Athletes who encounter repeated Functional Ankle Instability (FAI), exhibit excessive foot inversion during the various phases of gait than non-injured ankle. In gait, heel strike to toe off inversion ankle movement of the foot is controlled by eccentric function of the peroneus muscle, which stabilizes the ankle joint. As such, the purpose of this study was to investigate the response of biomechanical characteristics during gait cycle by applying neurodynamic exercise technique. An athlete with repeated FAI was checked for dynamic balance (Y-balance) and knee range of motion (using a electro-goniometer). To test the peroneal longus muscle activity and gait parameters, synchronisation of Surface Electromyography (sEMG) (Noraxon Myo-Muscle) was done with an instrumented myo-pressure treadmill in both injured and non-injured leg. Six-week post intervention measurements exhibited significant improvement in dynamic balance, knee range of motion, pain score, efficient peroneal muscle response and gait parameters. This ascertains the effect of neurodynamic technique.
Dynamic balance, Electro-goniometer, Functional ankle instability, Peroneus longus muscle, Surface electromyography
Case Report
A 17-year-old male, a medium pace cricket bowler reported with numerous ankle sprains on his right side during his training sessions, especially in trailing foot during contact phase prior to the delivery of a ball. For the past five months before the intervention, the patient experienced right ankle medial roll three times. He was referred by a sports medicine specialist for physiotherapy management at National Sports Institute, Malaysia. He walked independently with ankle brace support and was worried for his performance. The informed consent was taken from the patient and his subjective findings revealed that he was experiencing right lateral ankle pain during ankle inversion movements and especially while repeating bowling actions and the numeric pain rating score was 4/10.
Dynamic balance: Dynamic balance was measured using Y Balance Test Kit™ [1], which consists of a stance platform to which three pieces of a bamboo wooden bar scale is attached in the anterior, posteromedial, and posterolateral each directions. The posterior bars are positioned at 45° and 135° from the anterior wooden bar. Each wooden bar is marked at 5 millimetre increments to record the dynamic balance measurement score. The participant was instructed to stand on the centre wooden block on single leg and to push the indicator over the wooden scale bar anteriorly, postero-laterally and postero-medially along the stick, with the foot reaching the bar by bending the hip, knee and ankle joint of the tested leg. The participant was also instructed to return to the starting position without pushing off with the foot reaching the bar and without losing his balance. A standardised test protocol was created with sufficient rest in between the trials and it was ensured that the test was disregarded if the subject lost his balance and touched his reaching foot to the ground [2] as shown in [Table/Fig-1].
Therapist assessing the participant’s dynamic balance by using Y –balance test kit.

Range of motion: The participant was positioned on a high seated bench and instructed to place his hands behind to adopt a slumped spinal posture, facilitating the thoracic and lumbar spine to maintain a flexed posture. The hip joints were at 90° flexion, as measured by a universal goniometer and the active knee extension range of motion was measured with a neutral ankle joint by using the twin axis electro-goniometer as shown in [Table/Fig-2]. The accuracy of placement of the electrogoniometer was obtained by identifying the zero position in long sitting posture prior to the start of test.
In slump position participant’s, active Knee Range of Motion (ROM) measured by using twin axis electro-goniometer.

Gait analysis: Dynamic gait phase and spatial parameters were measured using Noraxon FDM-T SciFit myo-pressure Treadmill. The Noraxon FDM-T is fitted with 5376 Capacitive Sensors, with density of 1.4 sensors/cm2 embedded underneath the belt. The treadmill’s contact surface measures 62 feet × 22 feet. The treadmill sensors were set at a sampling rate of 100 Hz to record the force exerted by the participant while walking on the treadmill as shown in [Table/Fig-3].
Participant on myo-pressure treadmill for recording spatial gait parameters.
Surface Electromyography (sEMG) analysis: The participant’s peroneal muscle activation response was recorded with a Noraxon myo-muscle wireless sixteen-channel sEMG system. sEMG response was obtained from the peroneus longus bilaterally using eight-shaped, disposable, self-adhesive pre-gelled Ag/AgCl electrodes with dimensions 4 cm x 2.2 cm; diameter of the two circular adhesive areas was 1 cm with the inter-electrode distance being 2 cm and centered over the peroneus longus muscle bellies by following the guideline from Surface EMG For Non-invasive Assessment of Muscles (SENIAM) [3]. The skin was prepared by shaving off hair, by rasping the area gently with sandpaper and by cleaning with alcohol swab before electrode was placed. The EMG signals were acquired at a sampling rate of 500 Hz. The Root-Mean Square (RMS) amplitude for peroneus longus muscle burst was calculated as follows: the raw EMG signals were full-wave rectified, band-pass filtered with a hamming window to remove movement artefacts with a cut-off frequency of 40 Hz to 500 Hz, and smoothed with a 50 millisecond RMS algorithm. The myo-synch was used to synchronise the myo-pressure instrumented treadmill and myo-muscle sEMG. Testing was recorded to identify the injured and non-injured leg gait parameters by maintaining at 2 km/hour speed and the muscle activation of peroneus longus was recorded during stance phase of gait as shown in [Table/Fig-4].
