Gastric Tuberculous Ulcer Perforation Presenting as Acute Peritonitis
Zeineb Mzoughi1, Slim Zribi2, Sana Ben Slama Mallouli3, Dhouha Bacha4, Mohamed Taher Khalfallah5
1 Medical Doctor, Faculty of Medicine of Tunis, Tunis El Manar University, Tunis, Tunisia; Department of General Surgery, Mongi Slim Hospital, Sidi Daoud La Marsa, Tunisia.
2 Medical Doctor, Faculty of Medicine of Tunis, Tunis El Manar University, Tunis, Tunisia; Department of General Surgery, Mongi Slim Hospital, Sidi Daoud La Marsa, Tunisia.
3 Medical Doctor, Faculty of Medicine of Tunis, Tunis El Manar University, Tunis, Tunisia; Department of Anatomopathology, Mongi Slim Hospital, Sidi Daoud La Marsa, Tunisia.
4 Medical Doctor, Faculty of Medicine of Tunis, Tunis El Manar University, Tunis, Tunisia; Department of Anatomopathology, Mongi Slim Hospital, Sidi Daoud La Marsa, Tunisia.
5 Professor, Faculty of Medicine of Tunis, Tunis El Manar University, Tunis, Tunisia; Department of General Surgery, Mongi Slim Hospital, Sidi Daoud La Marsa, Tunisia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Zeineb Mzoughi, Medical Doctor, Department of General Surgery, Centre Hospitalier Universitaire Mongi Slim, Sidi Daoud, Tunis, Tunisia.
E-mail: mzeineb@yahoo.com
Koch’s bacillus infection is a rare cause of gastric ulcer. Gastric perforation associated with tuberculosis cvery rarely presented as generalised peritonitis. A 39-year-old patient presented with epigastralgia with fever for one week. The physical examination found a generalised abdominal defense. Computed tomography evoked the diagnosis of perforated duodenal ulcer. The patient was operated and a suture excision of a perforated gastric ulcer was performed. The mesentery contained multiple lymph nodes. The small intestine was uniformly carded. The histopathological examination showed a gastric tuberculous ulcer. Acute peritonititis complicating tuberculous duodenal ulcer should be considered especially in endemic area. Clinical history, abdominal CT scan results, and intraoperative exploration should suggest this diagnosis which has therapeutic implications.
Intestinal, Peritoneum, Tuberculosis, Ulceration
Case Report
A 39-year-old male patient presented to the Emergency Department for epigastralgia of sudden appearance occurring on the background of fever lasting one week. He reported an unquantified weight loss in the last six months.
The patient had history of smoking two packs per day for the last 10 years. The examination found a fever of 100.4°F and a generalised abdominal defense. The laboratory test found leukocytosis at 18000/mm3. The chest X-ray showed no parenchymal pulmonary abnormalities or pneumoperitoneum.
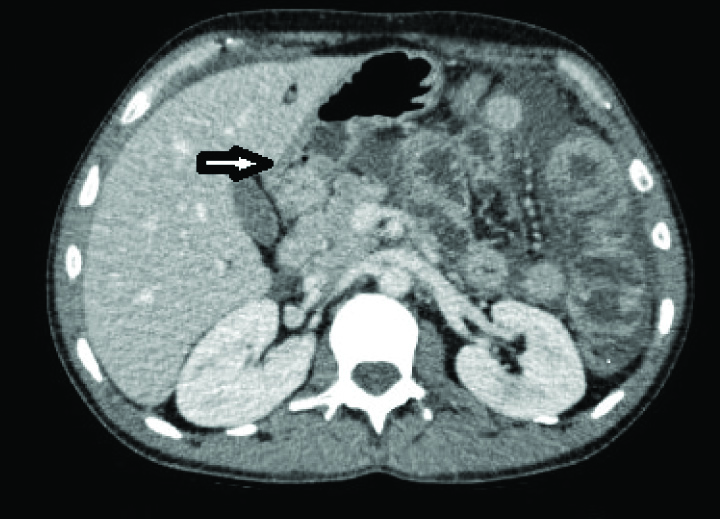
The abdominal computed tomography showed abdominal effusion in great abundance with nodular and irregular thickening of the parietal peritoneum and an extra luminal bull near the antrum, suggesting perforated duodenal ulcer [Table/Fig-1].
An abdominal effusion of great abundance with a nodular and irregular thickening of the parietal peritoneum and an extra luminal bull near the antrum (black arrow).
