Introduction
Hospital stay is an important aspect of the medical care and most of the times medical professionals face this question at the very beginning when patient is advised indoor treatment. The role of Revised Trauma Score (RTS) and Paediatric Trauma Score (PTS) for initial screening of the trauma patients is very well established. However, there is a lack of data available on the correlation between hospital stay and different score in pediatric trauma patients.
Aim
The aim of the present study was to find which trauma score is better for prediction of length of hospital stay in paediatric trauma patients.
Materials and Methods
A prospective, observational study was conducted from January 2013 to December 2013, including Children less than 12 years with history of trauma and who required admission. Patients with burns, drowning, physical abuse were excluded. Data regarding demographics, vital parameters, Glasgow Coma Scale (GCS), laboratory parameters, number of days required for full recovery were recorded on case record proforma. Rapid respiratory rate of infant and toddler age group were adjusted before calculation of RTS. Revised Abbreviated injury score was used to calculate Injury Severity Score (ISS). The RTS, PTS were calculated based on parameters at admission. ISS was calculated after primary examination, radiological investigations and intraoperative findings.
Results
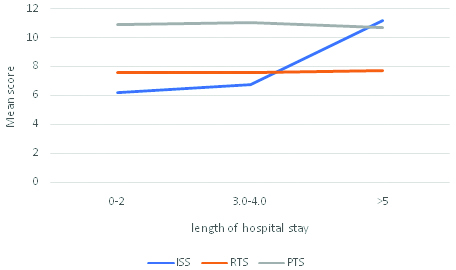
Mean ISS, RTS and PTS for 0-2 days of hospital admission was {(6.19±2.84), (7.59±0.41), (10.60±1.38)}, for 3-4 days it was {(6.72±3.40), (7.58±0.54), (11.03±1.42)} and for ≥5 days it was {(11.19±4.68), (7.69±0.54), (10.67±1.53)} respectively.
Conclusion
Length of hospital stay does not depend on physiological parameters on admission. There is a positive correlation between ISS and length of hospital stay. The ISS is a better predictor of length of hospital stay than PTS and RTS.
Introduction
Trauma is one of the major causes of morbidity and mortality [1]. Trauma surgeons can judge the outcome and hospital stay of the trauma patients based on their clinical acumen. Hospital stay is an important aspect of the medical care and most of the times medical professionals face this question at the very beginning when patient is advised indoor treatment. It was authors’ experience that some patients with severely deranged vital parameters on admission recover fast and some patients do not. In other words, different types of trauma can have the similar vital parameters on admission, but time required for recovery differs. For example, two patients with blunt abdominal trauma of the same age and same physical characteristics were presented to the emergency room with shock and loss of consciousness. One patient had mesenteric vascular injury and gross haemoperitoneum, other patient had pelvis fracture and internal haemorrhage. Both these patients were in haemorrhagic shock and had similar severely deranged vital parameters on admission but after surgery, the patient with mesenteric vascular injury recovered faster and patient with fractured pelvis required longer hospital stay. Another example: two patients with stable blood pressure, heart rate and GCS of E2M4V1 presented to the emergency, one patient had a large extradural haemorrhage and other patient had diffuse axonal injury. Both patients had similar parameters on admission but after surgery, the patient with extradural haematoma recovered faster than patient with diffuse axonal injury, who took more time to recover. Some trauma scores are based on physiological parameters e.g., RTS. Some are combination of both anatomical and physiological parameters e.g., PTS and ISS. Role of RTS and PTS for initial screening of the trauma patients is very well established [2].
