Mucormycosis is a potentially fatal fungal infection caused by a group of molds called mucormycetes. Rhino-Orbital-Cerebral Mucormycosis (ROCM) represents nearly half of all cases. This is the case of a 46-year-old female recently diagnosed with leukaemia and was started on chemotherapy. After initiating chemotherapy, she complained of headache, blurring of vision in the right eye, nasal discharge. Examinations revealed orbital apex syndrome. MRI disclosed an inflammation affecting the right orbit, ethmoid sinus and the frontal lobe. Ethmoidectomy was performed and biopsies confirmed mucormycosis. After that, symptoms persisted and complete loss of vision in her right eye occurred. Right orbital exenteration was required. The response was noticed over the subsequent weeks until she became asymptomatic. Five weeks after initially being diagnosed with leukaemia, she entered remission and was discharged on oral itraconazole and oral retinoic acid. Later, she remained in complete remission. In conclusion, early suspicion and diagnosis especially in immunocompromised patients with early aggressive treatment can be life saving.
Case Report
A 46-year-old female recently diagnosed with Acute Myeloid Leukaemia (AML) M3 by Department of Haematology developed an abrupt right-sided headache associated with monocular blurring of vision in the right eye and a nasal discharge one week after starting chemotherapy. Ophthalmological assessment revealed swelling, proptosis, decreased visual acuity, limitation in extraocular movements and a Relative Afferent Pupillary Defect (RAPD) involving the right eye. There was no evidence of papilloedema. ENT examination showed blockage of the middle meatus and a purulent discharge in the right nostril. Neurological evaluation showed normal power, tone and reflexes. Investigations were unremarkable with the exception of neutropenia.
An MRI showed an inflammatory process affecting the entire right orbit with thickening of the medial and lateral rectus muscles and compression of the optic nerve. Involvement of the right ethmoid sinus with extension to the base of the frontal lobe was also noted. These findings prompted discontinuation of chemotherapy and an urgent right external ethmoidectomy with decompression of the optic nerve.
Samples taken from ethmoidal sinus and nasal discharge were examined under microscope in 10% KOH wet mounts. It showed broad, non septate hyphae branching at right angle which raised the suspicion of mucormycosis infection. Fungal culture was identified using Sabouraud’s Dextrose Agar (SDA) media. White abundant colonies were grown after eight days, which were sensitive to amphotericin B, caspofungin, and fluconazole. The colonies were examined under microscopy using Lactophenol Cotton Blue (LCB) mount which revealed Rhizopus species. The patient was started on amphotericin B 50 mg IV daily.
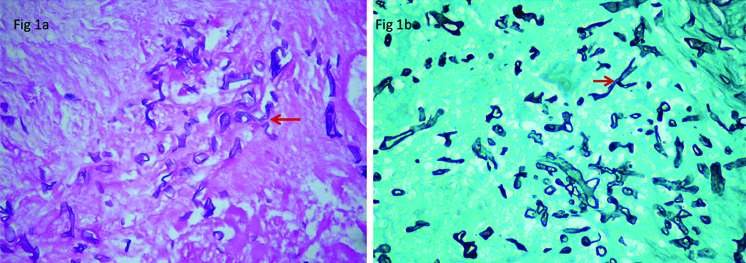
The fungal infection was further confirmed with histopathological examination. Right ethmoidal tissue sample, which was stained by Hematoxylin and Eosin Stain (H&E) and Grocott’s Methenamine Silver Stain (GMS), showed oedema and aggregation of dilated broad non septate hyphae in the subepithelial stroma consistent with mucormycosis [Table/Fig-1].
a) Histological section of mucomycosis with broad branching non septate hyphae (H&E, 400X); b) Hyphae branching at right angle consistent with mucormycosis (GMS, 400X).
On the third postoperative day chemotherapy was resumed with the addition of Granulocyte-Colony Stimulating Growth Factor (G-CSF). However, her previous symptoms persisted and progressed over the ensuing week and complete loss of vision occurred. Repeat ophthalmological examination showed a dilated, non reactive pupil, oculomotor apraxia, prolapse of the conjunctiva and severe papilloedema with pallor of the optic disc in the right eye. A repeat MRI showed worsening of the inflammatory collection that now involved the entire right orbit along with the globe, all sinuses and increased extension in the base of the frontal lobe.