The patient was operated first with a laparoscopic approach which found a generalised peritonitis with abundant purulent effusion and false layers. The peritoneal fluid was prelevated and sent for bacteriological examination. The exploration was difficult because of multiple adhesions and thickened, fragile small intestine. A median conversion was decided. There was a 2 cm perforation on the anterior aspect of the antrum. The mesentery contained multiple adenopathies. The small intestine was uniformly carded. We performed a suture excision of this perforated gastric ulcer. An adenopathy located on the mesentery was taken and sent for histopathological examination.
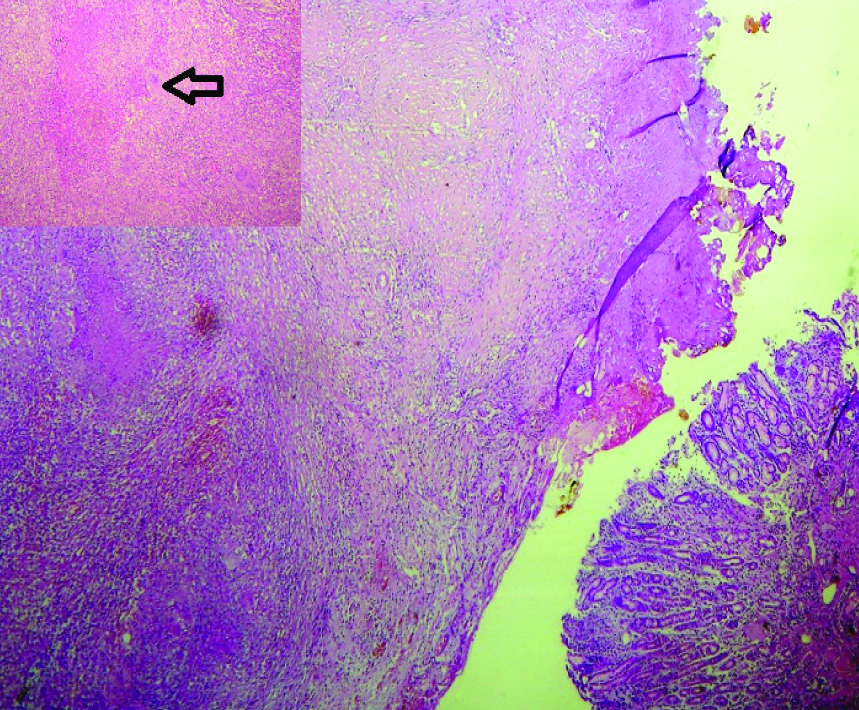
The histopathological examination of both gastric tissue around the ulcer and the lymph node, showed epithelioid and giganto-cellular tuberculoid granulomas with caseous necrosis confirming the diagnosis of tuberculous gastric perforation [Table/Fig-2]. Koch’s bacillus was not isolated from the abdominal effusion.
Histological image showing ulceration (top, left) with deep tuberculoid granulomas. Adjacent gastric mucosa (bottom right) (H&E x100).
The postoperative outcomes were uneventful. The postoperative assessment (clinical examination, CT scan, search for Koch’s bacillus in sputum and urine) did not find any other tuberculous sites, particularly pulmonary tuberculosis. An anti-tuberculosis quadritherapy was started.
The patient had no fever or any abdominal signs at six-month follow-up.
Written informed consent was obtained from the patient for publication of this case report and any accompanying image.
Discussion
Koch’s bacillus infection is a rare cause of gastric ulcer [1]. Gastric tuberculosis has been described as a pseudotumoural or obstructive lesion, most of the times [2,3].
Intestinal perforation is the doubtable complication of abdominal Koch’s bacillus chronic infection [4,5]. Gastric tuberculosis associated with perforation is extremely rare (five cases reported in the literature) [6,7]. In these cases, patients were young (mean age 35 years), with male to female ratio of 4:2. The diagnosis was confirmed by the presence of acid fast bacilli on culture specimen of the gastric biopsy or the caseating necrosis in the lymph nodes. In one case, the Mycobacterium tuberculosis culture was positive on peritoneal fluid and gastric biopsy specimen [6].
Because of peritoneal adhesions in abdominal tuberculosis, clinical presentation is rarely described as generalised peritonitis. Similarly, clinical findings in perforated tuberculous duodenal ulcer, has been reported in only one case [8]. In these circumstance, it is all the more difficult to preoperatively suspect the diagnosis of tuberculosis. Weight loss with nocturnal sweats and adenopathy in the abdominal CT scan contributes to the diagnosis.
