Introduction
Cataract is one of the leading causes of curable blindness in the world. The only way to cure cataract related blindness is surgery, which has changed fundamentally by the introduction of phacoemulsification, and now it has become the standard method to remove cataract. Many complications can occur during standard phacoemulsification using traditional ultrasound. Corneal decompensation is a rare but potentially vision-threatening complication after phacoemulsification surgery [1].
With the advent of specular microscopy, pachymetry and flourophotometry, endothelial morphology, pump function and permeability characteristics can now be quantitated easily.
Corneal endothelial cells are non replicative, and the loss of these cells is only compensated by the migration, enlargement, and increasing heterogeneity of the cells [2]. Loss of endothelial function by the damage of endothelial cells can lead to increased corneal thickness and decreased corneal transparency because of increased stromal hydration due to compromised pump function [3].
Thus, the evaluation of preoperative, intraoperative, and postoperative risk factors for endothelial cell loss provides important information, which can lead to increased corneal decompensation after phacoemulsification surgery. Phacoemulsification surgery is performed in a limited, confined space; however, securing adequate surgical space during an operation can decrease the risk of corneal endothelial cell loss as a result of the phacoemulsification procedure. Anatomical and surgical factors, such as adequate ACD, Ultrasound Time (UST) and ultrasound power are important for preserving these cells from the mechanical and thermal damage that can occur during phacoemulsification [1].
Maintenance of corneal transparency is an important aspect of successful cataract surgery. Hence, corneal endothelial cell loss was compared according to different ACDs in patients with various preoperative and intraoperative parameters.
Materials and Methods
This study was a hospital based comparative type of observational study and was conducted on the patients admitted in the upgraded Department of Ophthalmology, SMS Medical College and Hospitals, Jaipur, Rajasthan, India from 1 June 2014 to 31 May 2015. Before commencing the study each patient was explained the investigative nature of the study, its merits and potential risks. The surgical technique was properly explained and a written informed consent was taken. The patients were admitted to the hospital, minimum one day prior to surgery for routine preoperative investigations.
The study was conducted on total of 90 patients who were further divided into three groups (30 in each group) according to ACD.
Inclusion Criteria
Patients with senile cataract, on the basis of ACD, were divided into three groups of 30 each (30 eyes).
Group A: ACD1 : 1.5 mm<ACD≤2.5 mm (shallow ACD)
Group B: ACD2 : 2.5 mm<ACD≤3.5 mm
Group C: ACD3: 3.5 mm<ACD≤4.5 mm (deep ACD)
Exclusion Criteria
History of previous ocular surgery, glaucoma, trauma, intraoperative complications such as posterior capsule rupture or nucleus drop, those who were not able to come for follow up.
All patients underwent complete systemic, clinical and ophthalmological evaluation.
Surgical Technique
Pupillary dilation with tropicamide 0.8% and phenylephrine 5% eye drops was done and peribulbar anaesthesia given. Superotemporally biplanar clear corneal incision was created using 2.8 mm keratome. Side port was created 45 degree from the main entry. Anterior chamber formed with viscoelastic substance (sodium hyaluronate) and continuous curvilinear capsulorrhexis was done. After hydrodissection/hydrodelineation, nucleus emulsification by direct chop technique was performed using Alcon Laureate with kelman type microtip. Cortical matter was removed with Irrigation/Aspiration (I/A) ultra sleeve tip. After filling the anterior chamber with viscoelastic, foldable intraocular lens (hydrophilic) with the recommended injector system was implanted into the eye. Viscoelastic was removed with irrigation and aspiration tip and corneal wounds were hydrated.
Surgery time was recorded starting from creating the side port to the end of stromal wound hydration. Effective phaco time, ultrasound power and corneal tunnel length were recorded.
Any case of intraoperative or postoperative complications, lead to patient’s exclusion from the study.
Postoperatively, all patients were prescribed with tobramycin 0.3%+dexamethasone 0.1% eye drops two hourly and tapered in six weeks. The follow up examinations were conducted on day one, one week, one month and three months postoperatively and endothelial cell count and Central Corneal Thickness (CCT) were recorded.
CCT was measured at the central cornea using the pachy mode of the specular microscope. While identifying the center of each endothelial cell, the cell density (cells/mm2) was computed on the basis of 100 identified cells taken from the picture. Endothelial cell loss was calculated by measuring the percentage decrease in endothelial cell density of the central cornea as follows: endothelial cell loss=(preoperative cell count postoperative cell count)/ (preoperative cell count×100%)3.
