Introduction
Because of new evidence on several diagnostic and therapeutic aspects of hypertension (HTN), the present guidelines (ESH/ESC 2013) differ from the 2007 ones in several points [1]. The important part is update of the prognostic significance of asymptomatic organ damage, as there is an increase attention to organ damage-guided therapy [2,3]. Owing to the importance of asymptomatic organ damage, as an intermediate stage in the continuum of CVD, signs of organ involvement should be sought carefully by appropriate techniques [4].
Taking into consideration this recommendation, early diagnosis of subclinical LV systolic dysfunction is of a great importance because it is the hallmark for the progression of the HTN [5,6]. Some studies suggest that minimal systolic impairment in longitudinal contraction of the LV, could be found in patients with HTN especially when EF is still preserved, despite of diastolic function [7,8].
Speckle tracking echocardiography is a new method for evaluation of the global and regional myocardial function [9]. A fundamental advantage over Tissue Doppler Echocardiography (TDE) is the independence from the angle of penetration of the ultrasound beam [10]. The method is based on the principle of tracking a group of dots (speckles) with similar echo density in the myocardium [11]. Each group moves from frame-to-frame and a special software tracks and calculates the velocities and the deformational parameters [12-14].
Two-dimensional STE-derived GLS (2D-STE GLS) appears to be reproducible and feasible for clinical use and offers incremental prognostic data over LV EF in a variety of cardiac conditions including HTN, although, measurements vary among vendors and software versions [15,16]. The Global Longitudinal Strain (GLS) represents the global LV function. To provide some guidance, a peak GLS in the range of -20% can be expected in a healthy person, and the lower the absolute value of strain is below this value, the more likely it is to be abnormal [17].
Two-dimensional STE GLS can help to unmask early subclinical LV systolic dysfunction of newly diagnosed hypertensive patients without left ventricular hypertrophy [18]. Special care should be given to this patient group through the early initialized treatment, targeted at the organ damage protection [4].
In this study, we investigated subclinical LV systolic dysfunction on the basis of reduced 2D-STE GLS among hypertensive patients with preserved EF aiming to identify a high-risk group for developing a HF.
Materials and Methods
This was a single center, case-control study conducted on two populations (hypertensive patients and healthy controls). Subjects were randomly selected between March 2014 and January 2016 from outpatient and inpatient of the Cardiology Clinic at Military Medical Academy, Sofia, Bulgaria. This study and consent procedure were approved by local ethics committee (Protocol number BA218/15.02.14), and were carried out in accordance with the principles of the Declaration of Helsinki. The participants received information about the study methods and procedures and gave their written informed consent. The patients files were stored at the hospital electronic database. Assessment of participants was performed by experienced cardiologists using a standard protocol including a physical examination, an ECG, and the standard laboratory blood tests. Exclusion criteria for participation were signs and symptoms of coronary heart disease, reduced EF, congestive HF, more than a mild valvular heart disease, rhythm and conduction disturbances, and age above 55 years. All participants were in sinus rhythm and had a preserved LV EF. The definitions and classification of the office BP (mmHg) from the recent ESH/ESC Guidelines for the management of HTN were accepted [4].
In this study, 150 subjects were enrolled, including 80 patients with HTN (41±4 years) and 70 age and gender matched healthy controls (37±8 years). According to the protocol, subjects with HTN were divided in three groups taking into consideration the stage of HTN: mild HTN without DD (HTN I DD0; n=12), moderate HTN with two grades DD-impair relaxation or pseudonormalization (HTN II DD1,2; n=33), and severe HTN with all the grades DD (HTN III DD1,2,3; n=35). Each of these groups were compared with age-and gender-matched healthy controls (C I; n=10; C II; n=28; C III; n=32). All patients with HTN were treated by monotherapy or double or triple combination of the anti-hypertensive drugs according to the recent ESH/ESC guidelines for the management of HTN [Table/Fig-1] [4].
Antihypertensive treatment of the patients, mono/or combinations.
| HTN (n=80) | HTN I (DD 0) n=12 | HTN II (DD1,2) (n=33) | HTN III (DD1,2,3) n=35 |
|---|
| ACEi | 5 | | |
| ARB | 4 | 1 | |
| BB | 3 | 1 | |
| ACEi/CA | | 7 | 2 |
| ARB/CA | | 6 | 2 |
| ACEi/D | | 6 | 3 |
| ARB/D | | 5 | 2 |
| ACEi/BB | | 4 | 3 |
| ARB/BB | | 3 | 2 |
| ACEi/CA/D | | | 6 |
| ARB/CA/D | | | 7 |
| ACEi/CA/BB | | | 4 |
| ARB/CA/BB | | | 4 |
HTN-Hypertension, HTN I-Mild hypertension, HTN II-Moderate hypertension, HTN III-Severe hypertension, DD-Diastolic dysfunction DD0-Preserved diastolic function, DD1-Impaired relaxation, DD2-Pseudonormalization, DD3-Restriction,
ACEi-Angiotensin-converting enzyme inhibitors, ARB-Angiotensin receptor blockers, BB-Beta-blockers, D-Diuretics, CA-Calcium antagonistsbiplane
Echocardiography was performed in a left lateral decubitus position, using a GE Vivid I digital imaging ultrasound system, equipped with Phased-Arrayed 1.6-3.6 MHz transducer. Quantification of the LV dimensions and volumes was done using M-mode, and the antagonistsbiplane modified Simpson’s method respectively. LV mass in grams was calculated according to Devereux formula, and then, was normalized for BSA to obtain LV Mass Index (LVMI). LV Hypertrophy (LVH) was investigated by LVMI. The EF was assessed using the biplane Simpson’s method and assumed to be preserved when it was equal or more than 52% for male and equal or more than 54% for female [17]. Left atrial (LA) volume was calculated using the biplane disk method and indexed to BSA to obtain the LA Volume Index (LAVI) [17].
