Basal Cell Adenoma Arising in the Minor Salivary Gland of the Hard Palate
Tatsuo Okui1, Soichiro Ibaragi2, Keisuke Nakano3, Yukiko Fujii4, Akira Sasaki5
1 Assistant Professor, Department of Oral and Maxillofacial Surgery, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Science, Okayama, Japan.
2 Assistant Professor, Department of Oral and Maxillofacial Surgery, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Science, Okayama, Japan.
3 Associate Professor, Department of Oral Pathology and Medicine, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Science, Okayama, Japan.
4 Fellow, Department of Oral and Maxillofacial Surgery, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Science, Okayama, Japan.
5 Professor, Department of Oral and Maxillofacial Surgery, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Science, Okayama, Japan.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Tatsuo Okui, 2-5-1 Shikatach O Kitaku, Okayama-700-8525, Japan.
E-mail: tatsuookui0921@gmail.com
Basal Cell Adenoma (BCA) is an extremely rare benign salivary gland tumour that usually arises in the parotid gland. The incidence of BCA is 1%-3% of all salivary gland tumours. Here, we report an extremely rare case of BCA arising in the minor salivary gland of the hard palate of a young man.
Basal cell adenoma, Benign salivary tumour, Salivary gland tumour
Case Report
A 24-year-old, Malaysian man was referred to Okayama University Hospital in February 2014 for the evaluation of a painless mass in his hard palate that had increased in size over several months. There was no medical, dental or personal history related to the patient’s main complaint. General clinical examination was unremarkable with no history of systemic diseases. The extraoral examination revealed a symmetrical face and no extraoral swelling.
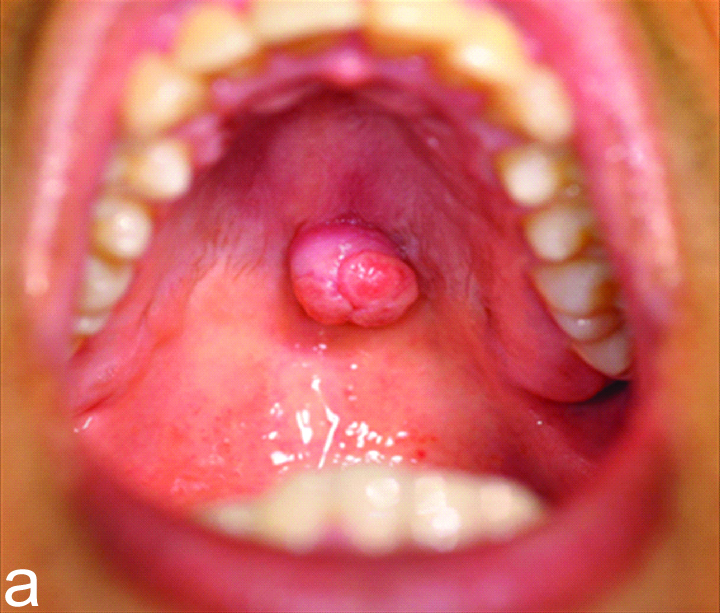
Intraoral examination showed that the mass on hard palate was round, measuring approximately 12 mm in diameter, elastic, and relatively soft. The mucosa covering the mass was normal [Table/Fig-1a].
Intraoral view at the first visit.
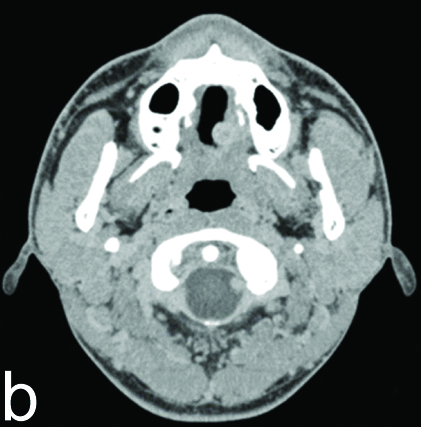
Computed Tomography (CT) imaging showed a round, well-circumscribed mass with no resorption in the hard palate bone [Table/Fig-1b]. We made the clinical diagnosis of benign palatal tumour based on the clinical features and CT images. On the basis of this clinical diagnosis, we conducted a tumour resection with a 5 mm safety margin under local anaesthesia. The periosteum of the palate bone was also removed. The histopathological diagnosis was BCA in the palate. No recurrence has been detected in the two years of follow up since the surgery.
scan CT imaging showed that the mass was round and well-circumscribed..