Statistical Analysis
Patient’s data were recorded and statistical analysis was done using paired t-test to compare preoperative and postoperative data and unpaired t-test to compare results between the three groups.
Results
[Table/Fig-1] shows that the mean ACD in Group A was 2.3±0.1 mm, in Group B was 3.1±0.2 mm and in Group C was 3.8±0.2 mm. The difference was statistically significant (p-value=0.001) between the groups. The difference of effective phaco time in between all three groups was statistically significant (p-value=0.02). In Group A, the mean phaco energy was 292.7±48.8 mJ while in Group B, it was 270.6±40.5 mJ and in Group C it was 244.0±32.2 mJ [Table/Fig-2].
Distribution of mean anterior chamber depth in all three groups.
| ACD (mm) | Group A | Group B | Group C | p-value |
|---|
| Mean ACD (mm) | 2.3 | 3.1 | 3.8 | 0.001 |
| S.D. | 0.1 | 0.2 | 0.2 |
| Maximum ACD (mm) | 2.49 | 3.47 | 4.28 |
| Minimum ACD (mm) | 1.98 | 2.73 | 3.52 |
Effective phaco time and phaco energy in all three groups.
| EPT (seconds) | Group A | Group B | Group C |
|---|
| Mean | 4.9 | 4.5 | 4.4 |
| S.D. | 0.8 | 0.6 | 0.5 |
| Phaco energy (Mean in mJ) | 292.7 | 270.6 | 244.0 |
| S.D. | 48.8 | 40.5 | 32.2 |
There was no statistically significant difference found in preoperatively central corneal thickness between all the three groups (p-value=0.61).
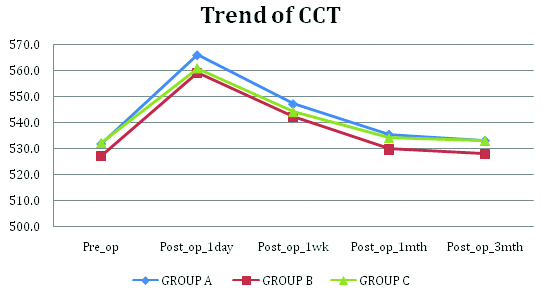
[Table/Fig-3] shows there was no statistically significant difference postoperatively in all the three groups (p-values postoperatively on 1st day, 1st week, one month and three months was 0.45, 0.70, 0.58 and 0.589 respectively).
Trend of central corneal thickness in all three groups.
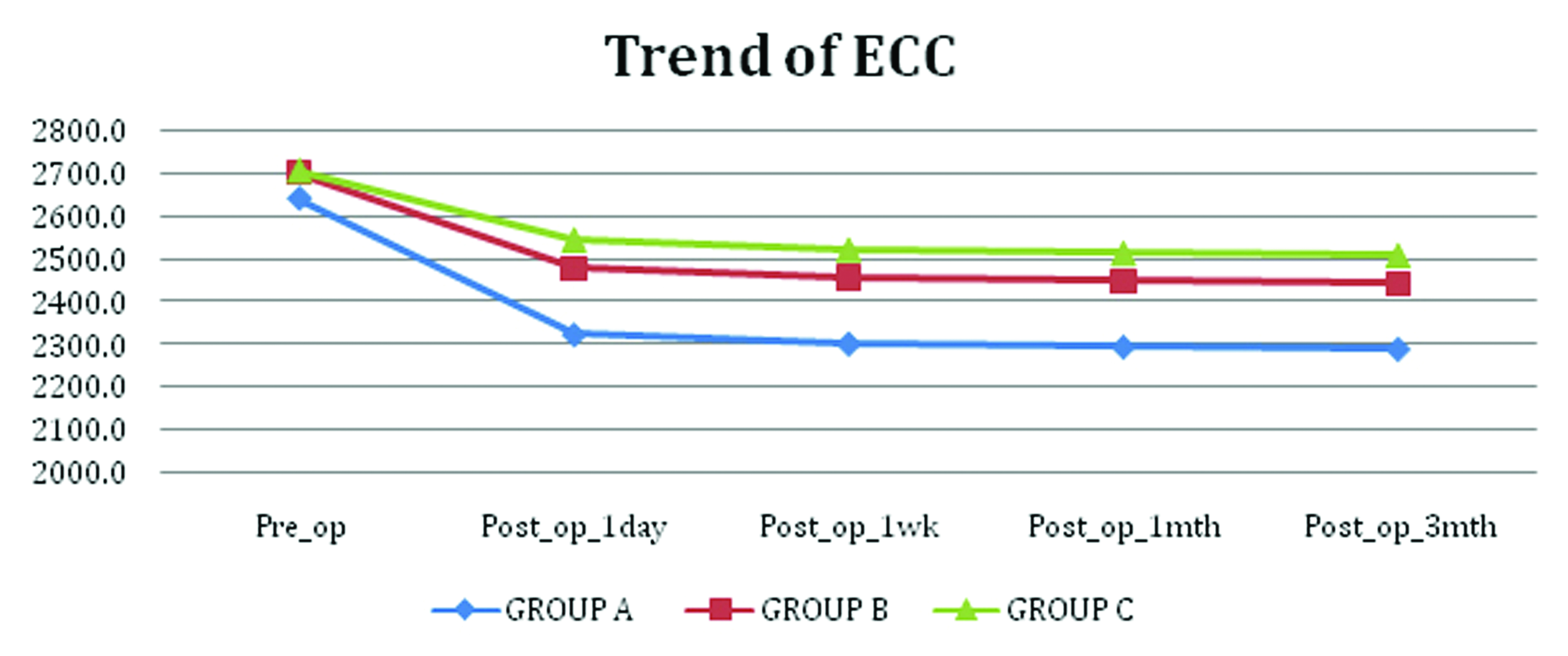
There was no statistically significant difference found in preoperatively endothelial cell counts between all the three groups (p-value=0.58).