Participant with wireless sEMG for testing peroneus longus muscle activation in stance phase of gait.

Neurodynamic Technique (NDT): The subjects underwent a six-week NDT, which consists of mobilization of the peroneal nerve,which commenced on the day after the first examination and continued for three sessions in the week. At each session, the NDT were applied on his involved leg four times for a 30 seconds period with a 1 minute pause between each application. The NDT movements carried in supine position were as follows in [Table/Fig-5].
Six weeks-Neurodynamic Technique (NDT).
| Week 1 | Passive one-end proximal sliding exercise to the peroneal nerve-knee flexion & extension movement performed by maintaining plantar-flexion of the ankle. |
|---|
| Week 2 | Passive one-end distal sliding exercise to the peroneal nerve-ankle dorsiflexion to plantar flexion movement performed by maintaining hip & knee in flexed position. |
|---|
| Week 3 | Passive two–end proximal tension exercise to the peroneal nerve-knee extension and neck flexion movement performed by maintaining the plantar-flexion of the ankle. |
|---|
| Week 4,5 & 6 | In sitting position, active two end peroneal nerves sliding exercise to the peroneal nerve- instructed to do plantar flexion and inversion of ankle with simultaneous neck extension x 2 times. The patient was also instructed to do active tension techniques by doing plantar flexion and inversion of the ankle with neck flexion movement respectively x 2 times. |
|---|
In all rehabilitation sessions, the technique was carried out without producing pain symptoms. These motions were alternated at a rate of approximately two seconds per cycle (one second into extension and one second into flexion), following the guidelines of Buttler (2005) [4]. While undergoing the six-week management process, the subject received standard physiotherapy intervention, additional with NDT as shown in [Table/Fig-6a,b]. The post intervention measurements were done at the end of sixth week. The subject maintained full compliance throughout the course of the trial, with no reported adverse effects of rehabilitation. This produced clinical improvements in patient pain, knee extension ROM, dynamic balance, peroneal muscle activation and gait parameters.
a) NDT-Knee extension (Starting Position) movement by maintaining plantar-flexion of ankle (first week); b) NDT-Passive one- end proximal sliding exercise to the peroneal nerve- knee flexion (first week).

The subject’s pain score and knee extension ROM improved in the follow-up visits and clinically exhibited a significant effect of NDT, which was maintained throughout the session. The post intervention dynamic balance score [Table/Fig-7] improved in anterior, posteromedial and posterolateral direction as derived using the Y-balance score sheet.
| Case | Variables | Pre intervention | Post intervention |
|---|
| Pain score (VAS) | Injured | 4/10 | 0/10 |
| Active Knee ROM | Injured | 90-15° | 90-2° |
| Non-injured | 90-2° | 90-1° |
| Y-Balance | Injured | 50.87 | 84.56 |
| Non-injured | 69.12 | 86.66 |
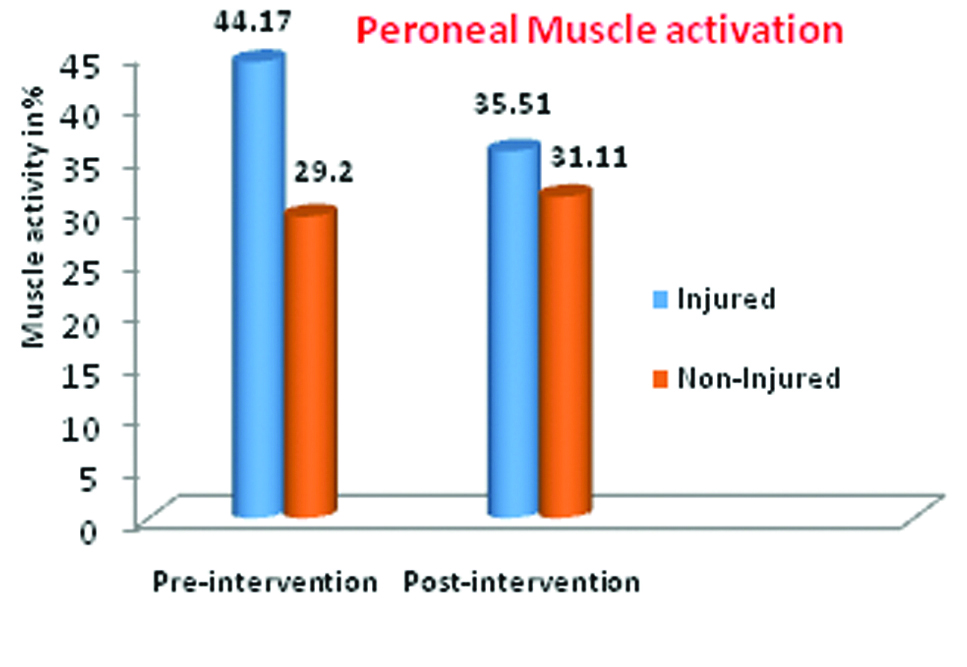
The measurements in [Table/Fig-8] show a decrease in peroneus longus muscle sEMG activation value percentage following NDT. Whereas, [Table/Fig-9] shows an increase in the spatial gait parameters and also changes in the force parameters of injured leg as compared to non-injured leg.
