Introduction
Laparoscopy is increasingly being performed for urologic surgeries either through transperitoneal or retroperitoneal approach. While physiological changes during transperitoneal surgeries have been extensively studied, very few studies have explored the effect of retroperitoneal laparoscopy.
Aim
To compare physiological changes that occurred when urologic laparoscopic surgeries were carried out through either transperitoneal or retroperitoneal approach in lateral positions. Primary outcome was respiratory changes and haemodynamic changes were considered secondary outcome.
Materials and Methods
This single centre prospective non randomised human study was conducted in 46 healthy individuals undergoing elective urologic laparoscopic surgeries at Dr. H.L. Trivedi Institute of Transplantation Sciences, Ahmedabad, Gujarat, India, from January 2017 to July 2017 and patients were divided into two groups according to the surgical approach used: 1) Transperitoneal (Trans) group; and 2) Retroperitoneal (Retro) group. Compliance, Peak Inspiratory Pressure (PIP), Minute Ventilation (MV), Heart Rate (HR) and Mean Arterial Pressure (MAP) were monitored at defined time interval. Arterial blood gases were also measured to compare Partial Pressure of Arterial Oxygen/Fraction of Inspired Oxygen (PaO2/FiO2) ratio.
Chi-square and t-test were used for statistical comparison between the two groups. A p-value<0.05 was considered significant.
Results
PaO2/FiO2 ratio improved in Trans (from 395.45±128.35 to 439.88±87.77) and decreased in Retro group (from 399.29±57.6 to 349.72±97.89) at the end of pneumoperitoneum with significant statistical difference between the two groups. Compliance decreased to 37% of baseline (from 33.03 to 20.99 mL/cm H2O in Trans group and from 37.02 to 23.23 mL/cm H2O in Retro group) and PIP increased to 45% from baseline (from 18.43 to 26.13 cm H2O in Trans group and from 17.91 to 25.86 cm H2O in Retro group) in both the groups without any statistical difference. The HR remained higher in Trans group as compared to Retro group during the insufflation period. The MAP remained higher than baseline during pneumoperitoneum in both the groups. Statistical comparison of HR and MAP between the two groups was insignificant.
Conclusion
Respiratory and haemodynamic parameters remain stable and are comparable between the two approaches. Larger studies are required to validate this results.
Introduction
Laparoscopy gives the advantage of decreased postoperative pain, minimal scars, rapid recovery and short convalescence when compared to open surgery. Therefore, many renal procedures like, simple nephrectomy, living donor nephrectomy, partial or radical nephrectomy and pyeloplasty are increasingly being carried out laparoscopically either through transperitoneal or retroperitoneal approach [1]. While retroperitoneal approach may be advantageous due to safe port placement and lesser handling of abdominal viscera, it may be technically challenging due to smaller working space and port proximity as compared to transperitoneal approach [2].
Physiological changes during laparoscopy have been extensively studied. Few studies have compared the effects of laparoscopy when performed through either transperitoneal or retroperitoneal approach [3-7]. Streich B et al., and Demiroluk S et al., found to have higher Carbon Dioxide (CO2) absorption with retroperitoneal approach [3,4]. In another study by Ng CS et al., retroperitoneoscopic surgery was not associated with increased CO2 absorption [5]. Ventilatory and haemodynamic functions were less affected with retroperitoneal approach in the study done by Nadu A et al., while Baird JE et al., found that the effects of CO2 insufflation on haemodynamics and partial pressure of CO2 are the same in the retroperitoneal and intraperitoneal spaces [6,7]. Patient population, type of surgery and positions during surgery were not similar between the comparing groups in most of these studies with variable outcome. Thus, we conducted a study to compare respiratory and haemodynamic changes that occurred when urologic laparoscopic surgeries were carried out through either transperitoneal or retroperitoneal approach in lateral positions.
Materials and Methods
After local ethics committee approval and informed patient consent, this non randomised prospective study was done on 46 patients scheduled to undergo elective urological laparoscopic surgeries at Dr. H.L. Trivedi Institute of Transplantation Sciences, Ahmedabad, Gujarat, India, from January 2017 to July 2017. Adult American Society of Anaesthesiologists (ASA) physical status 1 to 3 patients of either sex with Body Mass Index (BMI) less than 30 were included in the study. Exclusion criteria were morbid obesity, cardiorespiratory insufficiency, severe liver or renal dysfunction and previous laparotomy.