The recent recommendations for the evaluation of LV diastolic function by echocardiography was used [19]. The diagnostic approach includes mainly PW Doppler of the transmitral blood flow together with TDE of the mitral annulus. It was assessed the E/A ratio, ΔE/A during Valsalva, LAVI, PAS and E/e’ where e´ is averaged from the septal and lateral mitral annulus.
MAPSE was assessed by placing M-mode cursor through medial and lateral mitral annulus; maximum systolic displacement was measured and then, the mean of medial and lateral mitral annular excursion was calculated.
Online pulsed TDE was done in the apical four chamber view by placing the sample volume over the septal and lateral mitral annulus, and then, the peak systolic velocity (Sm), early diastolic velocity (Em), and late diastolic velocity (Am) were measured. The average velocity of the septal and lateral mitral annulus were estimated, and the E/e’ ratio was calculated.
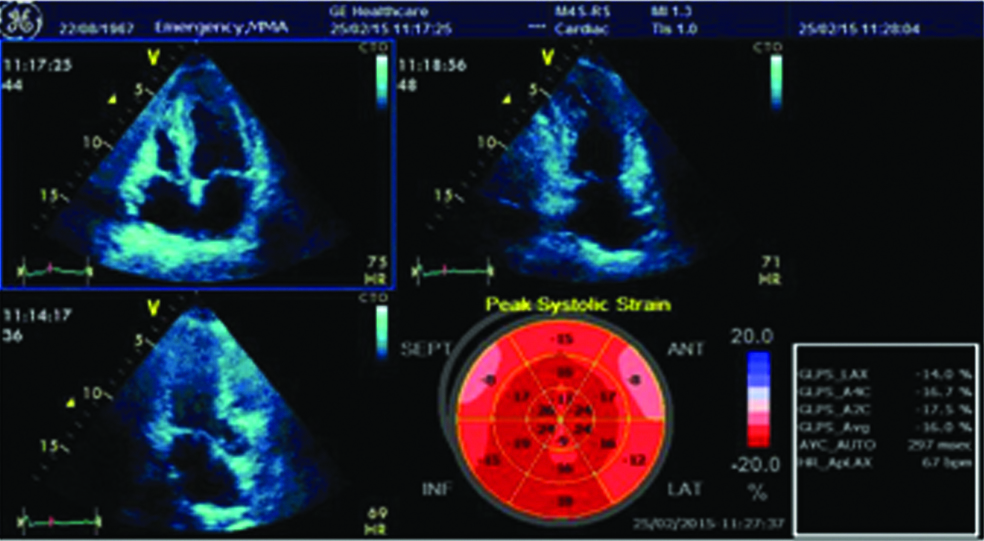
A2D-STE GLS: After optimizing image quality, maximizing frame rate, and minimizing foreshortening, which are all critical to reduce measurement variability, investigations start with records of an images in the three standard apical views and averaged [16]. For the assessment of resting function, the recommended LV midwall tracking were accepted as more reproducible [20-22]. The software used Region of Interest (ROI) by three-point system consecutively for the mitral annulus and the apex. Then, the software tracked the myocardial speckles, frame by frame and generated moving images. Visual inspection allowed to determine the adequacy of the tracking. When the tracking was not accurate, the investigator returned back and readjusted the ROI. If the tracking is already correct, then software divided the LV myocardium into six segments in each view and generates segmental and Global Longitudinal Strain (GLS). As the myocardium usually shortened in longitudinal direction during end-systole, the longitudinal strain was displayed below the baseline. From these curves, peak systolic longitudinal strain was recorded for each of the myocardial segments. The strain values for all the segments were recorded and averaged to obtain the GLS, and also “bull’s eye” was displayed in a 17-segment model. Subclinical LV systolic dysfunction was approved to be defined as reduced 2D-STE GLS <-20% [17]. A less negative value corresponds to a more impaired GLS [Table/Fig-2].
This picture presents the calculation of a 2D-STE GLS of a patient with HTN.
Reduced mean GLS (-16%) and the presence of subclinical LV systolic dysfunction are observed. It is also well visible a concentric LVH.
GLS-Global longitudinal strain, LV-Left ventricle, LVH-Left ventricular hypertrophy, GLPS_LAX-Global longitudinal peak strain in long axis view (A3C), GLPS_A4C-Global Longitudinal peak strain in apical four chamber view, GLPS_A2C-Global longitudinal peak strain in apical two chamber view, GLPS_Avg-Global longitudinal peak strain averaged, AVC Auto-time to aortic valve closure, HR_ApLAX-Heart rate
When regional tracking is suboptimal in more than two myocardial segments in a single view, the calculation of GLS to be avoided was the recommended approach, accepted in the study [17]. In such cases, alternatively to gain insight into longitudinal LV function, MAPSE or pulsed TDE-derived mitral annular Sm was used.
Statistical Analysis
The statistical analysis was performed using MedCalc® Version 10.2.0.0. Windows 7 pro. The significance level was set at p<0.05. Unpaired t-test was used to assess categorical data. Comparison between proportions was performed by chi-square test. To determine the strength of the correlation between the variables, the Pearson’s correlation coefficient (r) was used. Continuous variables and their association with age and gender were assessed using multiple regression analysis. Inter-and intra-observer variability were assessed using Intraclass Correlation Coefficient (ICC).
Results
Clinical and demographic data are presented in [Table/Fig-3]. No significant differences were found between the groups in terms of age or gender, laboratory data or smoking status. Patients with HTN had significantly higher BMI, systolic and diastolic BP than the control group (p<0.001).
