Congenital Midline Cervical Cleft–Clinical and Pathological Review of Three Cases
Anjireddy Kallam1, M Anantha Satyanarayana2
1 Director and Plastic Surgeon, Department of Plastic Surgery, ASRAM Medical College, Eluru, Andhra Pradesh, India.
2 Assistant Professor, Department of Pathology, ASRAM Medical College, Eluru, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anjireddy Kallam, Director and Plastic Surgeon, Department of Plastic Surgery, ASRAM Medical College, Eluru-534005, Andhra Pradesh, India.
E-mail: reddykanji@gmail.com
We are presenting three rare cases of Congenital Midline Cervical Cleft (CMCC). All are treated by excision and Z-plasty. Embryology, clinical appearance, histopathology and treatment have been discussed with review of the available literature.
Deformities, Fissure, Neck, Z-plasty
Congenital midline cervical cleft is a rare developmental anomaly in the midline of the neck. It was first described by Luschka in 1848 as “congenital fistula of the neck” [1]. After that less than 200 cases are reported in literature [1]. Early diagnosis and surgical intervention during infancy leads to a better functional and aesthetic outcome. Inadequate treatment may cause secondary complications such as impaired neck extension [2].
Case Series
Case 1
A 4-year-old female child, was born to non consanguineous parents after full term normal delivery. Parents brought the child to plastic surgery OPD with a complaint of a scar in the midline of the neck and difficulty in full extension of the neck. There was no similar or any other congenital abnormality in the family. On examination there was a fissure in the midline of the neck of 5 cm in length extending from hyoid region to below the thyroid cartilage. Both ends of the scar ended in a blind pouch. A nipple like skin tag was present at the upper end [Table/Fig-1a]. There were no other congenital abnormalities.
Case 1-Preoperative photograph; Case 1-Postoperative photograph.
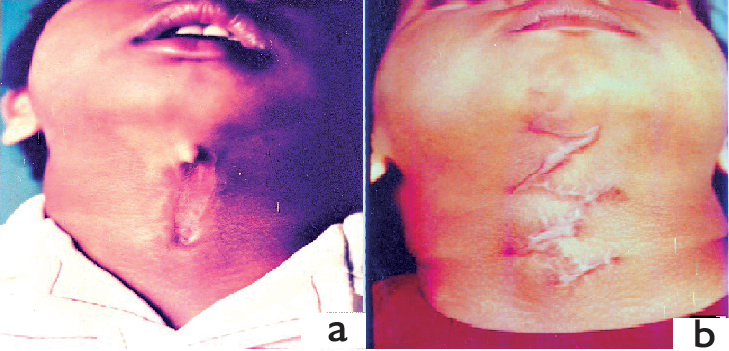
The child was operated under general anaesthesia at the age of four years. The fissure was completely excised up to the deep fascia and the wound was closed by double Z-plasty. When the child came for checkup after three months, full extension of the neck was possible, but some hypertrophy of the limbs of Z-plasty was observed [Table/Fig-1b].
Case 2
A 10-year-old male child was born to parents of non consanguineous marriage, after full term normal delivery. The child was brought to plastic surgery OPD by the parents with the complaint of restricted extension of the neck. There was no similar or any other congenital abnormality in the family. On examination, we found a 2 cm long fissure in the midline of the neck near the hyoid region with a nipple like skin tag in the upper part [Table/Fig-2a]. There was associated midline webbing of the neck. Extension of the neck was restricted [Table/Fig-2b]. There are no other congenital abnormalities such as macrostomia.
Case 2-Preoperative photograph; Case 2-Preoperative photograph (Lateral view); Case 2-Postoperative photograph; Case 2-Postoperative photograph (Lateral view).