Forty six patients posted for urological laparoscopy in kidney position were divided into two groups; either Trans or Retro. The choice of approach either transperitoneal or retroperitoneal was chosen by the surgeon according to his/her comfort and patients medical condition. The routine preoperative evaluation for laparoscopic surgeries was done. General anaesthesia was used for both groups. Patients were premedicated with 1-2 μgm/kg fentanyl and 0.004-0.008 μgm/kg glycopyrollate intravenous (i.v.) in the operation theatre. Anaesthesia was induced with thiopentone sodium 4-6 mg/kg i.v. and muscle relaxation was obtained with atracurium 0.5-0.8 mg/kg i.v. for tracheal intubation. Anaesthesia was maintained with isoflurane in a mixture of oxygen and air with incremental doses of atracurium and fentanyl. Volume controlled mode was used for all patients initially. Change in tidal volume, respiratory rate or change in mode to pressure controlled ventilation was done when oxygen saturation decreased to less than 97%, PIP greater than 35 mmHg or End Tidal Carbon Dioxide (EtCO2) partial pressure greater than 40 mmHg. The HR, Blood Pressure (BP), EtCO2, peak airway pressure and compliance were recorded at induction, after position, 10, 20, 30, 60 minutes after pneumoperitoneum, at the end of pneumoperitoneum and after extubation. Also, hourly reading was taken of these parameters after one hour of pneumoperitoneum till the end of surgery. Arterial blood gases were measured twice, at induction and after end of pneumoperitoneum to observe the effect of either approach (transperitoneal and retroperitoneal) on PaO2/FiO2 ratio of oxygen and PaCO2-EtCO2 difference.
Statistical Analysis
Data were presented as mean±Standard Deviation (SD) for quantitative variables, number and percentage for categorical variables. Chi-square and t-test were used where appropriate. A p-value<0.05 was considered significant.
Results
There were 23 patients in each group; Trans and Retro groups. One patient in Retro group was converted to open surgery due to extensive adhesions making a total of 45 patients for statistical comparison. There was no significant difference in age, sex, weight and duration of pneumoperitoneum and surgery between the two groups (p>0.05) [Table/Fig-1]. The [Table/Fig-2] shows, type of surgeries that patients underwent in both the groups. Two patients developed subcutaneous emphysema in Trans group.