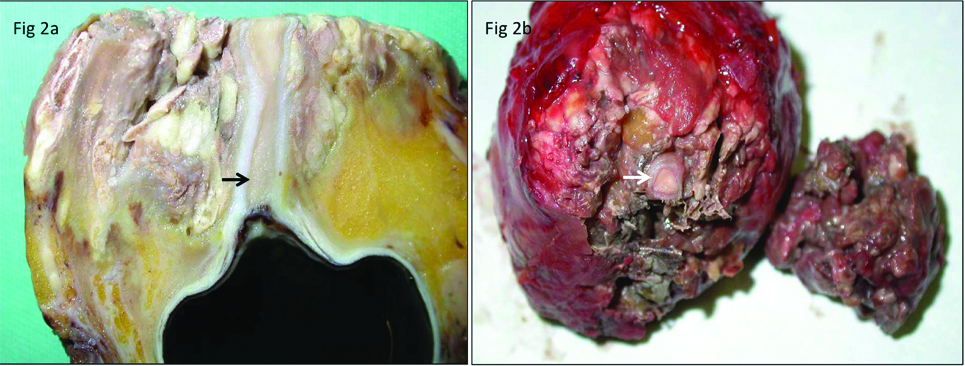
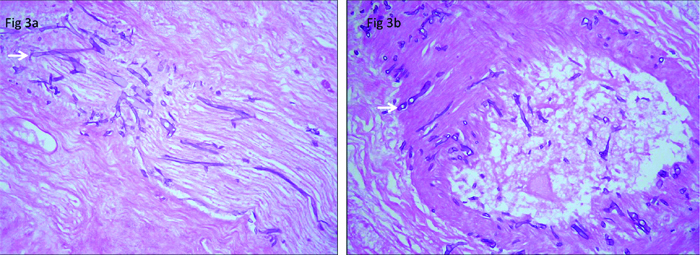
A multidisciplinary meeting between Ophthalmology, ENT, Neurosurgery, Infectious Diseases, and Oncology was conducted and it was decided that the patient should undergo right orbital exenteration and functional endoscopic sinus surgery with debridement and clearance of all collections as well as the continuation of her chemotherapy postoperatively [Table/Fig-2]. Repeated intraoperative samples of posterior orbital contents and nasal sinuses showed extensive necrosis, infiltration of inflammatory cells and presence of numerous branching non septate hyphae within the necrotic tissue, and demonstrated prominent angioinvasion [Table/Fig-3]. Infectious diseases team recommended the addition of itraconazole 200 mg q12 to the current medications.
a) The right eye globe post exenteration with greyish-white friable necrotic tissue surrounding optic nerve indicated by arrow; b) Posterior orbital necrotic tissue surrounding optic nerve.
a) Neural invasion by fungal hyphae (H&E, 400X); b) Vascular wall invasion by fungal hyphae (H&E, 400X).
She showed response to treatment over the next two weeks until she was asymptomatic. Five weeks after being initially diagnosed with AML, a repeat bone marrow biopsy and aspirate showed she was in remission. She was discharged on oral itraconazole 200 mg BID for six months and maintenance chemotherapy. On subsequent visits she remained asymptomatic without recurrence of AML or mucormycosis.
Discussion
Mucormycosis is the third most common fungal infection following candidiasis and aspergillosis, found during autopsies [1]. It is a rare opportunistic infection that may be lethal especially in immunocompromised hosts [2,3]. Mortality rates range from 24% to 49% [4]. It may reach 80% if diagnosis and treatment are delayed [5]. Predisposing factors include diabetes, haematological malignancies, chronic steroid use, chronic renal insufficiency, hepatic cirrhosis, burns, trauma, iron and aluminum overload, intravenous drug abuse and following solid organ or bone marrow transplantation [2,3]. Roden MM et al., found diabetes mellitus to be the most common predisposing factor in contrast to Skiada A et al., who demonstrated haematological malignancies to be the most prevalent [6,7]. The current patient had been diagnosed with AML and initiation of chemotherapy rendered her neutropenic one week prior to developing mucormycosis.