Demographic and clinical characteristics of the participants in the study.
| Variable | Patients with HTN ** n(%) | Control group** n(%) | p-value* |
|---|
| Participants (n=;%) | 80 (53%) | 70 (47%) | 0.464 |
| HTN I DD 0 (n=;%) | 12 (15%) | 10 (14.3%) | 0.578 |
| HTN II DD 1,2 (n=;%) | 33 (41.3%) | 28 (40%) | 0.874 |
| HTN III DD 1,2,3 (n=;%) | 35 (43.7%) | 32 (45.7%) | 0.935 |
| Systolic BP (mmHg) | 140±25 | 115±10 | <0.001 |
| Diastolic BP (mmHg) | 85±15 | 70±10 | <0.001 |
| Age (years) | 41±4 | 37±8 | =0.735 |
| Gender/male (n=;%) | 38 (47%) | 18 (26%) | =0.138 |
| BMI | 33.4±5.2 | 27.3±3.1 | <0.001 |
| Smoking (n=;%) | 29 (36%) | 18 (26%) | =0.480 |
| DM (n=;%) | 13 (16%) | 7 (10%) | =0.710 |
| Dyslipidemia (n=;%) | 39 (49%) | 14 (20%) | =0.06 |
| Microalbuminuria (n=;%) | 18 (22%) | 1 (1.4%) | =0.631 |
| Anemia (n=;%) | 5 (6%) | 1 (1.4%) | =0.863 |
Significance level was set at p< 0.05, by use of unpaired t-test for variables expressed as mean±SD or chi-square test for the comparison of two independent samples, expressed as a percentage.
** Values are presented as mean ± SD or proportion.
HTN-Hypertension, HTN I-Mild hypertension, HTN II-Moderate hypertension, HTN III-Severe hypertension, DD-Diastolic dysfunction DD0-Preserved diastolic function, DD1-Impaired relaxation, DD2-Pseudonormalization, DD3-Restriction, BMI-Body mass index; HTN-Hypertension; BP-Blood pressure; DM-Diabetes mellitus
Conventional echocardiography data are listed in [Table/Fig-4]. Significantly higher wall thickness in HTN patients was found (p=0.01). Also, the LVMI and LAVI were significantly higher in the HTN group (p<0.001). However, the MAPSE showed significant reduction of the values and considerable differences with controls (p=0.02), except for the patients with mild HTN (p=0.019). Tissue Doppler data showed, that Sm was significantly lower (p=0.01), and E/e’ ratio was significantly higher (p<0.001) in the HTN patients with DD. In subjects with mild HTN, non significant reduction of Sm (p=0.046) and normal E/e’ were found. There was a non significant difference in the EF between the two groups (p=0.110/0.187/0.485).
Comparison of echocardiographic findings in patients with different stages of HTN and control group. The echo-data for the control group are presented in the first column as the mean value. For each stage of HTN, from the age-and gender matched controls p-values were calculated.
| Variables | Controls** n=70 | HTN I (DD0) **n=12 | p-value* (n=10 controls) | HTN II(DD1,2) **N=33 | p-value* (n=28 controls) | HTN III(DD1,2,3) **n=35 | p-value* (n=32 controls) |
|---|
| IVSd (mm) | 8.1±1.3 | 9±1.3 | 0.121 | 11±1.3 | <0.001 | 12±1.3 | <0.001 |
| LVPWd (mm) | 8.3±2.1 | 7.2±2.1 | 0.235 | 9.5±2.1 | 0.034 | 10±2.1 | <0.001 |
| LVED (mm) | 48±3.6 | 47±3.6 | 0.523 | 49±3.6 | 0.284 | 47±3.6 | 0.260 |
| LVES (mm) | 30.5±3.6 | 31±2.1 | 0.688 | 32±3.6 | 0.110 | 31±2.1 | 0.485 |
| EDV (ml) | 93.5±25.4 | 98.3±25.4 | 0.663 | 105.3±25.4 | 0.075 | 102.5±25.4 | 0.152 |
| ESV (ml) | 35.7±15.4 | 40.3±15.4 | 0.493 | 41.3±15.4 | 0.141 | 38.3±15.4 | 0.492 |
| EF of LV (%) | 62.0±3.5 | 59.5±3.5 | 0.110 | 60.8±3.5 | 0.187 | 62.6±2.0 | 0.485 |
| LVMI (gr/m2) | 74.1±12 | 85.5±12 | 0.038 | 110.5±12 | <0.001 | 123.5±12 | <0.001 |
| MAPSE (mm) | 16.4±1.1 | 15.2±1.1 | 0.019 | 12.7±1.1 | <0.001 | 10.7±1.9 | <0.001 |
| LAVI (ml/m2) | 18.9±2.6 | 22.4±4.6 | 0.090 | 29.4±4.6 | <0.001 | 32.9±4.6 | <0.001 |
| E/A | 1.25±0.4 | 1.12±0.4 | 0.456 | 1.14±0.4 | 0.288 | 1.06±0.4 | 0.265 |
| Sm (cm/sec) | 10.5±1.1 | 9.5±1.1 | 0.046 | 8.3±1.1 | <0.001 | 7.28±1.1 | <0.001 |
| E/e’ | 7.56±2.14 | 6.35±2.14 | 0.201 | 8.8±2.14 | 0.027 | 11.4±2.14 | <0.001 |
* Significance level was set at p<0.05, by use of unpaired t-test.