| Sr. no | Variables | Transperitoneal group (n=23) | Retroperitoneal group (n=22) | p-value* |
|---|
| 1 | Age (years) | 43.30±15.87 | 46.9±13.29 | 0.414 |
| 2 | Gender (male/female) | 12/11 | 15/7 | 0.273 |
| 3 | Weight (kg) | 55.43±9.89 | 61.54±11.32 | 0.060 |
| 4 | Lateral positions (right/left) | 14/9 | 7/15 | 0.051 |
| 5 | Duration of CO2 insufflation (mins) | 194.13±54.43 | 174.32±52.74 | 0.222 |
| 6 | Duration of surgery (mins) | 266.73±61.86 | 207.27±57.73 | 0.177 |
*p-value<0.05 is statistically significant, mins-Minutes
| Surgery type | Transperitoneal (n=23) | Retroperitoneal (n=22) |
|---|
| Donor nephrectomy | - | 9 |
| Simple nephrectomy | 13 | 9 |
| Partial nephrectomy | - | 1 |
| Radical nephrectomy | 7 | 1 |
| Pyeloplasty | 3 | - |
| Ureterolithotomy | - | 2 |
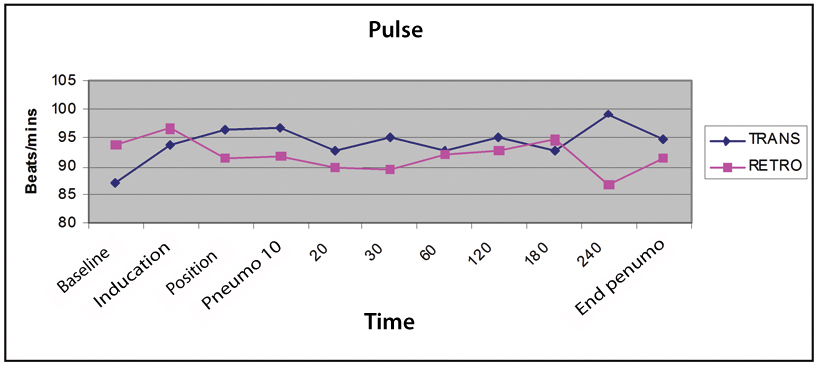
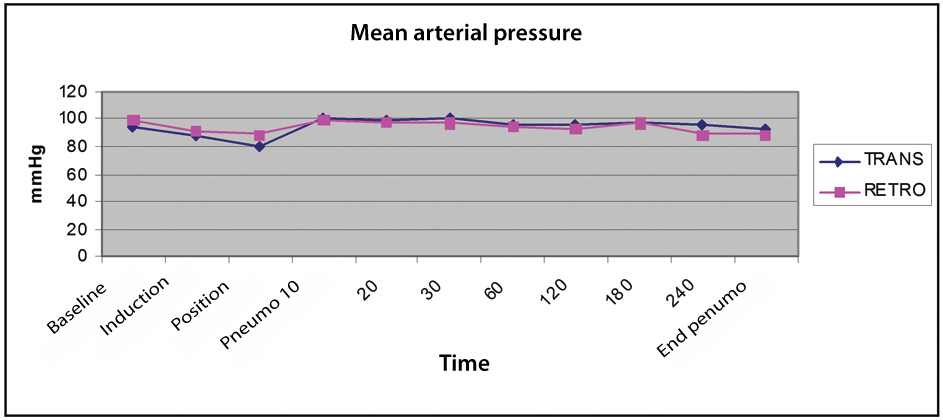
The HR increased after induction and remained between 90 to 100 beats per minutes throughout the surgery without any significant difference between the two groups (p>0.05) [Table/Fig-3]. Between the two groups MAP decreased at induction, decreased further with position, increased at insufflation of pneumoperitoneum and then remained same throughout the surgery. The difference in MAP at various interval time between the two groups was statistically insignificant (p>0.05) [Table/Fig-4].
Comparison of Mean arterial pressure.
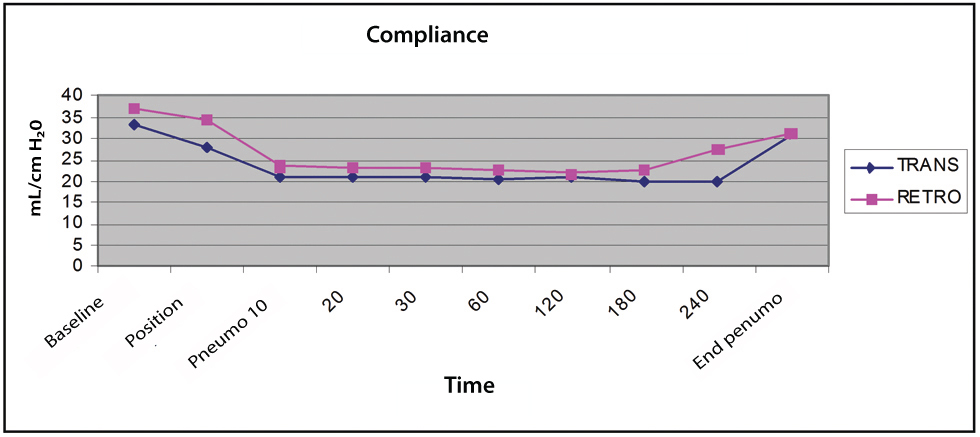
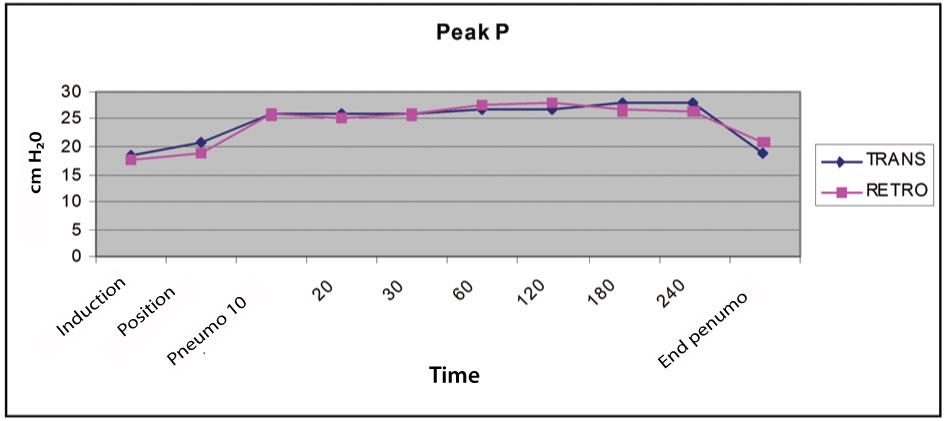
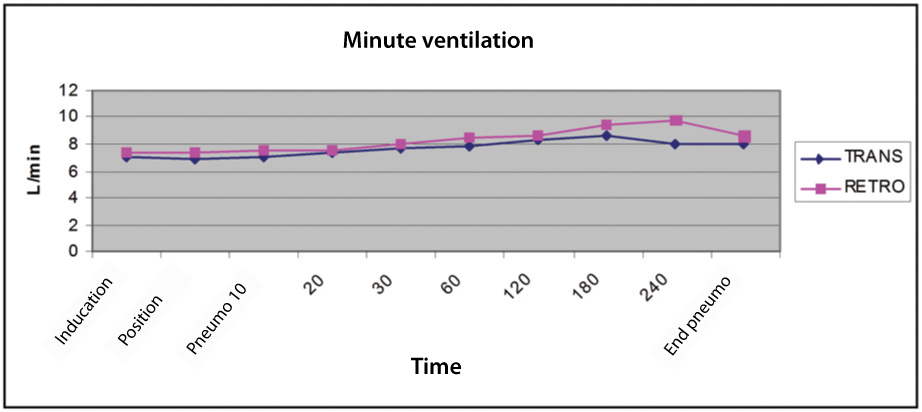
There was drop in compliance after giving lateral positon which further decreased after pneumoperitoneum in both the groups [Table/Fig-5]. The compliance remained same throughout insufflation period and again came near to baseline after desufflation in Trans group (from 33.03±6.9 to 30.57±9.7) however, not in Retro group (37.02±9.06 to 31±8.4). Simultaneously, PIP increased after insufflation, remained increased during insufflation and decreased after desufflation [Table/Fig-6]. The MV needed to be increased to compensate for the increase in EtCO2 during pneumoperitoneum in both the groups [Table/Fig-7]. Difference between compliance, PIP and MV at various interval between Trans and Retro group were statistically insignificant (p>0.05).