Peroneal muscle activation.
Spatial Gait and Force Parameters.
| Pre intervention | Post intervention |
|---|
| Stance phase (%) | Loading response (%) | Step length (cm) | Force (N) | Stance phase (%) | Loading response (%) | Step length (cm) | Force (N) |
|---|
| Injured | 69.4 | 17.6 | 34 | 548 | 75 | 20.4 | 36 | 597 |
| Non- injured | 68.1 | 19.6 | 30 | 531 | 68 | 23.6 | 36 | 570 |
Discussion
Inversion Ankle injuries (IAS) are the most common musculoskeletal injuries in sports and the rate of IAS accounts for 85% of ankle injuries with 10-30% of athletes, developing chronic ankle instability [5]. The most common injury mechanism results in a combination of inversion and adduction of the foot in plantar flexion position [6]. This injury mechanism causes a damage to the lateral ankle ligaments and produces FAI in activities involving jumping and landing movements in various sports [7]. However, the post injury imbalance between invertor and evertor muscle activation in FAI deviates the center of pressure in stance phase of gait laterally [8] and IAS disturbs the neurophysiological mechanism process in sending feedback to the central nervous system and causes repeated episodes of “giving way” or FAI [4] in basketball, volleyball and soccer players [9]. Referring to the international injury incidence, 4% of pace bowling cricketers are prone for ankle injuries [10]. More specifically, the peroneal nerve traction injury is revealed at the posterolateral knee while the foot forced into plantar flexion and inversion sprain [11].
‘The Neurodynamics techniques’ is a mechanical treatment of neural tissues in physiotherapy which has been in existence for quite some time [12,13]. This approach had been widely applied for the hamstring flexibility [14], in peroneal nerve paralysis [4], and clinical conditions demanding increase in ROM. In the past, researchers argued that the Peroneal Reaction Time (PRT) is generally prolonged in functional ankle instability [15]. The PRT was used as measurement variable to differentiate the diagnosis of chronic ankle instability [16]. However, analysing the peroneal muscle activation response during the functional tasks in gait would benefit to test the neuromuscular function, while comparing with the perturbation (unanticipated trap door) method. In ankle sprain, the mechanical and neurological properties of the joint may lead to alterations from the usual gait mechanics that place abnormal loads on the musculoskeletal system [17]. These dysfunctions could predispose repetitive injuries that lead to the development of chronic ankle instability. Therefore, understanding the mechanics of the injured and non-injured ankles loading and muscle response by applying the appropriate intervention methods, could assist clinicians in treating the dysfunction, and by avoiding further complications [18].