** Values are presented as mean ± SD.
HTN-Hypertension, HTN I-Mild hypertension, HTN II-Moderate hypertension, HTN III-Severe hypertension, DD-Diastolic dysfunction DD0-Preserved diastolic function, DD1-Impaired relaxation, DD2-Pseudonormalization, DD3-Restriction, LVPW-Left ventricle posterior wall, LVED and LVES-Left ventricle end-diastolic and end-systolic diameters, EDV and ESV-End-diastolic and end-systolic volumes of the LV, EF-Ejection fraction of the LV, LVMI-LV Muscle mass indexed to body surface area, MAPSE-Mitral annular plane systolic excursion, LAVI-Left atrial volume indexed to body surface area
It was observed that grade of HTN and stage of DD influent on longitudinal contraction of the LV. The patients with mild HTN had non-significant reduction of the GLS, compared to the age and gender matched controls (p=0.840). GLS was significantly attenuated in patients with HTN and DD (p<0.001). A stepwise difference in terms of reduction of the GLS depending on the grade of HTN and stage of DD was observed [Table/Fig-5].
Two dimensional-STE GLS data set. Comparison of the patients with HTN and controls. The GLS data of the control group are presented in the first column as the mean value. For each stage of HTN, p-values were calculated from the age-and gender matched controls.
| Variables | Controls** n=70 | HTN I(DD0) ** n=12 | p-value* n=10 | HTN II(DD1,2) ** n=33 | p-value * n=28 | HTN III (DD1,2,3) ** n=35 | p-value * n=32 |
|---|
| 2D-STE GLS | −20.75±2.4 | −20.54±2.4 | 0.840 | −17.41±2.4 | <0.001 | −16.26±2.4 | <0.001 |
* Significance level was set at p<0.05, by use of unpaired t-test.
** Values are presented as mean±SD.
HTN-Hypertension, HTN I-Mild hypertension, HTN II-Moderate hypertension, HTN III-Severe hypertension, DD-Diastolic dysfunction DD0-Preserved diastolic function, DD1-Impaired relaxation, DD2-Pseudonormalization, DD3-Restriction, 2D-STE GLS-Two dimensional speckle tracking echocardiography global longitudinal strain.
In 68 of 80 patients (85%) in the HTN group, subclinical LV systolic dysfunction was found. In two of 70 controls (2.9%) reduced GLS was observed, and attribute this to smoking, passive smoking, dyslipidemia, unknown genetic causes, or premature atherosclerosis. This rate may also be attributed to the small study sample size. Multivariate analysis was used to determine the influence of many factors as age, gender, BMI, EF, diastolic function and values of the BP. At this point, it can be concluded that the statistical significance (p=0.038) prove the lack of clinical significance of this group. Despite the controls with reduced GLS were excluded from the analysis, the aforementioned example should take into consideration as an important exception in clinical practice [Table/Fig-6].
Two dimensional-STE GLS data. Comparative analysis of the hypertensive patients vs. age-and gender-matched healthy controls.
| Variables | HTN group** n=80 | Control group** n=70 | p-value* |
|---|
| 2D-STE GLS | -16.84±2.4 | -20.75±2.4 | <0.001 |
| Normal systolic function | 12 (15%) | 68 (97.1%) | <0.001 |
| Subclincal dysfunction | 68 (85%) | 2 (2.9%) | =0.038 |
* Significance level was set at p<0.05, by use of unpaired t-test for variables expressed as mean±SD or Chi-square test for the comparison of two independent samples, expressed as a percentage.
** Values are presented as mean±SD or proportion.
GLS-Global longitudinal strain, 2D-STE-Two dimensional speckle tracking echocardiography. subclinical LV Systolic dysfunction corresponds to 2D-STE GLS <-20%
Using multivariate analysis, in patients with HTN and reduced GLS, increased BMI (p<0.001), higher values of the LAVI (p<0.001) and the LVMI (p<0.001), reduced Sm (p=0.01) and MAPSE (p=0.02) were found. A moderate negative correlation between GLS and BMI (r=-0.52; p<0.001) as well as GLS and LVMI (r=-0.61; p<0.001) were observed. A moderate positive correlation between GLS and EF (r=0.48; p=0.03), and GLS and Sm (r=0.56; p=0.01), as well as strong positive correlation between GLS and MAPSE (r=0.756; p=0.003) were also observed.
To assess the reliability of the measurements, Intraclass Correlation Coefficient (ICC) was used. The results are summarized in [Table/Fig-7].
Data base set about the reliability of the measurements.
| Participants (n=70) | ICC (1 observer) | 95% CI | Strength of agreement | ICC (2 observers) | 95% CI | Strength of agreement |
|---|
| Single measures | | Average measures | |
| Healthy (n=10) | 0.8358 | 0.7324 ÷ 0.8167 | Very good | 0.8478 | 0.6953 ÷ 0.9240 | Very good |
| HTN I (DD0) (n=10) | 0.7256 | 0.5132 ÷ 0.8655 | Good | 0.8476 | 0.6834 ÷ 0.9354 | Very good |
| HTN II DD(1,2) (n=10) | 0.7951 | 0.6834 ÷ 0.8419 | Good | 0.8811 | 0.7983 ÷ 0.9294 | Very good |
| HTN III (DD1,2,3) (n=10) | 0.8140 | 0.7038 ÷ 0.9109 | Very Good | 0.8129 | 0.7129 ÷ 0.9279 | Good |
Analysing the results, we can conclude that 2D-STE GLS demonstrates good and very good inter-and intra-observer reproducibility.
Discussion
Several studies have shown that the regression of asymptomatic organ damage occurring during treatment reflects the treatment-induced reduction of morbid and fatal CV events, thereby offering valuable information on whether patients are more or less effectively protected by the treatment strategies adopted. This has been shown for the treatment-induced regression of LVH, LVM and left atrial size [23-28]. It would be of some interest to receive guidance from organ damage studies, but unfortunately this information must be judged with great caution [29-31].