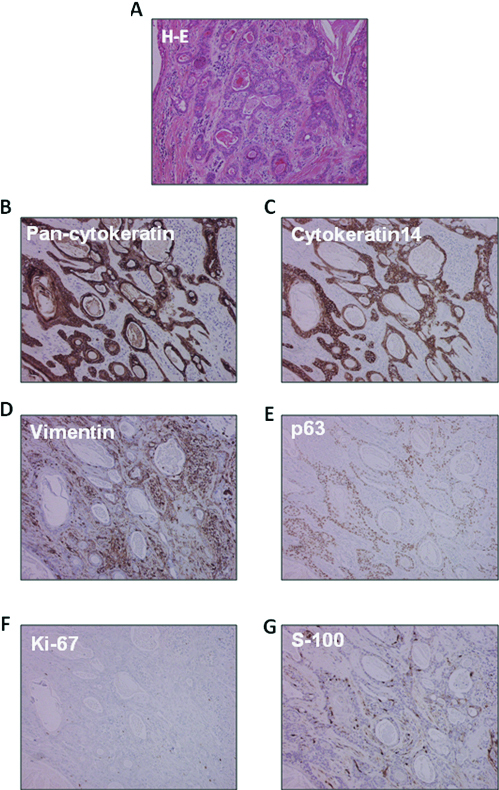
Histopathologically, the tumour was well encapsulated by fibrous connective tissue. The tumour tissue showed numerous epithelial tumour nests of varying size, with collagenous stroma. The tumour nests were composed of uniform basaloid cells with scant cytoplasm, undefined cell borders and round-to-oval nuclei arranged in tubules, with trabecular sheets. Many duct-like structures lined by cuboidal or basaloid cells were evident within the trabecular tumour nests. Occasionally, peripheral cuboidal cell palisading were observed in the tumour nests.
The mitotic rate was 1/10 high-power field (hpf). In the immunohistochemical staining, positive reactions for pancytokeratin, cytokeratin-14, p63, S-100 and vimentin were observed in the tumour nests. The pancytokeratin staining was most intense in the ductal cells. Cytokeratin-14 showed positivity across the whole tumour nests. The peripheral and palisading cells tend to show a positive reaction for myoepithelial markers. Many S-100-positive spindle cells were observed in the fibrous stromal tissue. The Ki-67 index was 3%. These histological findings were consistent with BCA, tubulo-trabecular type [Table/Fig-2].
Histopathological features of the patient’s palatal BCA 100X. a) H-E stain. Immunoreactivity for b) pancytokeratin; c) cytokeratin-14; d) vimentin; e) p63; f) Ki-67; g) S-100 protein.
Discussion
Salivary gland tumours are uncommon, accounting for <5% of all head and neck tumours [1]. BCA accounts for <1% of all salivary gland tumours [1]. Among the reported cases of BCA, 75% were located in the parotid gland and 20% were located in the minor salivary glands of the lip [2]. The BCA located in a minor salivary gland in the palate, as in the present patient, is extremely rare [2]. Only five other BCA cases arising at the hard palate have been reported [2-6]. In all of the prior cases, the treatment was surgical excision.
BCA was first described by Kleina in 1967 and BCA is included as a salivary gland tumour in the 1991 World Health Organization (WHO) classification [7]. BCAs display basaloid cells with a prominent basal cell layer and a distinct basement membrane-like structure without a myxochondroid component. BCAs can arise at any age and in either sex, they have usually been observed in the seventh decade of life and more often in females; the male to female ratio being 1:2.