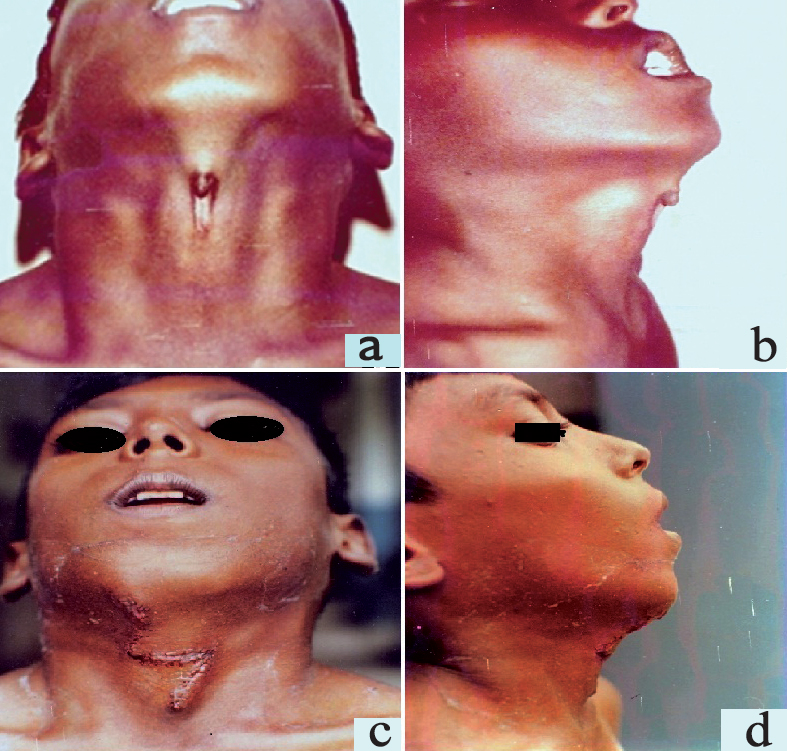
Under general anaesthesia the fissure was completely excised and the defect was repaired by Z-plasty [Table/Fig-2c]. Follow up after three months showed normal extension of the neck [Table/Fig-2d].
Case 3
A 19-year-old female, born after full term normal vaginal delivery presented to plastic surgery OPD with midline neck swelling since birth. There was no similar or any other congenital abnormality in the family. On examination, a 0.5 cm tongue like protruded swelling in midline of neck near the hyoid region with fissure below. There was a blind sinus with cord like thickening extending 3.5 cm from it [Table/Fig-3a]. No discharge was observed from the sinus. The length and depth of the sinus tract was probed with 2.0 prolene suture [Table/Fig-3b]. The distal end was blind; the sinus tract was subcutaneous and measuring about 3.5 cm in length. Under general anaesthesia the fissure was completely excised and the defect was repaired by double Z-plasty. Grossly, it was composed of three components, a superior tongue like projection, a blind sinus of 2.5 cm depth at the inferior end, and a midline longitudinal sulcus between them [Table/Fig-3c].
Case 3-Preoperative photograph; Case 3-Intraoperative photograph; Case 3-Excised specimen; Case 3-Postoperative photograph.
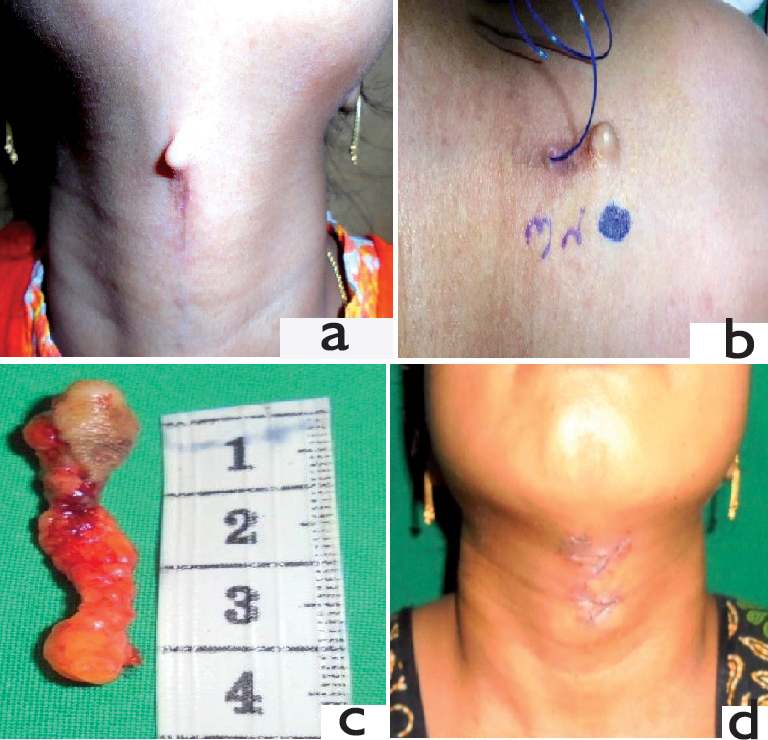
Follow up after 3 weeks showed normal extension of the neck [Table/Fig-3d].