In patients with HTN, the systolic function of the LV is considered normal, if the EF and the shortening fraction are preserved. However, these measurements reflect the global contractility of the LV in a wide spectrum, without taking into consideration the earliest changes in the segmental kinetics, which are the first sign of organ damage. According to the used method, the EF reflects the function of the radial and circumferential myocardial fibers, when Teichholz is used or of all fibers, when the biplane method of Simpson is used. The function of the longitudinal myocardial fibers is not independently investigated in any of the above methods. This is important, because in some heart diseases, the longitudinal fibers are the first to be affected. The reason for the long-standing preserved EF in patients with HTN is the supernormal work of the radial and circumferential myocardial fibers, which compensate for the reduced contraction of the longitudinal fibers. This is the rationale to use 2D-STE GLS for more precise diagnosis of the subclinical LV systolic dysfunction, even instead of TDE and MAPSE where exists dependence of the angle of ultrasound penetration [17].
It is necessary to take into consideration, the fact that in the evolution of the disease, there is a long-standing period, during which there is no evidence of change in the contractility. At first, minimal changes can be found in patients with moderate HTN and initial compromise of the diastolic function of the LV. The more the HTN advances and the diastolic function worsen, the more significant the changes in the contractility become. As a rule, the EF stays preserved until the more advanced stages of HTN.
To avoid the effect of the aging, myocardium on the values of GLS, the patients with age above 55 years were excluded, from participation in this study. According to the results, the GLS is reduced in patients with HTN and DD in comparison to the control group. Despite the normal EF of the LV, in these participants, there is evidence for the presence of subclinical LV systolic dysfunction. A gradual reduction of the GLS, which is dependent on the stage of HTN and the severity of DD was observed. The more severe the HTN and DD respectively, the more significant is the reduction of the GLS. The mild HTN showed non significant change in the GLS. This is the strong evidence in favour of an aggressive therapy to be started, before the hard-to-overcome morphological changes in the LV, have developed.
The results showed that in 2.9% of the healthy volunteers, there is a reduction of the GLS, a fact which is hard for interpretation, but most likely is due to the increased rates of tobacco smoking and dyslipidemia among the controls. Regardless of the insignificant number of controls with reduced GLS, the clinical evaluation should always have the priority before examination of the patient with 2D-STE GLS.
In patients with HTN, the diagnosis of subclinical LV systolic dysfunction can be made by a few echocardiographic methods [16-18]. Reproducibility of the measurements is closely related to quality of images, because STE is very sensitive in case of poor image quality. Alternative method is MAPSE or as an exception Sm obtained from pulsed TDE [32-35]. In case of a good image quality, no doubt the contemporary method is 2D-STE GLS [36,37]. The result of the present study is in consistent with the data received from recent studies. Two of them are of Imbalzano E et al., who determined that the GLS is reduced in all patients with HTN, independently form the LVH, and the study of Saghir M et al., who prove that patients with HTN and LVH have significantly reduced GLS [7,38]. In another study, Madaik T et al., found that LVMI and diastolic BP are independent predictors for reduced GLS [18]. Narayanan A et al., reported similar results [11]. According to results of present study, LVH and increased LVMM respectively, are predictors for reduced GLS. Lavie C et al., have determined that HTN is found in approximately 50% of the patients with obesity [39]. The effect of the two diseases on the remodeling of the LV is dependent on the duration. The HTN leads to the development of concentric LVH, which increases in obesity. Ballo P et al., in a study conducted on 112 patients with HTN, determined moderate negative correlation between BMI and myocardial strain [40]. In our study we found that the BMI is significantly higher in patients with reduced GLS in comparison with the controls. These results show that the increase of BMI in patients with HTN is associated with higher LVMM and significantly increases the probability for the development of subclinical LV systolic dysfunction. It can be concluded that increased BMI is an independent predictor of reduced GLS in HTN. The importance of its modification can potentially prevent LV systolic dysfunction in HTN patients together with antihypertensive treatment and lifestyle changes.
In a study by Matos J et al., reported that MAPSE is an independent predictor of the EF in HTN, and that this parameter should be used routinely in clinical practice, especially in low image quality [32]. In our study, the patients with HTN and DD had significantly lower values of MAPSE in comparison with the control group. The lowest values were observed in patients with severe HTN and DD or Sm derived from the pulsed TDE.
Some older studies reported another method that identified subclinical LV dysfunction in hypertensive patients who have evidence of target-organ damage, entitled midwall fractional shortening. The authors concluded that use of this method could identify a substantial subgroup among patients with HTN and reduced LV function who have concentric LVH, a pattern associated with high CV risk and increased mortality [41,42].
Regardless of what method is used for the diagnosis of subclinical LV systolic dysfunction, its analysis should be done only in the context of the whole clinical status and evaluation of the risk factors.
Limitation
This study was limited by the small sample size. Probably due to this reason some of the hypothesis could not be proved. Small sample size arises from the fact, that in the study included only young subjects with HTN, which are the target group for organ damage. The reason to enroll younger and middle aged participants is, to screen for early onset of target organ damage in HTN. As the population is younger and the organ damage is significant, the focus of interest is toward the long term protective therapy where the effect expects to be greater. As a future perspective, it is hoped to augment significantly, database with young and middle age hypertensive patients.
Another limitation was the method of examination. The principal method used was 2D-STE GLS and alternatively TDI and MAPSE. In order to be absolutely correct in the conclusions, 3D-STE was used or at least to map the circumferential strain and compare it to the longitudinal.
