Left-sided Gastroschisis with Skeletal Deformities
Rajkumar Motiram Meshram1, Amruta Phatak2, Balaji Bhise3, Avinash Chichkhede4, Duhita Sengupta5
1 Associate Professor, Department of Paediatrics, Government Medical College, Nagpur, Maharashtra, India.
2 Postgraduate Student, Department of Paediatrics, Government Medical College, Nagpur, Maharashtra, India.
3 Postgraduate Student, Department of Paediatrics, Government Medical College, Nagpur, Maharashtra, India.
4 Postgraduate Student, Department of Paediatrics, Government Medical College, Nagpur, Maharashtra, India.
5 Postgraduate Student, Department of Paediatrics, Government Medical College, Nagpur, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rajkumar Motiram Meshram, 219, Shilpa Society, Behind Ajanta Marble, Manish Nagar, Main Road, Nagpur, Maharashtra, India.
E-mail: dr_rajmeshram@rediffmail.com
Gastroschisis is a full thickness congenital defect in the abdominal wall. It has strong association with young maternal age of first para first gesta and usually in premature male babies. Though the pathogenesis is unclear, vascular insult during embryonic period is the most accepted theory. Variable length of intestine and occasionally parts of other abdominal organs are herniated outside the abdominal wall with no covering membrane or sac. It is commonly associated with gastrointestinal anomalies but extraintestinal anomalies are rare. An early preterm male neonate of 25-year-old first para first gesta mother without significant antenatal events exhibited left-sided gastroschisis with evisceration of both small and large intestine with stomach. He had absent digits of left foot except a single appendage, Congenital Talipes Equino Varus (CTEV) on right foot and pelvic deformity. Early identification of this defect by improving antenatal care and ultrasound examination helps to identify high risk patients in order to choose a specialised centre to optimise their outcome.
Abdominal wall defect, Congenital anomalies, Neonate, Prenatal ultrasound
Case Report
A 1200 gm early preterm male neonate was born by spontaneous vaginal delivery to a 25-year-old primigravida mother was presented to the Department of Paediatrics. Mother was non consanguineously married and from low socioeconomic class. She was in regular antenatal clinic and received iron, folic acid and calcium supplementation but antenatal ultrasound was not performed. She had no history of pregnancy induced hypertension, pregestational or gestational diabetes. There was no history of smoking or tobacco chewing. There was no history of abortion and there was no family history of fetal anomalies. Respiratory efforts after birth were poor, baby could not be salvaged and died within 30 minutes of birth.
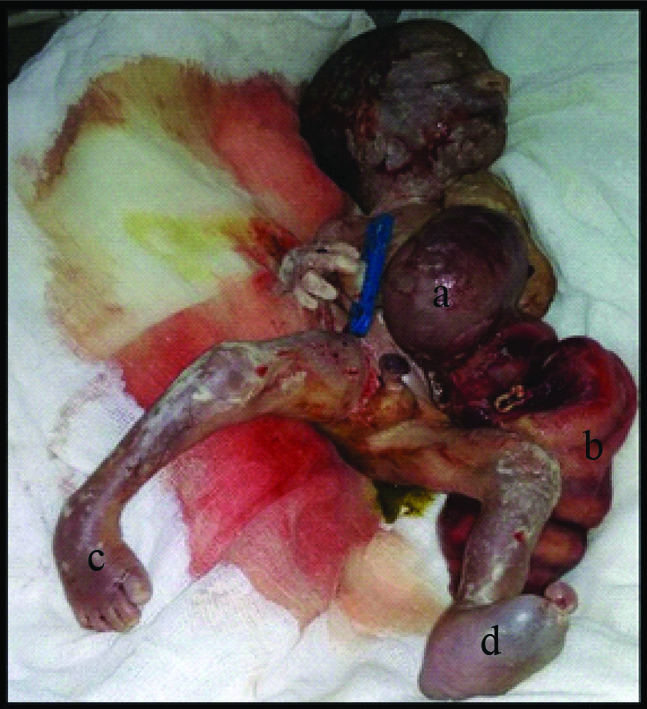
There was a small (2.5 cm) defect in the left paraumbilical area through which small intestine, large intestine and stomach had herniated. There was an associated left thoracic cage abnormality (some ribs could not be palpated) and pelvic deformity. Baby did not exhibit digits of left foot except a single appendage and had CTEV in right foot [Table/Fig-1].