There was statistically significant difference postoperatively in all the three groups (p-values postoperatively on 1st day, 1st week, one month and three months was 0.0024) [Table/Fig-4,5].
Trend of endothelial cell count in all three groups.
Trend of endothelial cell loss in between groups.
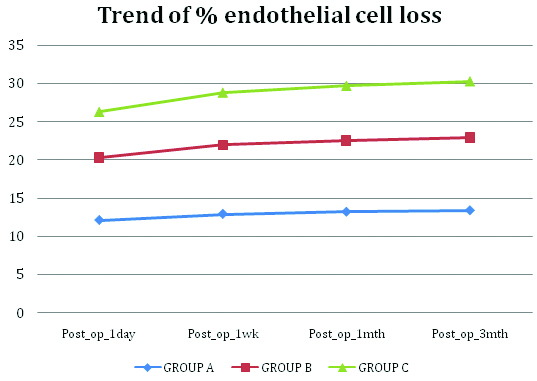
[Table/Fig-5]shows that in Group A, the mean endothelial cell loss postoperatively on 1st day, 1st week, one month and three months was 12.14±1.12%, 12.95±1.11%, 13.23±1.10% and 13.42±1.10% respectively.
The mean endothelial cell loss in Group B on 1st day, 1st week, one month and three months was 8.19±0.43%, 9.03±0.43%, 9.33±0.43% and 9.52±0.43% respectively.
In Group C, the mean endothelial cell loss on 1st day, 1st week, one month and three months was 5.96±0.26%, 6.82±0.26%, 7.12±0.26% and 7.32±0.26% respectively.
Discussion
Phacoemulsification has became the treatment of age related cataract due to small incision, which results in better control of postoperative astigmatism and more rapid recovery of visual acuity. As the phacoemulsificatiion procedure damages the corneal endothelial cells, the transparency of cornea becomes a major determinant of postoperative visual recovery.
A total of 90 eyes of 90 patients were evaluated in our study with the aim to study and assess the corneal endothelial cell density and central corneal thickness after phacoemulsification and IOL implantation, in three groups, divided according to ACD (Group A: 1.5 mm < ACD ≤2.5 mm, Group B: 2.5 mm < ACD ≤3.5 mm, Group C: 3.5 mm <ACD ≤ 4.5 mm).
Our study reports postoperative status of the corneal endothelium in three different anterior chamber depth groups and compares the status of the three groups.
In present study, the mean ACD in Group A was 2.3±0.1 mm, in Group B was 3.1±0.2 mm and in Group C was 3.8±0.2 mm. The difference was statistically significant. A p-value was <0.001 between the groups. A p-value between Group A v/s Group B was <0.001, between Group B v/s Group C was <0.001 and between Group A v/s Group C was <0.001.
Mean effective phaco time in group A was 4.9±0.8 seconds while in Group B, it was 4.5±0.6 seconds and in Group C it was 4.4±0.5 seconds.
The difference was statistically significant (p-value=0.02) between the groups. The difference was also statistically significant between Group A v/s Group B and Group A v/s Group C. A p-value was 0.04 and 0.01 respectively. The difference was not statistically significant between Group B v/s Group C (p-value=0.63).