Paediatric trauma score is a combination of anatomical and physiological trauma scoring system with six variables. Score varies between -6 to 12 [3]. Lesser score associated with more severe trauma [Table/Fig-1]. RTS is a physiological score which is revised version of trauma score. Score ranges between 0 to 12 [4]. Parameters are shown in [Table/Fig-2]. ISS was the first anatomical scoring system developed by Bakers and colleagues. It was not for the pre hospital triage but to compare the severity of the trauma in individual patients and to predict the outcome. The addition of square value of three maximum variables of abbreviated injury score was used to calculate ISS [5,6]. Subsequently, ISS has become important tool for prediction of the outcome and mortality. Score >16 was found to have 10% mortality and treatment of these patients was suggested in trauma care centres [7,8]. The present study was conducted to assess the length of hospital stay based on initial vital parameters by means of trauma scores.
| Component | Category |
|---|
| +2 | +1 | -1 |
|---|
| Weight | >20 kg (44 Lbs) | 10-20 kg (22-44 Lbs) | <10 kg (22 Lbs) |
| Airway | Patent | Maintainable | Unmaintainable |
| Systolic BP (mm Hg) | >90 | 50-90 | <50 |
| CNS | Awake | + Loss of consciousness | Unresponsive |
| Fractures | None | Closed or suspected | Multiple closed or open |
| Wounds | None | Minor | Major, penetrating or burns |
BP: Blood pressure; CNS: Central nervous system
| Glasgow com scale score | Systolic blood pressure, mmHg. | Respiratory rate respirations/minute | Coded value |
|---|
| 13-15 | >89 | 10-29 | 4 |
| 9-12 | 76-89 | >29 | 3 |
| 6-8 | 50-75 | 6-9 | 2 |
| 4-5 | 1-49 | 1-5 | 1 |
| 3 | 0 | 0 | 0 |
Materials and Methods
This was prospective observational study carried out between January 2013 to December 2013 at Lokmanya Tilak Municipal General Hospital, Mumbai, Maharashtra, India. The study was started after taking approval from Institutional Ethics Committee. Consent of patient’s parents was taken before inclusion in the present study. Patients younger than 12 years who sustained trauma from fall from height, road traffic accidents, sports injury, railway accidents were included in the present study. Age more than 12 years, drowning, child abuse, burns and the parents who didn’t give consent were excluded from the present study. On receiving the patient in emergency room, patients were evaluated as per standard advanced trauma life support protocols [9]. Airway, breathing and circulation were secured first and resuscitation was done. After which detailed history and radiological investigations were done. X-ray of Chest, pelvis and both hip bones were done in all patients, additional X-rays were done in patients suspected with other fractures. Focused Assessment with Sonography for Trauma (FAST) was done. Computed Tomography (CT) brain was done in the patients with symptoms or signs of brain injury which were loss of consciousness, vomiting, seizure, headache, focal neurologic signs suggestive of brain injury, depressed mental status. Data regarding demographics, vital parameters, Glasgow coma scale, laboratory parameters, number of days required for full recovery were recorded on case record proforma. Revised abbreviated injury score was used to calculate ISS [5,10,11]. Rapid respiratory rate of infant and toddler age group were adjusted before calculation of RTS [12]. The RTS, PTS calculated based on parameters at admission. ISS were calculated after primary examination, radiological investigations and intraoperative findings.
Statistical Analysis
The data analysis was done using SPSS software version 17.0 for windows. Mean score of each trauma scoring system and length of hospital stay compared by using ANOVA test. A p-value <0.05 was considered to be statistically significant.
Results
Out of 105 patients enrolled for study, four patients were discharged against medical advice and one didn’t consent. Total 100 patients were included in the study.
Out of 100 patients 95 patients had trauma due to fall from height, remaining patients suffered trauma from road traffic accidents. There were 76 male patients and 24 female patients, Male to Female ratio was 3.16:1. In present study mortality was zero. Intensive care management was required for 18 patients. The mean length of hospital stay was 7.10 days (ranged from 0-29 days). Surgery was done in nine patients.
Lowest and highest ISS was 3 and 16. PTS and RTS ranged between 6-12 and 5.43-7.84 respectively.
Mean ISS, RTS and PTS for 0-2 days of hospital admission was {(6.19±2.84), (7.59±0.41), (10.60±1.38)}, for 3-4 days it was {(6.72±3.40), (7.58±0.54), (11.03±1.42)} and for ≥5 days it was {(11.19±4.68), (7.69±0.54), (10.67±1.53)} respectively [Table/Fig-3]. For RTS and PTS p-value was not significant.