Conclusion
The study showed that 2D-STE GLS gives the opportunity for early diagnosis of a subclinical LV systolic dysfunction, in patients with HTN based on reduced GLS. In this way it’s possible to identify a group with a high risk for adverse CV events. An early and aggressive treatment, as well as control of risk factors and a lifestyle changes should be applied in this group, in order to avoid these unwanted events in future.
HTN-Hypertension, HTN I-Mild hypertension, HTN II-Moderate hypertension, HTN III-Severe hypertension, DD-Diastolic dysfunction DD0-Preserved diastolic function, DD1-Impaired relaxation, DD2-Pseudonormalization, DD3-Restriction,
ACEi-Angiotensin-converting enzyme inhibitors, ARB-Angiotensin receptor blockers, BB-Beta-blockers, D-Diuretics, CA-Calcium antagonistsbiplane
Significance level was set at p< 0.05, by use of unpaired t-test for variables expressed as mean±SD or chi-square test for the comparison of two independent samples, expressed as a percentage.
** Values are presented as mean ± SD or proportion.HTN-Hypertension, HTN I-Mild hypertension, HTN II-Moderate hypertension, HTN III-Severe hypertension, DD-Diastolic dysfunction DD0-Preserved diastolic function, DD1-Impaired relaxation, DD2-Pseudonormalization, DD3-Restriction, BMI-Body mass index; HTN-Hypertension; BP-Blood pressure; DM-Diabetes mellitus
* Significance level was set at p<0.05, by use of unpaired t-test.
** Values are presented as mean ± SD.HTN-Hypertension, HTN I-Mild hypertension, HTN II-Moderate hypertension, HTN III-Severe hypertension, DD-Diastolic dysfunction DD0-Preserved diastolic function, DD1-Impaired relaxation, DD2-Pseudonormalization, DD3-Restriction, LVPW-Left ventricle posterior wall, LVED and LVES-Left ventricle end-diastolic and end-systolic diameters, EDV and ESV-End-diastolic and end-systolic volumes of the LV, EF-Ejection fraction of the LV, LVMI-LV Muscle mass indexed to body surface area, MAPSE-Mitral annular plane systolic excursion, LAVI-Left atrial volume indexed to body surface area
* Significance level was set at p<0.05, by use of unpaired t-test.
** Values are presented as mean±SD.HTN-Hypertension, HTN I-Mild hypertension, HTN II-Moderate hypertension, HTN III-Severe hypertension, DD-Diastolic dysfunction DD0-Preserved diastolic function, DD1-Impaired relaxation, DD2-Pseudonormalization, DD3-Restriction, 2D-STE GLS-Two dimensional speckle tracking echocardiography global longitudinal strain.
* Significance level was set at p<0.05, by use of unpaired t-test for variables expressed as mean±SD or Chi-square test for the comparison of two independent samples, expressed as a percentage.
** Values are presented as mean±SD or proportion.GLS-Global longitudinal strain, 2D-STE-Two dimensional speckle tracking echocardiography. subclinical LV Systolic dysfunction corresponds to 2D-STE GLS <-20%
[1]. Mancia G, De Backer G, Dominiczak A, Fagard R, Germano G, Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)European Heart Journal 2007 28(12):1462-536. [Google Scholar]
[2]. Muiesan ML, Salvetti M, Paini A, Monteduro C, Galbassini G, Bonzi B, Inappropriate left ventricular mass changes during treatment adversely affects cardiovascular prognosis in hypertensive patientsHypertension 2007 49:1-7.10.1161/HYPERTENSIONAHA.107.08732017372030 [Google Scholar] [CrossRef] [PubMed]
[3]. Okin PM, Oikarinen L, Viitasalo M, Toivonen L, Kjeldsen SE, Nieminen MS, Serial assessment of the electrocardiographic strain pattern for prediction of new-onset heart failure during antihypertensive treatment: the LIFE studyEur J Heart Fail 2011 13:384-91.10.1093/eurjhf/hfq22421239405 [Google Scholar] [CrossRef] [PubMed]
[4]. Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, ESH/ESC Guidelines for the management of arterial hypertension. The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)European Heart Journal. 2013 34:2159-219.10.1093/eurheartj/eht15123771844 [Google Scholar] [CrossRef] [PubMed]
[5]. Daskalov IR, Daskalova IK, Demirevska LD, Atzev BG, The relationship between mitral annular systolic velocity and ejection fraction in patients with preserved global systolic function of the left ventricleBMC Cardiovascular Disorders 2013 13:9210.1186/1471-2261-13-9224160570 [Google Scholar] [CrossRef] [PubMed]
[6]. Daskalov IR, Petrovsky PD, Demirevska LD, Mitral annular systolic velocity as a marker of preclinical systolic dysfunction among patients with arterial hypertensionCardiovascular Ultrasound 2012 10:4610.1186/1476-7120-10-4623191932 [Google Scholar] [CrossRef] [PubMed]
[7]. Imbalzano E, Zito C, Carerj S, Oreto G, Mandraffino G, Cusmà-Piccione M, Left ventricular function in hypertension: new insight by speckle tracking echocardiographyEchocardiography 2011 28(6):649-57.10.1111/j.1540-8175.2011.01410.x21676016 [Google Scholar] [CrossRef] [PubMed]