Comparison of compliance.
Comparison of peak inspiratory pressure.
Comparison of minute ventilation.
Value of PaO2/FiO2 was comparable in both the groups at baseline which was taken after induction of general anaesthesia however, before insufflation. The PaO2/FiO2 value after desufflation was less in both the groups as compared to baseline however, significantly lower in Retro group as compared to Trans group (p<0.05) [Table/Fig-8]. PaCO2-ETCO2 difference increased in both the groups at the end of surgery as compared to baseline. There was no statistical significant difference in PaCO2-ETCO2 value between the two groups at baseline as well as at the end of pneumoperitoneum (p>0.05) [Table/Fig-8].
PaO2/FiO2 (P/F) ratio and PaCO2-EtCO2 difference
| Trans | Retro | p-value |
|---|
| P/F ratio baseline | 395.45±128.35 | 399.29±57.6 | 0.898 |
| P/F ratio at the end | 439.88±87.77 | 349.72±97.89 | 0.0022* |
| PaCO2-EtCO2 difference baseline | 4.66±4.03 | 4.52±4.61 | 0.915 |
| PaCO2-EtCO2 difference at the end | 6.28±5.99 | 8.05±6.77 | 0.359 |
T-test was used to calculate p-value.
*p-value (<0.05) statistically significant.
Discussion
Pneumoperitoneum affects the various organ systems by physical pressure on these systems and also due to the systemic absorption of the CO2. The increased intra-abdominal pressure results in splinting and cephalad shifts of the diaphragm leading to an absolute decrease in functional residual capacity, decrease in lung compliance and increase in Ventilation/Perfusion ratio (V/Q) mismatch in different parts of the lung with preferential ventilation of nondependent regions [8,9]. The outcome is compromised oxygenation and ventilation which may lead to hypoxia and hypercarbia, respectively. The basic differences between the two approaches related to anaesthesia are; exposure to surface area, lateral position and pneumoperitoneum pressure over one or both diaphragm.
