Nasopharyngeal Carcinoma: A Deceptive Presentation as Deep Neck Space Abscess
Raghul Sekar1, Vignesh Karunakaran2, Arun Alexander3
1 Junior Resident, Department of Otorhinolaryngology, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India.
2 Senior Resident, Department of Otorhinolaryngology, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India.
3 Additional Professor and Head, Department of Otorhinolaryngology, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vignesh Karunakaran, Senior Resident, Department of Otorhinolaryngology, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondichery-605006, India.
E-mail: raghul8020@gmail.com
The presentation of Nasopharyngeal Carcinoma (NPC) can be clandestine and deceptive. The NPC presenting as a deep neck space infection with airway compromise and intracranial extension is a rare occurrence. We report a case of 60-year-old male presenting with headache followed by right sided neck swelling with breathing difficulty with a Computed Tomography (CT) scan revealing a collection in deep neck space and destructive mass in the nasopharynx. We discuss the varied presentation of NPC from a trivial headache till life threatening stridor and furthermore review the literature emphasising on the same.
Headache, Lymphadenopathy, Retropharyngeal abscess
Case Report
A 60-year-old male presented to emergency department with the history of mild persistent headache for six months, painful swelling over right side neck for one week, difficulty in mouth opening for four days and history of fever and breathing difficulty on lying down for the last three days. There was no history of voice change, tooth ache or history of undergoing dental procedure in the recent past. No history of any nasal or ear complaints, no history of any comorbiditiesor addictions.
On examination, Patient was conscious, oriented, well built and nourished, pulse rate of 110/minute, respiratory rate 30/minute with mild inspiratory stridor. On oral cavity examination, there was mild trismus with poor hygiene; though no caries tooth was noted, oropharyngeal examination revealed a bulge in right lateral and posterior pharyngeal wall. On