm was felt. Clinically, there was no evidence of free fluid in the abdominal cavity. Bimanual examination confirmed the abdominal findings. Ultrasonography showed a large, mixed solid and cystic mass arising from right adnexa, uterus appeared normal in size and the left ovary could not be visualised. There was a minimal amount of free fluid in the abdominal cavity. Contrast Enhanced Computed Tomography (CECT) showed a well defined, mixed solid and cystic mass of 15×15 cm, with enlarged para-aortic lymph nodes and minimal ascites. Other abdominal organs and omentum appeared normal [Table/Fig-1]. The level of serum Carbohydrate Antigen (CA) 125 was 150 U/mL and other tumour markers such as Alpha-Fetoprotein (AFP), beta-human chorionic gonadotropin (βhcg), Carcinoembryonic Antigen (CEA) were within normal range. Staging laparotomy was done. Intraoperatively, minimal peritoneal fluid was noted and was collected for cytology. A right ovarian mass of 15×15 cm with areas of necrosis on the surface was noted [Table/Fig-2]. Uterus and other ovary appeared normal. Also, omentum grossly appeared normal and no other peritoneal deposits. Histopathological examination of right ovarian mass revealed spindle cells with moderate cytoplasm arranged in fascicles having pleomorphic hyperchromatic nuclei [Table/Fig-3]. The IHC showed positivity for Smooth Muscle Actin (SMA) and vimentin and negative for Cluster of Differentiation (CD) 34 and pan-cytokeratin antibody suggesting leiomyosarcoma [Table/Fig-4]. Peritoneal cytology showed malignant cells. Lymph nodes and omentum were free of tumour. So, a final diagnosis of leiomyosarcoma of ovary; intermediate grade, stage 1C was made. Postoperative period was uneventful. She was advised adjuvant chemotherapy with docetaxel and gemcitabine. Patient received three cycles of chemotherapy. Presently, she has been on follow up for two months after her last chemotherapy.
CECT picture showing well defined large mixed solid and cystic mass arising from right adnexa.

Specimen showing right ovarian mass of 15x15 cm with areas of necrosis on the surface, uterus and other ovary appears normal.
H&E stain of 100X showing spindle shaped cells with moderate cytoplasm arranged in fascicles having pleomorphic hyperchromatic nuclei.
Immunohistochemistry showing positivity for a) smooth muscle actin and b) vimentin.
Discussion
Primary leiomyosarcoma of ovary constitutes <1% of all ovarian tumours. Primary sarcoma of ovary is about 3% of all ovarian tumours [1]. Sarcoma of ovary includes fibrosarcoma, chondrosarcoma, angiosarcoma, rhabdomyosarcoma, stromal cell sarcoma and leiomyosarcoma. Among these, leiomyosarcoma is the least as ovary does not content smooth muscle fibers. The origin of this tumour is still a dilemma. Ovarian leiomyosarcomas usually occur in postmenopausal age group and are unilateral tumours [2]. They are present with pain and palpable abdominal mass. Grossly, they are large tumours (>10 cm size) with solid and cystic appearance with areas of haemorrhage and necrosis. Microscopically, they differ from their benign counterpart in being hypercellular and presence of increased mitotic figures (>10/10 high power field) [3].
The exact pathogenesis is uncertain as ovary does not contain smooth muscles. It is said that it may originate from smooth muscle of ovarian blood vessel or from muscle fibers of ligamental attachments of the ovary [4]. There are theories suggesting that totipotent cells of the ovary might differentiate into smooth muscle which also could be the origin of the tumour. Depending on the source of origin, leiomyosarcomas are of three types; teratoid, mesenchymal and mullerian. The mesenchymal origin are seen in postmenopausal age and are more likely to metastasise where as teratoid origin is seen in younger age group and are usually unilateral [5]. Though, many cases are seen in postmenopausal age group, like in present patient, there are a few cases reported even in younger age group like 27-30 years [1,6].