a) Herniation of stomach, small and large intestine with bilateral foot deformity: stomach; b) intestine; c) congenital talipes equino varus; d) deformity of left foot.
Discussion
Between 4 to 16 weeks of gestational age, the gastrointestinal tract develops from the embryonic foregut, midgut and hindgut. Gastroschisis and omphalocele are two commonly described anterior abdominal wall defect. Gastroschisis is a full thickness congenital defect in the abdominal wall usually to the right of a normally inserted umbilical cord. The incidence of gastroschisis appears to be increasing worldwide and it is approximately 1-4.9 per 10,000 births [1,2]. More than half of the cases are premature births and mainly affect male babies of first para first gesta mothers [3,4]. Though, the aetiology of gastroschisis is unclear, various theories (vascular insult, disorders of right-left axis orientation, and polymorphisms of several genes) have been proposed [5,6]. It has a strong association with young maternal age, cigarette smoking, use of illicit drugs, over the counter vasoactive drugs, environmental toxins and low socioeconomic level [7,8]. Young maternal age has been consistently reported as a risk factor. The anomalies occur at four times the baseline rate in women younger than 20 years of age [2].
Two types, simple and complex gastroschisis have been described in literature [9]. Simple gastroschisis translates into uncompromised bowel where as complex denotes bowel with necrosis, atresia or perforation. Variable amount of intestine and occasionally parts of other abdominal organs are herniated outside the abdominal wall with no covering membrane or sac. They usually have a normal karyotype. Prenatal ultrasound and four fold elevated maternal serum alfa-fetoprotein level facilitates early diagnosis and hence allows the family time to make preparation for infant’s care after birth. Very few cases of left-sided gastroschisis are presented in the literature [10].
Patients with gastroschisis have associated anomalies in 10-20% and most of the significant anomalies are pertaining to the gastrointestinal tract like stenosis, atresia, malrotation and volvulus. This is in contrast to patients with omphalocele who have associated anomalies in 50-60% and mostly of extraintestinal like cardiac, genito-urinary and chromosomal anomalies like Trisomy 18, 13 and 21. Omphalocele is also a part of Beckwith-Wiedemann syndrome, Pentalogy of Cantrell, Meckel-Gruber syndrome and the lethal cleft palate-Omphalocele syndrome. Hombalkar NN et al., reported presence of caecal agenesis with short gut and malrotation of the intestine in a patient with left-sided gastroschisis [10]. Evisceration of other abdominal organs like stomach, liver, gall bladder are reported by various authors but anomalies of urogenital tract, heart and nervous system are rarely observed [11,12]. Similar to this case Dharmraj M and Verma AP, reported case with deformed left feet and toes, accompanied by rudimentary male genital organ [13]. Genetic causes of gastroschisis are poorly explained but some authors observed gastroschisis in successive sibling and in conjoint twins suggestive of an interplay of genetic and environmental factors responsible for such defects [14,15].
Gastroschisis is often diagnosed before birth by ultrasound with a specificity >95% at about 20 weeks of gestation [16]. This wall defect shows an alpha-fetoprotein elevation in the amniotic fluid and consequently in the maternal serum and it is also almost always markedly elevated in such a kind of defect. The prenatal diagnosis of gastroschisis allows talking with families about the condition, treatment and prognosis of the fetus. Early identification may help to identify high risk patients in order to choose a specialised centre to optimise their outcome.