Similar results were seen by Cho YK et al., [1]. The mean operation time in Group A was 18.06±3.10 seconds, in Group B was 17.36±2.79 seconds and in Groups C was 17.45±1.64 seconds. However, the difference between groups was not statistically significant (p>0.05) Mean phaco energy was also compared in all three groups. The mean phaco energy in Group A was 292.7±48.8 mJ, in Group B, it was 270.6±40.5 mJ and in Group C, it was 244.0±32.2 mJ. The difference was statistically significant when compared among three groups (p-value <0.001). However, the difference was not significant when compared between Group A v/s Group B. (p-value=0.06). The difference was also significant when compared between Group B v/s Group C and Group A v/s Group C (p-value <0.001).
In a study by Cho YK et al., it was seen that the mean phaco energy was considerably higher in Group A (1.5 mm<ACD≤2.5 mm) when compared to group C (3.5 mm<ACD≤4.5 mm) [1].
The mean Endothelial Cell Count (ECC) in Group A, preoperatively was 2642.7±294.6 cells/mm2, in Group B was 2702.6±304.9 cells/mm2 and Group C was 2706±174.5 cells/mm2.
A p-value between the three groups was 0.58. A p-value between Group A v/s Group B was 0.44, between Group A v/s C was 0.31, between Group B v/s Group C was 0.95. Thus, there was no difference in ECC preoperatively in all the three groups and also when compared between each two groups individually.
ECC postoperatively at intervals of day 1, one week, one month and three months was assessed. There was statistically significant difference postoperatively in all the three groups. (p-values postoperatively on 1st day, 1st week, one month and three months was 0.0024)
A p-value=0.03 when compared between Group A and Group B which was statistically significant and between Group A v/s Group C also significant (p-value <0.01). A p-value was 0.29 when compared between Group B v/s Group C that was not significant.
We calculated the percentage of endothelial cell loss at each follow up and found that in Group A, the mean endothelial cell loss postoperatively on day 1, 1st week, one month and three months was 12.14±1.12%, 12.95±1.11%, 13.23±1.10% and 13.42±1.10%. The mean endothelial cell loss was found to be increasing gradually on each follow up until it was stabilised at 3 months. The mean endothelial cell loss was highest between the preoperative and 1st postoperative day and decreased gradually between 1st day to one week, one week to one month and 1 month to 3 months. The mean endothelial cell loss in Group B and Group C also followed the same trend. The mean endothelial cell loss in Group B on day 1, 1st week, one month and three months was 8.19±0.43%, 9.03±0.43%, 9.33±0.43% and 9.52±0.43% respectively.
In Group C, the mean endothelial cell loss on day 1, 1st week, one month and three months was 5.96±0.26%, 6.82±0.26%, 7.12±0.26% and 7.32±0.26% respectively. It was observed that preoperatively there was no significant difference in the endothelial cell counts between the three groups, still the percentage of mean endothelial cell loss was significantly higher in Group A as compared to Group C at each follow up (p-value <0.01).
Similar results were seen by Hwang HB et al., [4]. The mean decrease in endothelial cell density at two months in the Group A (1.5 mm<ACD≤2.5 mm) was 12.94±3.16% and 9.61±2.96% in Group C (3.5 mm<ACD≤4.5 mm). The difference in cell density between these two groups was statistically significant (p<0.05).
Similar results were seen in a study conducted by Walkow T et al., [5]. Fifty consecutive patients scheduled for routine cataract surgery were selected prospectively for this clinical trial. After 12 months, the mean overall central endothelial cell loss in all eyes was 8.5%. However, a relationship between ACD and endothelial cell loss could not be demonstrated but it was stated that shorter eyes with short axial length have a significantly higher risk for greater endothelial cell loss.
The phacoemulsification surgery is performed in a limited, confined space; however, adequate space during surgery can decrease the risk of corneal endothelial cell damage by the procedure. Satisfactory surgical space is important for decreasing endothelial cell damage from the aforementioned risk factors. Within a shallow ACD, surgery can take place closer to the corneal endothelium. Therefore, we conclude that a deep ACD would correlate with lower endothelial cell loss during phacoemulsification surgery.
Conclusion
The study would have been more informative if the sample size were larger. If a longer follow up duration were given, the results could have been more informative.
Conclusion
To conclude we found that a shallow ACD would lead to phacoemulsification being performed closer to the endothelium, so that the corneal endothelium could be vulnerable to phacoemulsification energy and touch by surgical instruments. For this reason, eyes with shallow ACD are therefore associated with an increased endothelial cell loss than eyes with deep ACDs.