Grossly, they appear similar to sarcomas as solid mass with cystic degeneration with areas of necrosis and haemorrhage. Microscopically, uniformly arranged spindle shaped cells with abdundant cytoplasm and nuclear atypia is noted. The IHC helps in the accurate diagnosis and markers include desmin, SMA, vimentin and caldesmon. There are no specific serum tumour markers for detecting leiomyosarcoma.
Surgery still remains the mainstay of treatment. Surgery includes total abdominal hysterectomy with bilateral salphingo-ophorectomy, pelvic lymphadenectomy and omentectomy. Fertility preserving surgery can be considered in younger age group. Staging is as per International Federation of Gynaecology and Obstetrics (FIGO) staging for ovarian carcinoma. Benefit of adjuvant therapy with chemotherapy or radiotherapy is not well documented as the reported cases are few and no studies are done to prove their efficacy due to rarity of the disease [7]. Pankaj S et al., used post adjuvant chemotherapy with docetaxel and gemcitabine which is frequently used in uterine leiomyosarcoma and showed 30 months disease progession free interval [6]. Kumar VJ et al., demonstrated chemotherapy with vincristine, epirubicin, and cyclophosphamide was beneficial to prolong progression free survival [1]. We also recommended docetaxel and gemcitabine combination to present patient as ascitic fluid cytology was positive for malignant cells.
Prognosis depends on stage of the tumour, tumour size and mitotic index. Prognosis is poor as 80% of patients in stage II-IV die within a year. A 63% of patients of stage I disease are alive without evidence of the disease at the end of 42 months. A five-year survival rate is 32% overall for ovarian sarcomas and for ovarian leiomyosarcoma it is just 18% [6].
Conclusion
Leiomyosarcoma is a rare tumour of the ovary. Ovarian leiomyosarcoma are highly aggressive with an inherent poor prognosis. Diagnosis is mainly by IHC. Although, surgery is performed in all cases, extent of surgery is debatable. Benefit of adjuvant therapy is inconclusive. More studies on this particular ovarian tumour are required to establish definitive treatment.
[1]. Kumar VJ, Khurana A, Kaur P, Chuahan AK, Singh S, A rare presentation of primary leiomyosarcoma of ovary in a young womanEcancermedicalscience 2015 9:52410.3332/ecancer.2015.52425932048 [Google Scholar] [CrossRef] [PubMed]
[2]. Rivas G, Bonilla C, Rubiano J, Arango N, Primary leiomyosarcoma of the ovary: a case reportCase Reports in Clinical Medicine 2014 3:192-96.10.4236/crcm.2014.34045 [Google Scholar] [CrossRef]
[3]. Dixit S, Singhai S, Baboo HA, Vyas RK, Neema JP, Murthy R, Leiomyosarcoma of the ovaryJ Postgrad Med 1993 39(3):151-53. [Google Scholar]
[4]. Kaul R, Sharma J, Primary leiomyosarcoma of ovaryOnline J Health Allied Scs 2009 8(3):16 [Google Scholar]
[5]. Kaur J, Mishra M, Goel B, Primary ovarian leiomyosarcoma: a case report with reviewInt J Reprod Contracept Obstet Gynecol 2014 3(1):258-60.10.5455/2320-1770.ijrcog20140355 [Google Scholar] [CrossRef]
[6]. Pankaj S, Choudhary V, Singh RK, Harshvardhan R, High grade pleomorphic leiomyosarcoma of ovary in young female: a caseWorld J Surg Res 2013 7:07-11. [Google Scholar]
[7]. Lee BN, Ouh YT, Choi HJ, Yang SY, Lee JK, Hong JH, Leiomyosarcoma of the ovary mimicking gastrointestinal stromal tumour originating from small bowel: a case report and literature reviewGynecol Obstet (Sunnyvale) 2016 6(2):35910.4172/2161-0932.1000359 [Google Scholar] [CrossRef]