Athletes with repeated ankle sprains are not traditionally treated with NDT. Commonly, sports injuries are treated with the standard physical therapy protocol of exercise, ultrasound, cold and/or heat [19]. The application of NDT has recently emerged as an adjunct to the assessment and treatment of pain syndromes. NDT is theoretically aimed at reducing physical “pressure” on nerves. The previous literatures shows that NDT assists with facilitation of relative motions between nerves and adjacent tissues, which decreases nerve adherence, assists with diffusion of noxious liquids, and improves neural vascularity following the intervention [4]. Khalid R et al., strongly stated that the function of the peroneal nerve should be evaluated in all patients with the history of inversion ankle sprain [20]. Anatomically, the common peroneal nerve is the course of sciatic nerve [21]. The active slump test findings in this case showed the subject has limited terminal knee extension over his injured compared with non- injured ankle, which aligns the findings from the previous study about investigating neural tissue involvement in ankle sprain [22]. Particularly, the knee extension ROM was improved 13° post application of neurodynamic technique. The participant in this study experienced three repeated ankle slips. His pre-intervention dynamic balance (Y-balance test) of his injured ankle was grossly lower when compared to the normative data [23] and had an improved follow-up with post intervention. However, his injured ankle peroneus longus muscle activation response percentage were longer in stance phases of gait cycle compared with non-injured ankle. These findings were similar to the previous results by Feger MA et al., on peroneus longus activation response time percentage which had longer duration throughout the stride cycle in the chronic ankle instability group (36.0%±10.3%) than in the control group (23.3%±22.2%) [15]. Furthermore, the spatial gait and force parameter values for the subject progressed following the post intervention. The step length value also improved and were near normal to the non-injured leg following the six week post intervention. Finally, the results from this study showed improvement in dynamic balance and reduction over pain produced by neurodynamic technique [24]. However, in this case, the systemic response may have been attributable to combined standard physiotherapy management and NDT. This case report has limitations that it cannot be generalized when interpreting the results of the present study and is suggested for further randomised controlled trial to see the effect of neurodynamic technique in repeated inversion ankle sprains.
Conclusion
The six week neurodynamic technique post intervention assessment exhibited an improvement in the participant’s pain score, biomechanical aspects; dynamic balance, knee range of motion, peroneal muscle activation response, and increase in the percentage of gait parameters in repeated functional ankle instability for medium pace cricket bowler. From the future perspective, including NDT with standard physiotherapy management would speed up the progress of rehabilitation and reduce the recurrence rate of ankle injury. Further research is needed to address this problem with a larger sample and using motion capture system with force plate to predict the joint load and muscle force before and after the neurodynamic technique.
[1]. Shaffer LTCSW, Teyhen LTCDS, Lorenson CPTCL, Koreerat CPTCM, Straseske CPTCA, Y-Balance Test : A Reliability Study Involving Multiple Raters 2015 17810.7205/MILMED-D-13-0022224183777 [Google Scholar] [CrossRef] [PubMed]
[2]. Plisky J., Paul P. Gorman, Robert J. Butler, Kyle B. Kiesel, Frank B. Underwood, Bryant Elkins N, The Reliability of an Instrumented Device for Measuring Components of the Star Excursion Balance TestAm J Sports Phys Ther 2009 4(2):92-99. [Google Scholar]
[3]. Hermens HJ, Freriks B, Disselhorst-Klugb C, Rau G, Development of recommendations for SEMG sensors and sensor placement proceduresJ Electromyogr Kinesiol 2000 10(5):361-74.10.1016/S1050-6411(00)00027-4 [Google Scholar] [CrossRef]
[4]. Villafane JH, Pillastrini P, Borboni A, Manual therapy and neurodynamic [4]mobilization in a patient with peroneal nerve paralysis: A case reportJ Chiropr Med 2013 12(3):176-81.10.1016/j.jcm.2013.10.00724396318 [Google Scholar] [CrossRef] [PubMed]