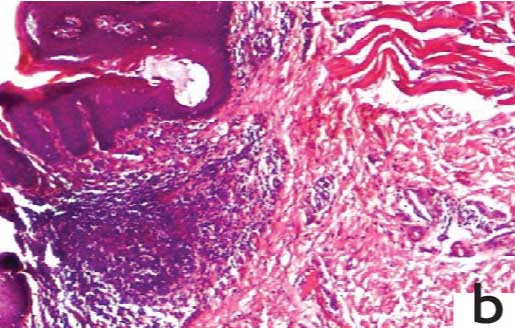
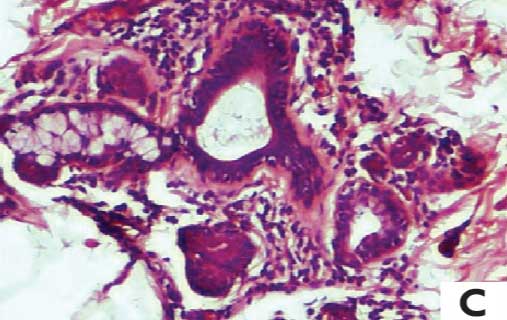
Microscopically, the superior tongue like projection shows skin, covered by stratified squamous epithelium with surface parakeratosis. Dermis shows dermal appendages, fibro fatty tissue and skeletal muscle bundles [Table/Fig-4a]. Middle cleft portion shows indentation of the skin covered by stratified squamous epithelium with surface parakeratosis. Dermis shows absence of adnexal structures and presence of haphazardly arranged skeletal muscle bundles at the edge of the indentation [Table/Fig-4b]. Lower portion of the blind duct is lined by pseudostratified ciliated columnar epithelium of upper respiratory type, which is surrounded by seromucinous glands [Table/Fig-4c]. All three cases are summarised in [Table/Fig-5].
Case 3-Photomicrograph of superior tongue like projection showing stratified squamous epithelium with parakeratosois, dermal appendages, fibro fatty tissue and skeletal muscle bundles (H&E, 40X).
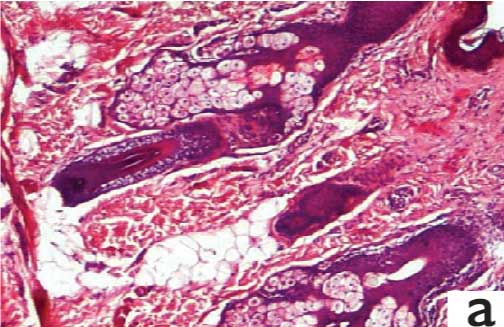
Case 3-Photomicrograph of middle cleft portion showing indentation of the stratified squamous epithelium with parakeratosois, absence of adnexal structures and presence of skeletal muscle bundles in the dermis at the edge of the indentation (H&E, 40X).
Case 3-Photomicrograph of the lower portion of the blind duct showing pseudostratified ciliated epithelium of upper respiratory type and surrounded by seromucinous glands (H&E, 100X).
| Case | Age of the presentation | Gender | Treatment |
|---|
| 1 | 4 | Female | Excision followed by double Z-plasty |
| 2 | 10 | Male | Excision followed by Z-plasty |
| 3 | 19 | Female | Excision followed by double Z-plasty |
Discussion
Congenital midline cervical cleft is a very uncommon malformation of the anterior neck which is present at birth. A female to male ratio of 2:1 is reported, with a sporadic presentation [2], which is similar to our cases. They may occur alone or there may be associated anterior webbing of the neck [2-3]. In one (Case 2) of our cases, where the cervical cleft was near the hyoid region, anterior midline cervical webbing was also present. Saha S et al., published five cases of congenital midline cervical cleft for the first time in Indian subcontinent followed by our study with three cases and single case reports [4-7].
Regarding the aetiological factors there was no hereditary or environmental factors in any of the cases reported. CMCC is due to failure of fusion of the paired branchial arches (I and II) in the process of development of the neck during eighth to twelfth week of foetal development [8]. Faulty closure of the branchial arches is either due to presence of amniotic adhesions, vascular anomalies, failure of the mesenchyme to penetrate the midline, with subsequent poor interaction between the mesoderm and ectoderm and pressure exerted on the cervical area by the pericardial roof [9].
It presents at birth as a visible defect in the midline cervical region and it is often overlooked or misdiagnosed [2]. CMCC is diagnosed by clinical examination, and the three typical findings which include nipple-like skin tag in the cranial portion, a sinus tract or fistula in the caudal portion, and a midline cleft resembling a skin defect in between [10]. Microscopy shows skin epidermis which is lined by stratified squamous epithelium with surface parakeratosis. Dermis reveals the absence of skin adnexal structures at midline cleft portion and haphazardly arranged skeletal muscle bundles mixed with fat tissue and the blind sinus tract is lined by pseudostratified ciliated epithelium of upper respiratory type which is surrounded by seromucinous glands [2].
Either hypoplasia of midline neck structures or other head and neck congenital abnormalities such as cleft lower lip, cleft tongue, and cleft mandible are known to be associated [10]. In our three cases, except midline cervical cleft no other anomaly was found.