The present BCA arose in a male in his twenties, which is extremely rare. For the reasons mentioned above, it was difficult to clinically diagnose his tumour as a BCA case. Pathologically, the differential diagnosis of Basal Cell Adenocarcinoma (BCAC) and Adenoid Cystic Carcinoma (ACC) versus BCA is difficult because of the similar cellular composition of these tumours. However, histologically BCACs show infiltration into adjacent structures, and ACCs lack a vascular component and show perineural invasion compared to BCAs [1].
In immunohistochemistry analyses, BCACs and BCAs have exhibited nuclear p63, S-100, and cytokeratin protein [2]. These findings are helpful for differentiating basal cell neoplasms from ACCs. The final diagnosis is difficult based on imaging and clinical findings alone. Nagao K et al., indicated that the Ki-67 labeling index is <3% in BCAs but are over 30% in BCACs, and that Ki-67 labeling should thus be performed to distinguish BCA from BCAC [2].
BCAs are categorized by their morphologic pattern into four subtypes: solid, trabecular, tubular, and membranous types. The tumour usually shows a predominance of one of these patterns. The present BCA exhibited predominantly the tubular pattern with some areas of the trabecular pattern. BCAs are usually a non-recurrent tumour, except for the membranous type, which has a recurrence rate of 25% [9]. Although, it is an extremely rare, malignant transformation of BCA has been reported. Careful follow up of BCAs is thus advisable.
Conclusion
Basal cell adenoma is rare benign tumor arising in minor salivary gland. Membranous type BCA is at high risk of developing recurrence.
[1]. Faquin WC, Powers C, Basaloid tumours: basal cell adenoma and basal cell adenocarcinoma. In: Salivary Gland Cytopathology. Print ISBN: 978-0-387- 76622-5.Vol. 5 of the series Essentials in Cytopathology Series. 2008 5U.S.Springer:115-30. [Google Scholar]
[2]. Yadav AB, Narwal A, Devi A, Kumar S, Yadav SK, Basal cell adenoma of palate, a rare occurrence with review of literatureJ Dent Shiraz Univ Med Sci 2015 16:291-95. [Google Scholar]
[3]. Esteves AR, Dib LL, Carvalho LV. Basal cell adenoma: A case reportJ Oral Maxillofac Surg 1997 55(1):1323-25.10.1016/S0278-2391(97)90193-2 [Google Scholar] [CrossRef]
[4]. Siddaraju A, Giraddi GB, Hemamythily P, Bhatt G, Nayaknur VA, Basal cell adenoma of palate- report of a rare lesionArchives of Oral Sciences & Research 2013 3(1):51-55. [Google Scholar]
[5]. Gupta N, Jadhav K, Ahmed MB, Amberkar VS, Basal cell adenoma in a relatively rare siteJ Oral Maxillofac Pathol 2009 13(2):101-04.10.4103/0973-029X.5768021887012 [Google Scholar] [CrossRef] [PubMed]
[6]. Ishibashi N, Yanagawa T, Yamagata K, Karube R, Shinozuka K, Nagata C, Basal cell adenoma arising in a minor salivary gland of the palateOral Maxillofac Surg 2012 16(1):111-14.10.1007/s10006-011-0263-z21327332 [Google Scholar] [CrossRef] [PubMed]
[7]. Veeresh M, Bavle RM, Vinay KN, Nandakumar H, Basal cell adenoma of the submandibular glandJ Maxillofac Oral Surg 2010 9(3):01-03.10.1007/s12663-010-0035-622190808 [Google Scholar] [CrossRef] [PubMed]
[8]. Nagao K, Matsuzaki O, Saiga H, Sugano I, Shigematsu H, Kaneko T, Histopathologic studies of basal cell adenoma of the parotid glandCancer 1982 50(1):736-45.10.1002/1097-0142(19820815)50:4<736::AID-CNCR2820500419>3.0.CO;2-M [Google Scholar] [CrossRef]
[9]. Kudoh M, Harada H, Sato Y, Omura K, Ishii Y, A case of basal cell adenoma of the upper lipCase Reports in Medicine 2014 2014(1):795356-20.4 pages, doi:10.1155/2014/79535610.1155/2014/79535624711821 [Google Scholar] [CrossRef] [PubMed]