inspection of neck, there was a diffuse swelling of size 6 cm × 4 cm over right side neck extending medially from midline, laterally till anterior border of right sternocleidomastoid, superiorly from mandible till the level of hyoid bone, surface of the swelling was smooth and overlying skin was normal. Swelling was warm and tender on palpation with fluctuation. No other swelling was palpable on right side. There was diffuse 2 cm × 2 cm swelling over left side neck along the upper one third of sternocleidomastoid, on palpation it was found to be a single discrete lymph node at left level two which was firm in consistency, mobile in all directions and non tender. Surface of the swelling was smooth and overlying skin was normal. Video laryngoscopy showed the oropharyngeal swelling extending upto the level of right Pyriform sinus compressing supraglottis airway. With this history and examination we had a provisional diagnosis of right deep neck space abscess secondary to an unkown aetiology and proceeded with imaging to confirm the findings.
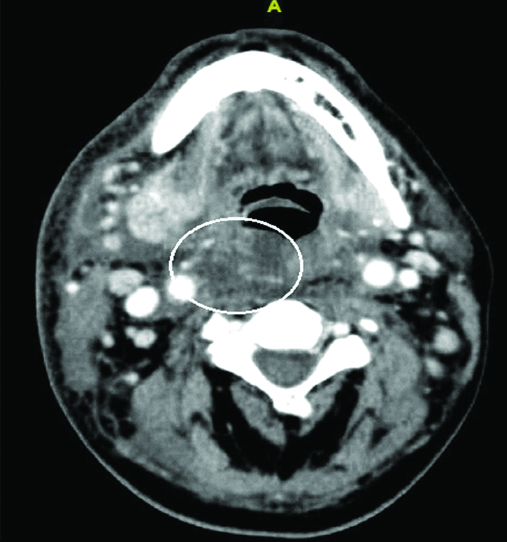
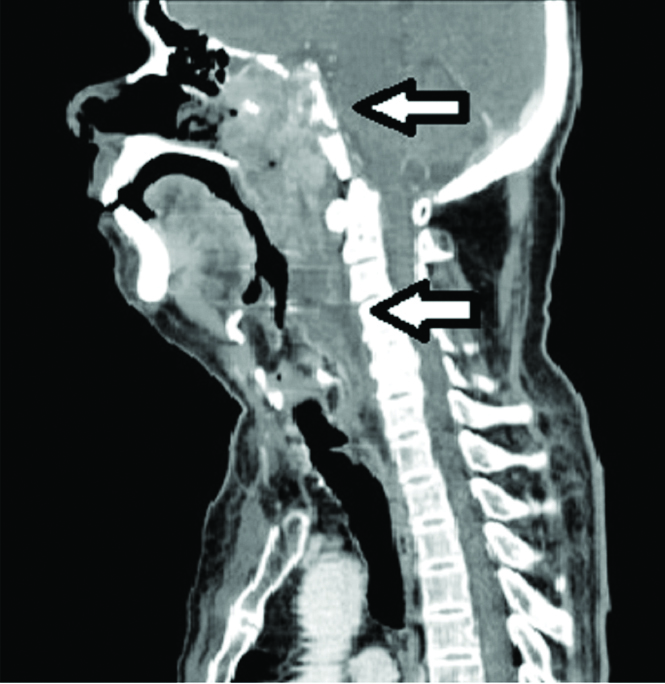
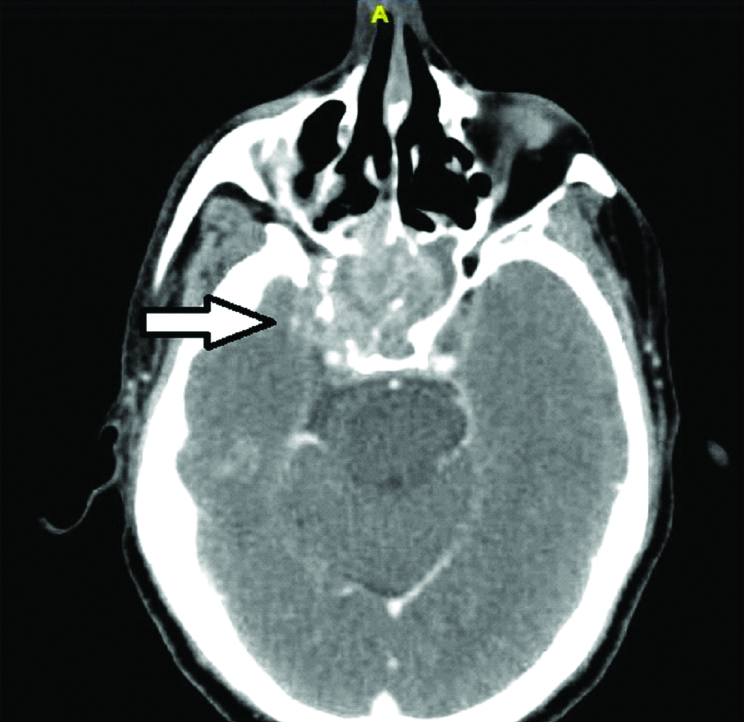
Patient underwent a contrast enhanced CT of neck which showed collection in the right pre-styloid parapharyngeal space and retropharyngeal space C2 to C4 with mild narrowing of airway and an heterogeneously enhancing soft tissue density in the nasopharynx extending into sphenoid sinus with destruction of its bony walls and extension into middle cranial fossa [Table/Fig-1,2 and 3]. Retrospectively, the patient’s neurological examination was normal and he had right ear serous otitis media, though he didn’t have any ear complaint.
Low density soft tissue swelling in the right retropharyngeal and parapharyngeal space (circle) corresponding to the bulge in the pharyngeal wall.
Sagittal section showing both the lesion in nasopharynx with bony destruction of sphenoid sinus and collection in retropharyngeal space (white arrows).
Heterogenously enhancing sift tissue density in nasophaynx with destruction of bony walls of sphenoid sinus with extension into middle cranial fossa (white arrow).