It can present with rhino-orbital-cerebral, pulmonary, gastrointestinal, cutaneous, or disseminated disease [1]. ROCM represents about 50% of cases [3]. Clinical picture varies from non invasive sinusitis in immunocompetent patients to severe invasive disease in immunocompromised patients. In its invasive picture, fungal infection is typically inhaled into the nasal cavity and paranasal sinuses and causes necrotising vasculitis of the nose and sinuses, then rapidly spreads into the orbits, deep face, meninges, and cranial cavity by osseous erosion, direct soft-tissue invasion, and angioinvasion [8]. This usually leads to suppurative arteritis, vascular thrombosis, and infarction of the surrounding tissues [8]. Classically, ROCM is heralded by bloody nasal discharge and black nasal eschar [9]. Also, it usually presents with proptosis, ptosis, periretro-orbital pain, eye discharge, ophthalmoplegia, diplopia, pupil dilatation, blurry vision, acute vision loss, chemosis, headache, fever, lethargy and altered levels of consciousness [1-3].
Diagnosis of mucormycosis requires histopathological demonstration of the causative organism, sputum cultures and bronchoalveolar washings may also be used [3]. Early detection can be attained by direct KOH microscopic examination, which demonstrates the presence of non septate hyaline hyphae, with right-angled irregular branching [10]. Prompt initiation of medical therapy and surgical debridement of necrotic tissue have been shown to reduce the three-month mortality rate from 83% to 49% [11]. Early diagnosis and aggressive multidisciplinary therapy are paramount for successful treatment.
Current guidelines indicate that the first line of therapy is amphotericin B and for cases with central nervous system involvement it has been demonstrated to be superior to other medications [4]. If resistance or intolerance to amphotericin B is encountered, posaconazole is recommended [4]. Local administration of antifungals following debridement of non viable tissue may overcome reduced efficacy of systemic antifungals due to the decreased tissue perfusion associated with mucormycosis [12].
The present patient developed ROCM with orbital apex syndrome, which is a rare condition that stems from invasion and subsequent infarction of the ophthalmic artery and the optic, oculomotor, trochlear, abducens nerves as well as the ophthalmic branch of the trigeminal nerve. It is characterised by sudden loss of vision, ophthalmoplegia, proptosis, optic atrophy and diplopia as occurred initially in our patient [13]. In the present case, the patient developed orbital apex syndrome rapidly just after initiation of chemotherapy. Despite early efforts to preserve her right eye with medical and surgical interventions, the infection progressed. Following invasion of the right eye globe and complete loss of vision, exenteration was required.
Exenteration, when ophthalmoplegia and blindness have occurred may be life saving [14]. In a review of 35 cases of ROCM, 42% of patients had extensive orbital involvement requiring exenteration, 82% of these cases survived [15]. Our patient showed no improvement following initial surgery, but ultimately following functional loss of her right eye, exenteration and change of antifungal aided improvement in the patient’s condition and survival tremendously.
Other treatment options include hyperbaric oxygen therapy which when combined with standard therapy has shown significant increase in the survival rate [3]. G-CSF and granulocyte transfusions also demonstrated a statistically significant benefit in patients with neutropenia [3]. The underlying cause of immunosuppression must be addressed when applicable, in the current patient chemotherapy was interrupted after mucormycosis developed and G-CSF was used, when a response to medical and surgical interventions was realised chemotherapy was resumed.
Conclusion
Mucormycosis is a time sensitive diagnosis that should be suspected in immunocompromised patients who present with acute and non specific ophthalmic or sinusoidal symptoms. Early and aggressive use of antifungal therapy with surgical interventions including orbital exenteration when orbital involvement is extensive may be life saving. Frequent, multidisciplinary assessment and collaboration are necessary for best outcomes.