Association between hospital stay and ISS, RTS and PTS.
| Duration (days) | (X±SD) (n=100) |
|---|
| ISS | RTS | PTS | | | | | |
|---|
| 0-2 (n=43) | 6.19±2.84 | 7.59±0.41 | 10.60±1.38 |
| 3-4 (n=36) | 6.72±3.40 | 7.58±0.54 | 11.03±1.42 |
| ≤5 (n=21) | 11.19±4.68 | 7.69±0.54 | 10.67±1.53 |
| p-value | *0.04 | 0.0548 (NS) | 0.0604 (NS) |
Correlation between ISS, PTS, RTS and length of hospital stay was 0.151, -0.188 and -0.193 respectively.
[Table/Fig-4] shows that as duration of hospital stay increases mean ISS score increases, there was significant change. As duration of hospital stay increases mean PTS and RTS score did not show any significant change.
Association between length of hospital stay and mean score of ISS, RTS, PTS.
ISS: Injury severity score; RTS: Revised trauma score; PTS: Paediatric trauma score
Discussion
Weight, airway, systolic blood pressure, central nervous system parameters, associated fractures and wounds are evaluated for calculation of PTS [Table/Fig-1].
Child with small weight has less physiological reserve than that of large weight. The severity of trauma causing open wounds and skeletal fracture are usually directly proportional to the transfer of energy [13]. The PTS was found reliable predictor of outcome and severity. It was found that PTS <8 was associated with significant mortality [3,12].
In present study, as the value of mean score increases the duration of hospital stay significantly increases with ISS. This is not true in case of the RTS where there is no association found between the mean score and hospital stay duration. As the mean value of PTS increases the hospital stay duration also increases but this was not statistically significant (p>0.05).
There are very few studies where comparative analysis of length of hospital stay and trauma scores has been done. The PTS and RTS being more of physiological scoring systems are usually considered inferior to the anatomical scoring systems like ISS for prediction of the mortality and morbidity. As the mortality of present study was nil, we could not deduce any conclusion regarding mortality. According to Mayer T et al., who studied 110 paediatric patients with multiple trauma in overall mortality of that study was 14.5% and 60% patients with mean ISS score of >25, injury proved fatal. Worst outcomes were associated with mean score of >40, where there is 100% fatality [14]. In present study, maximum ISS score was 16, so it is obvious that the mortality associated should be zero. We can conclude that ISS is a simple and accurate predictor of length of hospital stay.
Study carried out by Tepas JJ et al., assessed the ability of the paediatric trauma score to predict the injury severity and mortality by analysis of its relationship with the ISS. In this study mean ISS for survivors was 8.1 in comparison to 59.7 for fatal trauma. In that study PTS greater than 8 had 0% mortality and there was increase in mortality with decrease in PTS from 8 to 0 [3]. In present study mean average PTS was 10. Only three patients had PTS less than and close to eight (one with six and other two had seven) so for obvious reasons the mortality was zero. Also, the average ISS in present study was 7.6. This way results related to survival are comparable. In present study, there was linear relationship documented between PTS and hospital stay but was not statistically significant. Recently Narci A et al., Showed that ISS is better predictor of the length of hospital stay [15].
The RTS was developed for better assessment of the head injury patients because score more inclines toward the GCS. It is helpful for overall prediction of the survival but is not very useful for the prediction of the length of hospital stay [4,15,16]. In present study there was no significant relationship with the hospital stay and RTS.
Limitation
This study was done in only one institute. Sample size was small. Study involving multiple centres and large number of patients should be done to predict the average duration of hospital stay for a particular type of trauma using scores like ISS.
Conclusion
Though, physiological parameters are important for the initial screening of the trauma patients, but the length of hospital stay does not depend on these parameters. There is no significant relationship between the length of hospital stay and RTS, PTS calculated on admission. There is positive correlation between ISS and length of hospital stay. Being a combination of anatomical and physiological parameters, ISS is a better predictor of length of hospital stay than PTS and RTS.