Radiographs of the neck occasionally may show bony mandibular spur. Ultrasound of the neck shows a midline blind-ending sinus tract from the skin surface and normal thyroid gland. MRI shows T1 hypointense, T2 hyperintense linear tract with peripheral enhancement and excludes thyroglossal duct cysts or branchial cleft anomalies [11].
A sinogram may be obtained by injecting radiopaque dye into the sinus tract to know the length and depth of the sinus tract. Fine needle aspiration is helpful in distinguishing branchial cleft cysts from malignant neck masses and culture of the aspirated material may guide antibiotic therapy for infected cysts [9].
Treatment in early infancy is advocated to prevent developmental abnormality of the neck or of the mandible. The treatment is in the form of excision of the complete fissure with any sinus tracts or skin tags if present and repair of the defect by Z-plasty (single or multiple), to prevent cicatricle neck contracture and the resulting limitation of neck motion [3,12]. In one of the case, which is previously reported, the authors have observed hypertrophy of the oblique limbs of the Z-plasty [13]. We also had similar experience in case one, even though wound healed well initially by primary intention.
Conclusion
Congenital midline cervical cleft is a rare developmental abnormality of the anterior part of the neck which can be successfully treated by complete excision and Z-plasty. It is important to recognise this rare congenital anomaly early, as the operating results are excellent.
[1]. Puscasn L, Midline cervical cleft: review of an uncommon entityInternational Journal of Pediatrics 2015 2015:20941810.1155/2015/20941825983756 [Google Scholar] [CrossRef] [PubMed]
[2]. Sinopidis X, Kourea HP, Panagidis A, Alexopoulos V, Tzifas S, Dimitriou G, Congenital midline cervical cleft: diagnosis, pathologic findings, and early stage treatmentCase Reports in Pediatrics 2012 2012:95104010.1155/2012/95104023094176 [Google Scholar] [CrossRef] [PubMed]
[3]. Wynn-Williamss D, Congenital midline cervical cleft and webBr J Plast Surg 1952 5:87-93.10.1016/S0007-1226(49)80016-6 [Google Scholar] [CrossRef]
[4]. Saha S, Misra S, Saha VP, Mondal AR, Midline cervical cleft: A report of two casesIndian J Otolaryngol Head Neck Surg 2005 57:78-79. [Google Scholar]
[5]. Saha VP, Pal S, Saha S, Misra S, Congenital midline cervical cleft: a 7 year prospective studyIndian J Otolaryngol Head Neck Surg 2013 65(4):367-70.10.1007/s12070-013-0670-624427601 [Google Scholar] [CrossRef] [PubMed]
[6]. Jaiswal AA, Behara BK, Membally R, Mohanty MK, Congenital midline cervical cleft: a case report with review of literatureInt J Head Neck Surg 2017 8(1):25-30.10.5005/jp-journals-10001-1301 [Google Scholar] [CrossRef]
[7]. Doddamani SS, Handi PS, Chandrashekharyya SH, Suligavi SS, Chouguley SS, Congenital midline cervical cleft: a case report and an embryological reviewJ Clin Diagn Res 2012 6(6):1086-88. [Google Scholar]
[8]. Mirzaa B, Congenital midline cervical cleftAPSP J Case Rep 2013 4:9 [Google Scholar]
[9]. Kakodkar K, Patel S, Maddalozzo J, Congenital midline cervical cleftOtolaryngology 2013 3:13210.4172/2161-119X.1000132 [Google Scholar] [CrossRef]
[10]. Eom TK, Sun H, Yoon HK, Congenital midline cervical cleftArch Plast Surg 2014 41(4):429-31.10.5999/aps.2014.41.4.42925075373 [Google Scholar] [CrossRef] [PubMed]
[11]. Villanueva-Meyer J, Glastonbury C, Marcovici P, Congenital midline cervical cleftJournal of Radiology Case Reports 2015 9(3):07-11.10.3941/jrcr.v9i3.220225926928 [Google Scholar] [CrossRef] [PubMed]
[12]. Bajaj Y, Dunaway D, Hartley BE, Surgical approach for congenital midline cervical cleftJ Laryngol Otol 2004 118:566-69.10.1258/002221504161507415318968 [Google Scholar] [CrossRef] [PubMed]
[13]. Eastlack JP, Howard RM, Frieden IJ, Congenital midline cervical cleft: Case report and review of the English language literaturePediatric Dermatology 2000 17(2):118-22.10.1046/j.1525-1470.2000.01727.x10792800 [Google Scholar] [CrossRef] [PubMed]