[1]. Petrikkos G, Skiada A, Lortholary O, Roilides E, Walsh TJ, Kontoyiannis DP, Epidemiology and clinical manifestations of mucormycosisClin Infect Dis 2012 54(Suppl 1):S23-34.10.1093/cid/cir86622247442 [Google Scholar] [CrossRef] [PubMed]
[2]. Koc Z, Koc F, Yerdelen D, Ozdogu H, Rhino-orbital-cerebral mucormycosis with different cerebral involvements: infarct, hemorrhage, and ophthalmoplegiaInt J Neurosci 2007 117(12):1677-90.10.1080/0020745060105023817987470 [Google Scholar] [CrossRef] [PubMed]
[3]. Prabhu RM, Patel R, Mucormycosis and entomophthoramycosis: a review of the clinical manifestations, diagnosis and treatmentClin Microbiol Infect 2004 10(Suppl 1):31-47.10.1111/j.1470-9465.2004.00843.x14748801 [Google Scholar] [CrossRef] [PubMed]
[4]. Cornely OA, Arikan-Akdagli S, Dannaoui E, Groll AH, Lagrou K, Chakrabarti A, ESCMID and ECMM joint clinical guidelines for the diagnosis and management of mucormycosis 2013Clinical Microbiology and Infection 2014 20(Suppl 3):5-26.10.1111/1469-0691.1237124479848 [Google Scholar] [CrossRef] [PubMed]
[5]. Ganesh R, Manikumar S, Vasanthi T, Rhinocerebral mucormycosis in an adolescent with type 1 diabetes mellitus: case reportAnn Trop Paediatr 2008 28(4):297-300.10.1179/146532808X37547719021947 [Google Scholar] [CrossRef] [PubMed]
[6]. Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, Epidemiology and outcome of zygomycosis: a review of 929 reported casesClin Infect Dis 2005 41(5):634-53.10.1086/43257916080086 [Google Scholar] [CrossRef] [PubMed]
[7]. Skiada A, Pagano L, Groll A, Zimmerli S, Dupont B, Lagrou K, Zygomycosis in Europe: analysis of 230 cases accrued by the registry of the European Confederation of Medical Mycology (ECMM) Working Group on Zygomycosis between 2005 and 2007Clin Microbiol Infect 2011 17(12):1859-67.10.1111/j.1469-0691.2010.03456.x21199154 [Google Scholar] [CrossRef] [PubMed]
[8]. Kohn R, Hepler R, Management of limited rhino-orbital mucormycosis without exenterationOphthalmology 1985 92(1):1440-44.10.1016/S0161-6420(85)33844-7 [Google Scholar] [CrossRef]
[9]. Yohai RA, Bullock JD, Aziz AA, Markert RJ, Survival factors in rhino-orbitalcerebral mucormycosisSurv Ophthalmol 1994 39(1):3-22.10.1016/S0039-6257(05)80041-4 [Google Scholar] [CrossRef]
[10]. Bonifaz A, Vázquez-González D, Tirado-Sánchez A, Ponce-Olivera RM, Cutaneous zygomycosisClin Dermatol 2012 30:413-19.10.1016/j.clindermatol.2011.09.01322682190 [Google Scholar] [CrossRef] [PubMed]
[11]. Chamilos G, Lewis RE, Kontoyiannis DP, Delaying amphotericin B-based frontline therapy significantly increases mortality among patients with hematologic malignancy who have zygomycosisClin Infect Dis 2008 47(4):503-09.10.1086/59000418611163 [Google Scholar] [CrossRef] [PubMed]
[12]. DiBartolo MA, Kelley PS, Rhino-orbital-cerebral mucormycosis (ROCM): a comprehensive case reviewAviat Space Environ Med 2011 82(9):913-16. [Google Scholar]
[13]. Schlemmer F, Lagrange-Xelot M, Lacroix C, de La Tour R, Socie G, Molina JM, Breakthrough Rhizopus infection on posaconazole prophylaxis following allogeneic stem cell transplantationBone Marrow Transplant 2008 42(8):551-52.10.1038/bmt.2008.19918622416 [Google Scholar] [CrossRef] [PubMed]
[14]. Ferry AP, Abedi S, Diagnosis and management of rhino-orbitocerebral mucormycosis (phycomycosis). A report of 16 personally observed casesOphthalmology 1983 90(9):1096-104.10.1016/S0161-6420(83)80052-9 [Google Scholar] [CrossRef]
[15]. Bhansali A, Bhadada S, Sharma A, Suresh V, Gupta A, Singh P, resentation and outcome of rhino-orbital-cerebral mucormycosis in patients with diabetesPostgrad Med J 2004 80(949):670-74.10.1136/pgmj.2003.01603015537854 [Google Scholar] [CrossRef] [PubMed]