In the present study, partial pressure of oxygen in the blood decreased more after desufflation in the Retro group as compared to Trans group which was similar at the start of surgery between the two groups. There is no unanimity with regard to the effect of lateral position on arterial oxygenation under anaesthesia. Brismar B et al., found fall in PaO2 in lateral position compared to supine under general anaesthesia [10]. Manikandan S and Umamaheswara Rao GS compared the effect of supine, lateral and prone positions on pulmonary gas exchange in neurosurgical patients [11]. Lateral and prone positions improved the oxygenation as compared to supine position. Fujise K et al., studied the effects of lateral position on cardiopulmonary function in 15 transperitoneal renal surgeries [12]. There were no significant changes in Pulmonary Shunt Fraction (Qs/Qt) and PaO2/PAO2, at any point in the study. In the present study average PaO2/FiO2 improved from 395.45 at baseline to 439.88 at the end of desufflation in Trans group while it decreased from 399.29 to 349.72 at the end desufflation in Retro group. Comparing the two groups, difference of PaO2/FiO2 at the end of desufflation between the two groups was statistically significant (p=0.0022). This might be due to the difference in patient positioning between the two approaches. In transperitoneal approach, lateral position is given with angle of aroung 60°-80° without break down of operation table at flank level. While in retroperitoneal approach the patient is given 90° lateral position with flexion at flank and elevation of kidney rest. Nonetheless, this difference was clinically insignificant as none of the patient developed respiratory complication perioperatively.
It is a matter of debate that which approach is associated with higher CO2 absorption. A retrospective study in 63 laparoscopic urologic surgeries by Wolf JS et al., concluded that CO2 absorption is higher with retroperitoneal approach and in patients who developed subcutaneous emphysema [13]. While a prospective study by Ng CS et al., in 51 patients had different outcome [5]. Retroperitoneoscopy was not associated with greater CO2 absorption compared to transperitoneal laparoscopy. Striech B et al., compared three groups with 10 patients in each group; laparoscopic cholecystectomy, extraperitoneal renal surgeries and open orthopaedic surgeries as control [3]. They found that Retro group had higher CO2 absorption due to dissection of loose areolar tissue in retroperitoneal space. Though, we did not compared the CO2 absorption between the two approaches, MV needed to increase to compensate for systemic CO2 absorption in both the groups. The MV was increased gradually at first, second and third hour of pneumoperitoneum in both the groups suggesting that CO2 absorption increase with time.
In the present study, PIP increased 45% of baseline and compliance decreased 35% of baseline after creation of pneumoperitoneum in both the groups without statistical significance. In a study done by Nadu A et al., in 39 renal surgeries, compliance decreased 50% in Trans group requiring change in ventilatory mode from Volume Control Ventilation (VCV) to Pressure Control Ventilation (PCV) in 50% patients of Trans group [6]. They conclude ventilatory changes are less affected with retroperitoneal approach as compared to transperitoneal approach.
In the present study, during the insufflation period, mean HR remained higher Trans group than in Retro group. However, it was statistically insignificant (p>0.05). The MAP remained higher than baseline throughout the insufflation period in both the groups without any significant difference. Thus, haemodynamic variables were comparable between the two groups. In animal studies, while Giebler RM et al., and Bannenberg JJ et al., found less haemodynamic impairment with extraperitoneal CO2 insufflation [14,15]. Baird JE et al., found stable haemodynamics in both approaches [7]. The HR, systolic and diastolic BP remained higher in transperitoneal approach than in retroperitoneal approach in a study done by Nadu A et al., [6]. Haemodynamic changes with CO2 insufflation depend on patient position, volume status, anaesthetic agents, arterial CO2 pressure, transthoracic pressure and transabdominal pressure of insufflated CO2. Complex interaction between these factors can give different outcome in different patient.
Limitation
The present study has several limitations. First, this is not the randomised study. Therefore, level of evidence of present study will be inferior compared to randomised study. Second, surgeons operating on patients of present study had different level of experience. Third, apart from various nephrectomies, pyeloplasty and ureterolithotomy were also included in present study. These factors could have affected the results of present study.
Conclusion
Retroperitoneal organs can be operated through either trans or retroperitoneal approach. We conducted a prospective non randomised comparative study in 45 patients underwent laparoscopic urologic surgeries to evaluate the respiratory and haemodynamic changes when either transperitoneal or retroperitoneal approach is used. Both the approaches are safe. The present study may help in deciding which approach to choose, especially in patients with compromised respiratory and cardiovascular functions. Larger studies are required to validate present results.
*p-value<0.05 is statistically significant, mins-Minutes
T-test was used to calculate p-value.
*p-value (<0.05) statistically significant.