In peroperative care, the absence of sclerotomatosis and intestinal lesions consistent with Crohn’s disease (stenosis, fistulae), and the presence of lymph nodes were evoking gastric tuberculosis in the present case [9].
Suspecting perforated gastric tuberculosis makes it possible to limit the gesture to excision of the ulcer (for pathological examination) and suture. Treatment of the bacilli infection should be done by anti-tuberculosis drugs. For the cases described in literature, total or partial gastrectomy was performed in most of the cases (four cases) [7]. All these patients died postoperatively. In one case, conservative approach was considered keeping in mind the high mortality rate of gastric resection. The patient died by associated pulmonary tuberculosis despite no surgical complications [6].
The intraoperative data may be helpful to direct the anatomo-pathologist towards the search for granulomas and caseous necrosis [10].
The postoperative management involves isolation of the patient with a complete tuberculosis check-up and medical treatment based on anti-tubercular drugs.
Conclusion
All the elements of the digestive tract can be affected by abdominal tuberculosis. Gastric perforation associated with tuberculosis is very rarely described as generalised peritonitis. This aetiology may have therapeutic and operative implications.
[1]. Espinoza-Rios J, Bravo Paredes E, Pinto Valdivia J, Guevara J, Huerta-Mercado J, Tagle Arrospide M, Penetrating gastric ulcer as a manifestation of multisystemic tuberculosisRev Gastroenterol Peru 2017 37(1):91-93. [Google Scholar]
[2]. Ghadimi Moghadam A, Alborzi A, Pouladfar G, Monabati A, Primary gastric tuberculosis mimiking gastric cancer: a case reportJ Infect Dev Ctries 2013 7(4):355-57.10.3855/jidc.259823592646 [Google Scholar] [CrossRef] [PubMed]
[3]. Padmanabhan H, Rothnie A, Singh P, An unusual case of gastric outlet obstruction caused by tuberculosis: challenge in diagnosis and treatmentBMJ Case Rep 2013 doi:10.1136/bcr-2012-00827710.1136/bcr-2012-00827723704423 [Google Scholar] [CrossRef] [PubMed]
[4]. Wani RA, Parray FQ, Bhat NA, Wani MA, Bhat TH, Farzana F, Non traumatic ileal perforationWorld J Emerg Surg 2006 1:710.1186/1749-7922-1-716759405 [Google Scholar] [CrossRef] [PubMed]
[5]. Afridi SP, Malik F, Ur-Rahman S, Shamim S, Samo KA, Spectrum of perforation peritonitis in Pakistan: 300 cases eastern experienceWorld J Emerg Surg 2008 3:3110.1186/1749-7922-3-3118992164 [Google Scholar] [CrossRef] [PubMed]
[6]. Gill RS, Gill S, Mangat H, Logsetty S, Gastric perforation associated with tuberculosis: a case reportCase Report Med 2011 2011:39276910.1155/2011/39276921629804 [Google Scholar] [CrossRef] [PubMed]
[7]. Sharma D, Gupta A, Jain BK, Agrawal V, Dargan P, Upreti L, Tuberculous gastric perforation: report of a caseSurg Today 2004 34(6):537-41.10.1007/s00595-004-2745-115170553 [Google Scholar] [CrossRef] [PubMed]
[8]. Berney T, Badaoui E, Totsch M, Mentha G, Morel P, Duodenal tuberculosis presenting as acute ulcer perforationAm Gastroenterol 1998 93:1989-91.10.1111/j.1572-0241.1998.00564.x9772074 [Google Scholar] [CrossRef] [PubMed]
[9]. Almadi MA, Ghosh S, Aljebreen AM, Differentiating intestinal tuberculosis from Crohn’s disease: a diagnostic challengeAm J Gastroenterol 2009 104(4):1003-12.10.1038/ajg.2008.16219240705 [Google Scholar] [CrossRef] [PubMed]
[10]. Sabooni K, Khosravi MH, Pirmohammad H, Afrasiabian S, Moghbl N, Shahverdi E, Tuberculosis peritonitis with features of acute abdomen in HIV infectionInt J Mycobacteriol 2015 4(2):151-53.10.1016/j.ijmyco.2015.02.00426972884 [Google Scholar] [CrossRef] [PubMed]