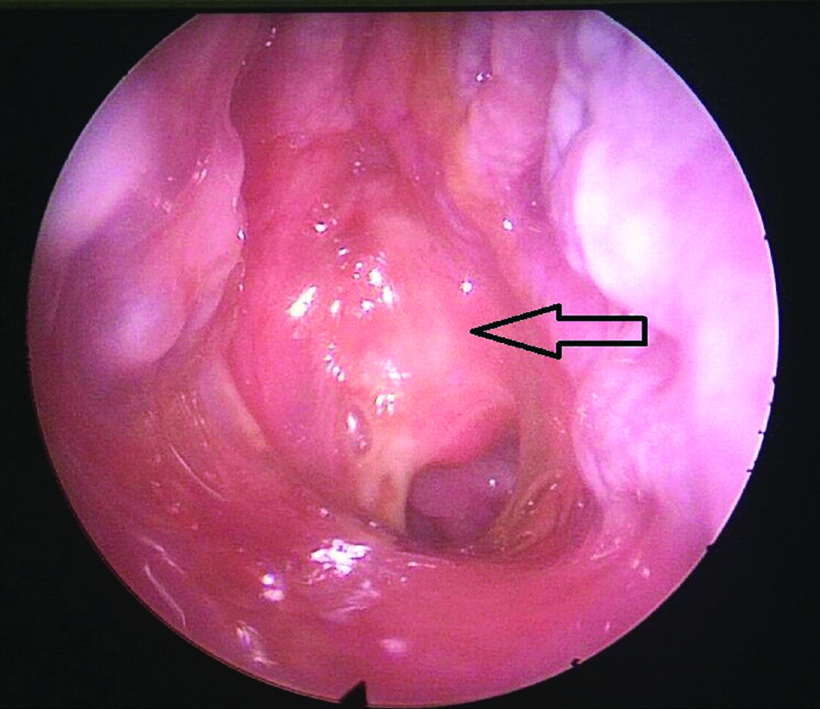
The patient underwent tracheostomy in view of difficult intubation and under general anaesthesia the abscess was drained by an external incision, about 25-30 mL of pus was drained. On diagnostic nasal endoscopy, a mucosa covered proliferative mass was seen in the nasopharynx which was biopsied for histopathological examination [Table/Fig-4]. Biopsy turned out to be undifferentiated squamous cell carcinoma showing uniform cells with ovoid vesicular nuceli, prominent nucleoli with indistinct cell borders and numerous lymphocytic infiltrations. Patient improved with intravenous Cloxacillin, Gentamycin and Metronidazolefor two weeks followed by oral Clindamycin for two weeks as culture sensitivity showed klebsiella pneumoniae sensitive to clindamycin and neck wound was allowed to heal by secondary intention. Patient received concurrent chemoradiation with 70 Gy/35 fractions for seven weeks along with weekly cisplatin for NPC after discussion with multidisciplinary team for malignancy. Patient was followed up with two-monthly nasoendoscopy and was disease free at the end of one year.
Endoscopic view of right nasal cavity showing proliferative mass (black arrow) in nasopharynx covered with discharge.
Discussion
The NPC is a tumour that exhibits a characteristic ethnic and geographical distribution, primarily affecting people from southern China, Southeast Asia with 80% cases being prevalent in these areas [1]. It is primarily a disease of the young, the incidence rates rising at 20 years, stabilising between 35-60 years and declining subsequently. In high risk population, there is a peak incidence between 45 and 54 years and declines thereafter [1]. Numerous aetiological agents have been implicated in its causation including the Ebstein-Barr virus, environmental toxins, HLA genes and a genetic predisposition [1]. Further cantonese style salted fish and other salted and preserved food items contain nitrosomamines which has been proposed to act as a carcinogen for NPC [2,3]. The probable differential diagnosis for this condition is lymphoma, haemangioma, haemaniopericytoma, rhabdomyosarcoma, chordoma etc.
The presenting symptoms and signs of NPC can be so varied that it can be a conundrum for the practicing physician. In a study done by Lee AW et al., the most common symptoms were a neck swelling seen in 3612/4768 (75.8%) of patients, nasal complaints in 3501/4768 (73.5%) of patients and aural symptoms in 2975/4768 (62.4%) of patients while headache was complained by 1657/4768 (34.8%) of patients [4]. In another study done by Suzina SA et al., an unilateral neck mass was a presenting complaint in 22/56 (39.3%) patients, nasal complaints in 39/56 (69.6%) and aural symptoms in 34/56 (60.7%) while headache was seen in 23/56 (41.1%) patient [5].
In the above studies, we can see that a patient perceived a neck mass in a majority of situations, with aural and nasal symptoms such as deafness, otalgia, epistaxis, nasal obstruction being the next most common reason for presentation. Headache though a trivial symptom is one of the most common complaint in patients with NPC which is regarded as those of benign disease by both the patient and clinician [5]. It has been recognised that early detection of the tumour is an exception rather the rule. However, the patients came reporting a neck mass and this was indicative of cervical lymphadenopathy while the involvement of retropharyngeal nodes has largely been undiscussed. Chong V et al., documented the incidence of asymptomatic retropharyngeal lymphadenopathy in 29.1% to 89% of patients diagnosed with NPC [6]. This can be explained by the proximity of the nasopharynx to the retropharyngeal space in which case, the tumour would first metastasise to the node of Rouviere and then spread to the cervical lymph nodes. Infection can be superadded onto the malignancy, leading to a retropharyngeal abscess, taken along with benign nasal or aural symptoms, misguide the clinician to think of an infective pathology. The NPC can cause erosive or permeative bone changes of skull base or spread through foraminal pathways causing intracranial extension as in present case leading to progression of disease to a higher stage [7]. This impacts the prognosis: it has been seen that symptom duration was a significant factor that affected the mortality, the incidence of treatment failure and need for radical radiotherapy [4]. The latter most leads to an increase in the toxicity of treatment such as mucosits, oral candidiasis, xerostomia, dental caries, soft tissue fibrosis and visual changes, further decreasing the quality of life.