[8]. Szymanski C, Lévy F, Tribouilloy C, Should LVEF be replaced by global longitudinal strain?Heart 2014 100(21)10.1136/heartjnl-2014-30618625049321 [Google Scholar] [CrossRef] [PubMed]
[9]. Mondillo S, Galderisi M, Mele D, Badano LP, Speckle-tracking echocardiography: [9]a new technique for assessing myocardial functionJ Ultrasound Med 2011 30(1):71-83.10.7863/jum.2011.30.1.7121193707 [Google Scholar] [CrossRef] [PubMed]
[10]. Voigt J, Pedrizzetti G, Lysyansky P, Marwick T, Houle H, Baumann R, Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imagingEuropean Heart Journa-Cardiovascular Imaging 2015 16(11):1-11.10.1093/ehjci/jeu18425525063 [Google Scholar] [CrossRef] [PubMed]
[11]. Narayanan A, Aurigemma GP, Chinali M, Hill JC, Meyer TE, Tighe DA, Cardiac mechanics in mild hypertensive heart disease: a speckle-strain imaging studyCirc Cardiovasc Imaging 2009 2(5):382-90.10.1161/CIRCIMAGING.108.81162019808626 [Google Scholar] [CrossRef] [PubMed]
[12]. Galderisi M, Lomoriello VS, Santoro A, Esposito R, Olibet M, Raia R, Differences of myocardial systolic deformation and correlates of diastolic function in competitive rowers and young hypertensives: a speckle-tracking echocardiography studyJ Am Soc Echocardiogr 2010 23:1190-98.10.1016/j.echo.2010.07.01020810245 [Google Scholar] [CrossRef] [PubMed]
[13]. Daskalov IR, Petrova VM, Examination of the myocardial mechanics by echocardiography. Clinical applications (Part II)Cardiovascular diseases 2016 1:3-7. [Google Scholar]
[14]. Gorcsan J, Tanaka H, Echocardiographic assessment of myocardial strainJACC 2011 58(14):1401-13.10.1016/j.jacc.2011.06.03821939821 [Google Scholar] [CrossRef] [PubMed]
[15]. Belghitia H, Brette S, Lafitte S, Reant P, Picard F, Serri K, Automated function imaging: a new operator-independent strain method for assessing left ventricular functionArchives of cardiovascular diseases 2008 101(3):163-69.10.1016/S1875-2136(08)71798-4 [Google Scholar] [CrossRef]
[16]. Mor-Avi V, Lang RM, Badano LP, Belohlavek M, Cardim MN, Derumeaux G, Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of EchocardiographyEur J Echocardiogr 2011 12:167-205.10.1093/ejechocard/jer02121385887 [Google Scholar] [CrossRef] [PubMed]
[17]. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular ImagingJ Am Soc Echocardiogr 2015 28:01-39.10.1016/j.echo.2014.10.00325559473 [Google Scholar] [CrossRef] [PubMed]
[18]. Madaik T, Negi P, Padam A, Gupta U, Subclinical systolic dysfunction among newly diagnosed hypertensives with preserved left ventricular ejection fraction using two dimensional strain imaging method; Hospital based observational studyNatl J Med Res 2014 4(1):27-32. [Google Scholar]
[19]. Nagueh S, Smiseth O, Appleton C, Byrd B, Dokainish H, Edvardsen T, Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the american society of echocardiography and the European association of cardiovascular imagingJ Am Soc Echocardiogr 2016 29:277-314.10.1016/j.echo.2016.01.01127037982 [Google Scholar] [CrossRef] [PubMed]
[20]. Yingchoncharoen T, Agarwal S, Popovic ZB, Marwick TH, Normal ranges of left ventricular strain: a meta-analysisJ am Soc Echocardiogr 2013 26:185-91.10.1016/j.echo.2012.10.00823218891 [Google Scholar] [CrossRef] [PubMed]
[21]. Mignot A, Donal E, Zaroui A, Reant P, Salem A, Hamon C, Global longitudinal strain as a major predictor of cardiac events in patients with depressed left ventricular function: a multicenter studyJ Am Soc Echocardiogr 2010 23(1):1019-24.10.1016/j.echo.2010.07.01920810243 [Google Scholar] [CrossRef] [PubMed]
[22]. Stanton T, Leano R, Marwick TH, Prediction of all-cause mortality from global longitudinal speckle strain: comparison with ejection fraction and wall motion scoringCirc Cardiovasc Imaging 2009 2:356-64.10.1161/CIRCIMAGING.109.86233419808623 [Google Scholar] [CrossRef] [PubMed]
[23]. Devereux RB, Wachtell K, Gerdts E, Boman K, Nieminen MS, Papademetriou V, Prognostic significance of left ventricular mass change during treatment of hypertensionJAMA 2004 292:2350-56.10.1001/jama.292.19.235015547162 [Google Scholar] [CrossRef] [PubMed]
[24]. Okin PM, Devereux RB, Jern S, Kjeldsen SE, Julius S, Nieminen MS, Regression of electrocardiographic left ventricular hypertrophy during antihypertensive treatment and the prediction of major cardiovascular eventsJAMA 2004 292(1):2343-49.10.1001/jama.292.19.234315547161 [Google Scholar] [CrossRef] [PubMed]
[25]. Fagard RH, Staessen JA, Thijs L, Celis H, Birkenhager WH, Bulpitt CJ, Prognostic significance of electrocardiographic voltages and their serial changes in elderly with systolic hypertensionHypertension 2004 44:459-64.10.1161/01.HYP.0000142169.17298.5415326091 [Google Scholar] [CrossRef] [PubMed]
[26]. Muiesan ML, Salvetti M, Paini A, Monteduro C, Galbassini G, Bonzi B, Inappropriate left ventricular mass changes during treatment adversely affects cardiovascular prognosis in hypertensive patientsHypertension 2007 49:1077-83.10.1161/HYPERTENSIONAHA.107.08732017372030 [Google Scholar] [CrossRef] [PubMed]