BP: Blood pressure; CNS: Central nervous system
[1]. Organisation WH, Inuries and violence: the factsGeneva 2010 [cited 2017 May 15]. [Available from: http://www.who.int/violence_injury_prevention/key_facts/en/ [Google Scholar]
[2]. Senkowski CK, McKenney MG, Trauma scoring systems: a reviewJ Am Coll Surg 1999 189(5):491-503.10.1016/S1072-7515(99)00190-8 [Google Scholar] [CrossRef]
[3]. Tepas JJ, Mollitt DL, Talbert JL, Bryant M, The pediatric trauma score as a predictor of injury severity in the injured childJ Pediatr Surg 1987 22(1):14-18.10.1016/S0022-3468(87)80006-4 [Google Scholar] [CrossRef]
[4]. Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME, A revision of the trauma scoreJ Trauma 1989 29(5):623-29.10.1097/00005373-198905000-000172657085 [Google Scholar] [CrossRef] [PubMed]
[5]. Baker SP, o’Neill B, Haddon W, Long WB, The injury severity score: a method for describing patients with multiple injuries and evaluating emergency careJ Trauma 1974 14(3):187-96.10.1097/00005373-197403000-000014814394 [Google Scholar] [CrossRef] [PubMed]
[6]. Moore EE, Shackford SR, Pachter HL, McAninch JW, Browner BD, Champion HR, Organ injury scaling: spleen, liver, and kidneyJ Trauma 1989 29(12):1664-66.10.1097/00005373-198912000-000132593197 [Google Scholar] [CrossRef] [PubMed]
[7]. Champion H, Frey C, Report on the major trauma outcome studyAmerican College of Surgeons Committee on Trauma Chicago 1986 PMID:2231804 [Google Scholar]
[8]. MacKenzie EJ, Shapiro S, Eastham JN, Rating AIS severity using emergency department sheets vs. inpatient chartsJ Trauma 1985 25(10):984-88.10.1097/00005373-198510000-000103930759 [Google Scholar] [CrossRef] [PubMed]
[9]. ACS Cot. Advanced trauma life support 2012 17th EditionChicagoAmerican college of surgeons:246-72. [Google Scholar]
[10]. Gennarelli TA, Wodzin E, Abbreviated injury scale 2005: update 2008Russ Reeder 2008 [Google Scholar]
[11]. Civil ID, Schwab CW, The Abbreviated Injury Scale, 1985 revision: a condensed chart for clinical useJ Trauma 1988 28(1):87-90.10.1097/00005373-198801000-000123339667 [Google Scholar] [CrossRef] [PubMed]
[12]. Eichelberger MR, Gotschall CS, Sacco WJ, Bowman LM, Mangubat EA, Lowensteiny AD, A comparison of the trauma score, the revised trauma score, and the pediatric trauma scoreAnn Emerg Med 1989 18(10):1053-58.10.1016/S0196-0644(89)80930-8 [Google Scholar] [CrossRef]
[13]. Haller JA, Pediatric trauma: the no. 1 killer of childrenJAMA 1983 249(1):4710.1001/jama.1983.033302500270226848781 [Google Scholar] [CrossRef] [PubMed]
[14]. Mayer T, Matlak ME, Johnson DG, Walker ML, The modified injury severity scale in pediatric multiple trauma patientsJ Pediatr Surg 1980 15(6):719-2.10.1016/S0022-3468(80)80271-5 [Google Scholar] [CrossRef]
[15]. Narcı A, Solak O, Turhan-Haktanır N, Ayçiçek A, Demir Y, Ela Y, The prognostic importance of trauma scoring systems in pediatric patientPediatr Surg Int 2009 25(1):25-30.10.1007/s00383-008-2287-519009298 [Google Scholar] [CrossRef] [PubMed]
[16]. Chawda M, Hildebrand F, Pape HC, Giannoudis PV, Predicting outcome after multiple trauma: which scoring system?Injury 2004 35(4):347-58.10.1016/S0020-1383(03)00140-2 [Google Scholar] [CrossRef]