A high index of suspicion by the treating physician is necessary for successfully detecting an early tumour, which would lead to lower rates of morbidity and mortality. When surgical drainage or needle aspiration is performed for deep neck infection, routine pathological examination of the tissue must be performed to exclude the possibility of malignancy [8]. The present patient had failed to seek medical attention for headache considering it to be a trivial symptom. There was significant delay in diagnosis and treatment, leading to morbidity in terms of deep neck space infection and intracranial extension of the tumour and the need to delay radiotherapy till the infection subsided. Further infection in the deep neck space has potential neurovascular complications along with airway compromise. Since, present patient presented with airway compromise, tracheostomy had to be done to secure the airway adding to the existing morbidity. Though aural complaints are common in the presentation of NPC, the present patient did not have any complaints. Any further delay in the presentation in this patient would have caused death not only by the complication of deep neck space infection but also by direct intracranial extension of the tumour as seen on CT. Retropharyngeal abscess can be explained by probable infection of the retropharyngeal lymph nodes which drain nasopharynx. Present report thus brings to light one of the rare presentations of NPC as a retropharyngeal abscess which has spread to parapharyngeal space leading to airway compromise and the importance of headache in the symptomatology of NPC.
Conclusion
The NPC is a silent malignancy with myriads of presentation and early diagnosis becomes imperative as the stage and extent of the disease at the time of diagnosis and initiation of treatment is an important prognostic factor. The present article highlights rare presentation of NPC as deep neck space infection and the need for a full otorhinolaryngological examination to identify head and neck cancer in case of cervical lymphadenopathy with a deep neck abscess.
[1]. Tsao SW, Yip YL, Tsang CM, ang PS, Lau VM, Zhang G, Etiological factors of nasopharyngeal carcinomaOral Oncol 2014 50(5):330-38.10.1016/j.oraloncology.2014.02.00624630258 [Google Scholar] [CrossRef] [PubMed]
[2]. Jia WH, Luo XY, Feng BJ, Ruan HL, Bei JX, Liu WS, Traditional Cantonese diet and nasopharyngeal carcinoma risk: a large-scale case-control study in Guangdong, ChinaBMC Cancer 2010 10:44610.1186/1471-2407-10-44620727127 [Google Scholar] [CrossRef] [PubMed]
[3]. Zou XN, Lu SH, Liu B, Volatile N-nitrosamines and their precursors in Chinese salted fish--a possible etological factor for NPC in chinaInt J Cancer 1994 59(2):155-58.10.1002/ijc.29105902027927911 [Google Scholar] [CrossRef] [PubMed]
[4]. Lee AW, Foo W, Law YF, Poon WM, Sze OSK, Nasopharyngeal carcinoma: presenting symptoms and duration before diagnosisHong Kong Med J 1997 3(4):355-61. [Google Scholar]
[5]. Suzina SA, Hamzah M, Clinical presentation of patients with nasopharyngeal carcinomaMed J Malaysia 2003 58(4):539-45. [Google Scholar]
[6]. Chong V, Fan Y, Khoo J, Retropharyngeal lymphadenopathy in nasopharyngeal carcinomaEur J Radiol. 1995 21(2):100-05.10.1016/0720-048X(95)00689-N [Google Scholar] [CrossRef]
[7]. Chidhara PS, Venkateshwaran A, Imaging of nasopharyngeal carcinoma with intracranial extensionInt J Sci Stud 2014 2(91):117-20. [Google Scholar]
[8]. Wang CP, Ko JY, Lou PJ, Deep neck infection as the main initial presentation of primary head and neck cancerJ Laryngol Otol 2006 120(4):305-09.10.1017/S002221510600028416623974 [Google Scholar] [CrossRef] [PubMed]