[27]. Okin PM, Oikarinen L, Viitasalo M, Toivonen L, Kjeldsen SE, Nieminen MS, Serial assessment of the electrocardiographic strain pattern for prediction of new-onset heart failure during antihypertensive treatment: the LIFE studyEur J Heart Fail 2011 13:384-91.10.1093/eurjhf/hfq22421239405 [Google Scholar] [CrossRef] [PubMed]
[28]. Gerdts AS, Wachtell AS, Omvik AS, Otterstad AS, Oikarinen AS, Boman AS, Sharma HS, Left atrial size and risk of major cardiovascular events during antihypertensive treatment: losartan intervention for endpoint reduction in hypertension trialHypertension 2007 49(1):311-16.10.1161/01.HYP.0000254322.96189.8517178978 [Google Scholar] [CrossRef] [PubMed]
[29]. Mancia G, Laurent S, Agabiti-Rosei E, Ambrosioni E, Burnier M, Caulfield MJ, Re-appraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force documentJ Hypertens 2009 27:2121-58.10.1097/HJH.0b013e328333146d19838131 [Google Scholar] [CrossRef] [PubMed]
[30]. Okin PM, Devereux RB, Jern S, Kjeldsen SE, Julius S, Nieminen MS, Regression of electrocardiographic left ventricular hypertrophy by losartan vs. atenolol: The losartan intervention for endpoint reduction in hypertension (LIFE) studyCirculation 2003 108:684-90.10.1161/01.CIR.0000083724.28630.C312885747 [Google Scholar] [CrossRef] [PubMed]
[31]. Fagard RH, Celis H, Thijs L, Wouters S, Regression of left ventricular mass by antihypertensive treatment: a meta-analysis of randomized comparative studiesHypertension 2009 54:1084-91.10.1161/HYPERTENSIONAHA.109.13665519770405 [Google Scholar] [CrossRef] [PubMed]
[32]. Matos J, Kronzon I, Panagopoulos G, Perk G, Mitral annular plane systolic excursion as a surrogate for left ventricular ejection fractionJ Am Soc Echocardiogr 2012 25(9):969-74.10.1016/j.echo.2012.06.01122795199 [Google Scholar] [CrossRef] [PubMed]
[33]. Hu K, Liu D, Herrmann S, Niemann M, Gaudron PD, Voelker W, Clinical implication of mitral annular plane systolic excursion for patients with cardiovascular diseaseEur Heart J Cardiovasc Imaging 2013 14(3):205-12.10.1093/ehjci/jes24023161791 [Google Scholar] [CrossRef] [PubMed]
[34]. Hu K, Liu D, Niemann M, Hermann S, Gaudron PD, Ertl G, Methods for assessment of left ventricular systolic function in technically difficult patients with poor imaging qualityJournal of the American Society of Echocardiography 2013 26(2):105-13.10.1016/j.echo.2012.11.00423257213 [Google Scholar] [CrossRef] [PubMed]
[35]. Bergenzaun1 L, Öhlin H, Gudmundsson P, Willenheimer R, Chew MS, Mitral annular plane systolic excursion (MAPSE) in shock: a valuable echocardiographic parameter in intensive care patientsCardiovascular Ultrasound 2013 11:1610.1186/1476-7120-11-1623718803 [Google Scholar] [CrossRef] [PubMed]
[36]. Yuda S, Inaba Y, Fujii S, Kokubu N, Yoshioka T, Sakurai S, Assessment of left ventricular ejection fraction using long-axis systolic function is independent of image quality: a study of tissue Doppler imaging and m-mode echocardiographyEchocardiography 2006 23(10):846-52.10.1111/j.1540-8175.2006.00331.x17069603 [Google Scholar] [CrossRef] [PubMed]
[37]. Yu CM, Sanderson JE, Marwick TH, Oh JK, Tissue Doppler Imaging: A new prognosticator for cardiovascular diseasesJournal of the American College of Cardiology 2007 49(19):1903-14.10.1016/j.jacc.2007.01.07817498573 [Google Scholar] [CrossRef] [PubMed]
[38]. Saghir M, Areces M, Makan M, Strain rate imaging differentiates hypertensive cardiac hypertrophy from physiologic cardiac hypertrophy (athlete’s heart)J Am Soc Echocardiogr 2007 20(2):151-57.10.1016/j.echo.2006.08.00617275700 [Google Scholar] [CrossRef] [PubMed]
[39]. Lavie C, Parto P, Archer E, Obesity, fitness, hypertension, and prognosis. Is physical activity the common denominator?JAMA Intern Med. 2016 176(2):217-18.10.1001/jamainternmed.2015.757126784456 [Google Scholar] [CrossRef] [PubMed]
[40]. Ballo P, Betti I, Barchielli A, Castelli G, De Luca L, Gheorghiade M, A Body mass index, gender, and clinical outcome among hypertensive and diabetic patients with stage A/B heart failureObesity 2013 21(9):500-07.10.1002/oby.2042023512886 [Google Scholar] [CrossRef] [PubMed]
[41]. De Simone G, Devereux RB, Roman MJ, Ganao A, Saba PS, Alderman MH, Assessment of left ventricular function by the midwall fractional shortening/ end-systolic stress relation in human hypertensionJournal of the American College of Cardiology 1994 23(6):1444-51.10.1016/0735-1097(94)90390-5 [Google Scholar] [CrossRef]
[42]. Schussheim A, Diamond J, Jhang J, Phillips R, Midwall fractional shortening is an independent predictor of left ventricular diastolic dysfunction in asymptomatic patients with systemic hypertensionThe American Journal of Cardiology 1998 8(9):1056-59.10.1016/S0002-9149(98)00558-X [Google Scholar] [CrossRef]