[1]. Garg M, Singh V, Sinha RJ, Sharma P, Prospective randomized comparison of transperitoneal vs retroperitoneal laparoscopic simple nephrectomyUrology 2014 84(2):335-39.10.1016/j.urology.2014.04.03824975713 [Google Scholar] [CrossRef] [PubMed]
[2]. Taue R, Izaki H, Koizumi T, Kishimoto T, Oka N, Fukumori T, Transperitoneal versus retroperitoneal laparoscopic radical nephrectomy: a comparative studyInt J Urol 2009 16(3):263-67.10.1111/j.1442-2042.2008.02219.x19087210 [Google Scholar] [CrossRef] [PubMed]
[3]. Streich B, Decailliot F, Perney C, Duvaldestin P, Increased carbon dioxide absorption during retroperitoneal laparoscopyBr J Anaest 2003 91(6):793-76.10.1093/bja/aeg27014633746 [Google Scholar] [CrossRef] [PubMed]
[4]. Demiroluk S, Salihoglu Z, Bakan M, Bozkurt P, Effects of intraperitoneal and extraperitoneal carbon dioxide insufflation on blood gases during the perioperative period.J Laparoendosc Adv Surg Tech 2004 14(4):219-22.10.1089/lap.2004.14.21915345159 [Google Scholar] [CrossRef] [PubMed]
[5]. Ng CS, Gill IS, Sung GT, Whalley DG, Graham R, Schweizer D, Retroperitoneoscopic surgery is not associated with increased carbon dioxide absorptionJ Urol 1999 162(4):1268-72.10.1016/S0022-5347(05)68262-6 [Google Scholar] [CrossRef]
[6]. Nadu A, Ekstein P, Szold A, Friedman A, Nakache R, Cohen Y, Ventilatory and haemodynamic changes during retroperitoneal and transperitoneal laparoscopic nephrectomy: a prospective real-time comparisonJ Urol 2005 174(3):1013-17.10.1097/01.ju.0000169456.00399.de16094033 [Google Scholar] [CrossRef] [PubMed]
[7]. Baird JE, Granger R, Klein E, Warriner CB, Phang PT, The effects of retroperitoneal carbon dioxide insufflation on haemodynamics and arterial carbon dioxideAm J Surg 1999 177(2):164-66.10.1016/S0002-9610(98)00326-2 [Google Scholar] [CrossRef]
[8]. Bardoczky GI, Engelman E, Levarlet M, Simon P, Ventilatory effects of pneumoperitoneum monitored with continuous spirometryAnaesthesia 1993 48:309-11.10.1111/j.1365-2044.1993.tb06949.x8494131 [Google Scholar] [CrossRef] [PubMed]
[9]. Rauh R, Hemmerling TM, Rist M, Jacobi KE, Influence of neumoperitoneum and patient positioning on respiratory system complianceJ Clin Anaesth 2001 13:36110.1016/S0952-8180(01)00286-0 [Google Scholar] [CrossRef]
[10]. Brismar B, Hedensteirna G, Lundquist H, Strandberg A, Svensson L, Tokics L, Pulmonary densities during anaesthesia with muscle relaxation–a proposal of atelectasisAnaesthesiology 1985 62(4):422-28.10.1097/00000542-198504000-000093885791 [Google Scholar] [CrossRef] [PubMed]
[11]. Manikandan S, Umamaheswara Rao GS, Effect of surgical position on pulmonary gas exchange in neurosurgical patientsIndian J Anaesth 2002 46(5):356-59. [Google Scholar]
[12]. Fujise K, Shingu K, Matsumoto S, Nagata A, Mikami O, Matsuda T, The effects of the lateral position on cardiopulmonary function during laparoscopic urological surgeryAnesth Analg 1998 87(4):925-30.10.1097/00000539-199810000-000349768796 [Google Scholar] [CrossRef] [PubMed]
[13]. Wolf JS, Monk TG, McDougall EM, McClennan BL, Clayman RV, The extraperitoneal approach and subcutaneous emphysema are associated with greater absorption of carbon dioxide during laparoscopic renal surgeryJ Urol 1995 154(3):959-63.10.1016/S0022-5347(01)66943-X [Google Scholar] [CrossRef]
[14]. Giebler RM, Kabatnik M, Stegen BH, Scherer RU, Thomas M, Peters J, Retroperitoneal and intraperitoneal CO2 insufflation have markedly different cardiovascular effectsJ Surg Res 1997 68(2):153-60.10.1006/jsre.1997.50639184674 [Google Scholar] [CrossRef] [PubMed]
[15]. Bannenberg JJ, Rademaker BM, Froeling FM, Meijer DW, Haemodynamics during laparoscopic extra- and intraperitoneal insufflationAn experimental study. Surg Endosc 1997 11(9):911-14.10.1007/s0046499004859294271 [Google Scholar] [CrossRef] [PubMed]