[5]. Kerkhoffs GM, van den Bekerom M, van Beek LAM, Hullegie PA, Bloemers WAM, Diagnosis, treatment and prevention of ankle sprains: an evidence-based clinical guidelineBr J Sports Med 2012 46(12):854-60.10.1136/bjsports-2011-09049022522586 [Google Scholar] [CrossRef] [PubMed]
[6]. Hertel J, Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instabilityJournal of Athletic Training 2002 37:364-75. [Google Scholar]
[7]. Coughlan G, Caulfield B, A 4-Week Neuromuscular Training Program and Gait [7]Patterns at the Ankle JointJ Athl Train (National Athl Trainers’ Assoc 2007 42(1):51-59. [Google Scholar]
[8]. Ty Hopkins J, Coglianese M, Glasgow P, Reese S, Seeley MK, Alterations in evertor/invertor muscle activation and center of pressure trajectory in participants with functional ankle instabilityJ Electromyogr Kinesiol 2012 22(2):280-85.10.1016/j.jelekin.2011.11.01222178005 [Google Scholar] [CrossRef] [PubMed]
[9]. McKeon PO, Mattacola CG, Interventions for the Prevention of First Time and Recurrent Ankle Sprains.Clinics in Sports Medicine 2008 27:371-82.10.1016/j.csm.2008.02.00418503873 [Google Scholar] [CrossRef] [PubMed]
[10]. Orchard JW, James T, Alcott E, Carter S, Farhart P, Injuries in Australian cricket at [10]first class level 1995/1996 to 2000/2001Br J Sports Med 2002 36:270-74.[Available From: http://dx.doi.org/10.1136/bjsm.36.4.270]10.1136/bjsm.36.4.27012145117 [Google Scholar] [CrossRef] [PubMed]
[11]. Marciniak C, Fibular (Peroneal) Neuropathy. Electrodiagnostic Features and [11]Clinical CorrelatesPhysical Medicine and Rehabilitation Clinics of North America 2013 24:121-37.[Available From: https://doi.org/10.1016/j.pmr.2012.08.016 ].10.1016/j.pmr.2012.08.01623177035 [Google Scholar] [CrossRef] [PubMed]
[12]. Shacklock M, Clinical Neurodynamics a new system of musculoskeletal treatment: General Neurodynamics 2005 EdinburghElsevier Butte Rworth Heinemann:16-18.10.1016/B978-0-7506-5456-2.50006-8 [Google Scholar] [CrossRef]
[13]. Nee RJ, Butler D, Management of peripheral neuropathic pain: Integrating neurobiology, neurodynamics, and clinical evidencePhys Ther Sport 2006 7(1):36-49.10.1016/j.ptsp.2005.10.002 [Google Scholar] [CrossRef]
[14]. Pagare VK, Ganacharya PM, Sareen A, Palekar TJ, Effect of Neurodynamic Sliding Technique Versus Static Stretching on Hamstring Flexibility in Football Players With Short Hamstring SyndromeJ Musculoskelet Res 2014 17(2):1-8.10.1142/S0218957714500092 [Google Scholar] [CrossRef]
[15]. Feger MA, Donovan L, Hart JM, Hertel J, Lower extremity muscle activation in patients with or without chronic ankle instability during walkingJ Athl Train 2015 50(4):350-57.10.4085/1062-6050-50.2.0625562453 [Google Scholar] [CrossRef] [PubMed]
[16]. Lofvenberg R, Karrholm J, Sundelin G, Ahlgren O, Prolonged reaction time in patients with chronic lateral instability of the ankleAm J Sport Med 1995 23(4):414-47.10.1177/0363546595023004077573649 [Google Scholar] [CrossRef] [PubMed]
[17]. Vaes P, Duquet W, Van Gheluwe B, Peroneal reaction times and eversion motor response in healthy and unstable anklesJ Athl Train 2002 37(4):475-80. [Google Scholar]
[18]. Webster KA, Gribble PA, Functional Rehabilitation Interventions for Chronic Ankle Instability: A Systematic ReviewJ Sport Rehabil 2010 19(1):98-114.10.1123/jsr.19.1.9820231748 [Google Scholar] [CrossRef] [PubMed]
[19]. Mattacola CG, Dwyer MK, Rehabilitation of the ankle after acute sprain or chronic instabilityJournal of Athletic Training 2002 37:413-29. [Google Scholar]
[20]. Khalid R, Millar T, Khalid R, Peroneal TM, Internet T, Peroneal nerve palsy following an ankle sprain : case reportTetracyclineTeratology 2008 15(1):2650764110.5580/2357 [Google Scholar] [CrossRef]
[21]. Mitsiokapa E, Mavrogenis AF, Drakopoulos D, Mauffrey C, Scarlat M, Peroneal nerve palsy after ankle sprain: an updateEur J Orthop Surg Traumatol 2016 27(1):53-60.10.1007/s00590-016-1845-027581424 [Google Scholar] [CrossRef] [PubMed]
[22]. Pahor S, Toppenberg R, An investigation of neural tissue involvement in ankle inversion sprainsMan Ther. 1996 1(4):192-97.10.1054/math.1996.026811440507 [Google Scholar] [CrossRef] [PubMed]
[23]. Gribble PA, Hertel J, Considerations for Normalizing Measures of the Star Excursion Balance TestMeas Phys Educ Exerc Sci 2003 7(2):89-100.10.1207/S15327841MPEE0702_3 [Google Scholar] [CrossRef]
[24]. Park J, Cha J, Kim H, Asakawa Y, Immediate effects of a neurodynamic sciatic nerve sliding technique on hamstring flexibility and postural balance in healthy adults 2014 :38-42.10.14474/ptrs.2014.3.1.38 [Google Scholar] [CrossRef]