Conclusion
This was a case of left-sided gastroschisis with skeletal deformities. Since, early prenatal diagnosis can improve prognosis, we emphasise the importance of antenatal care to all pregnant women, especially high risk. Facilities for early and precise diagnosis and treatment should be provided by means of establishing advanced centers and improving the expertise in the diagnosis and management of fetal anomalies.
[1]. Loane M, Dolk H, Bradury I, Increasing prevalence of gastroschisis in Europe 198-2002: a phenomenon restricted to younger mothers?Pediatr Perinat Epidemiol 2007 21(4):363-69.10.1111/j.1365-3016.2007.00820.x17564594 [Google Scholar] [CrossRef] [PubMed]
[2]. Fillingham A, Rankin J, Prevalence, prenatal diagnosis and survival of gastroschisisPrenat Diagn 2008 28(13):1232-37.10.1002/pd.215319039824 [Google Scholar] [CrossRef] [PubMed]
[3]. Chircor L, Mehedinti R, Hineu M, Risk factors related to omphalocele and gastroschisisRom J Morphol Embryol 2009 50(4):645-69. [Google Scholar]
[4]. Briganti V, Luvero D, Gulia C, Piergentili R, Zaami S, Buffone EL, A novel approach in the treatment of neonatal gastroschisis: a review of literature and a single centre experienceJ Matern Fetal Neonatal Med 2018 31(9):1234-40.10.1080/14767058.2017.131185928337935 [Google Scholar] [CrossRef] [PubMed]
[5]. Mandelia A, Aetiology of left sided gastroschisisAfr J Pediatr Surg 2015 12(2):15910.4103/0189-6725.16044026168760 [Google Scholar] [CrossRef] [PubMed]
[6]. Feldkamp ML, Carey JC, Sadler TW, Development of gastroschisis: review of hypothesis, a novel hypothesis, and implication for researchAm J Med Genet A 2007 143(7):639-52.10.1002/ajmg.a.3157817230493 [Google Scholar] [CrossRef] [PubMed]
[7]. Stevenson RE, Rogers RC, Chandler JC, Gauderer MW, hunter AG, Escape of the yolk sac: a hypothesis to explain the embrogenesis of gastroschisisClin Genet 2009 75(4):326-33.10.1111/j.1399-0004.2008.01142.x19419415 [Google Scholar] [CrossRef] [PubMed]
[8]. Toris CP, Christianson RE, Iovannisci DM, Shaw GM, Lammer EJ, Selected gene polymorphisms and their interaction with maternal smoking, as risk factors for gastroschisisBirth Defects Res A Clin Mol Teratol 2006 76(10):723-30.10.1002/bdra.2031017051589 [Google Scholar] [CrossRef] [PubMed]
[9]. Bradnoch TJ, Marven S, Owen A, Johnson P, Kurinczuck JJ, Spark P, Gastroschisis: one year outcomes from national cohort studyBMJ 2011 343:d674910.1136/bmj.d674922089731 [Google Scholar] [CrossRef] [PubMed]
[10]. Hombalkar NM, Rafe A, Prakash GD, Left-sided gastroschisis with caecal agenesis: a rare case reportAfr J Paediatr Surg 2015 12(1):74-75.10.4103/0189-6725.15098925659556 [Google Scholar] [CrossRef] [PubMed]
[11]. Alaani S, Report of three cases of unusual anterior abdominal wall defects in Fallujah general hospital during the year 2010JIMA 2012 44(1):01-07.10.5915/44-1-10354PMC3708633 [Google Scholar] [CrossRef] [PubMed]
[12]. Nirmaladevi M, Mathivanan D, Kurup S, Gastroschisis with skeletal deformities- a case report with review of literature.Int J Health Sci Res 2015 5(2):402-06. [Google Scholar]
[13]. Dharmraj M, Verma AP, Gastroschisis associated with lower limb and spinal congenital anomaliesJ Clin Neonatol 2012 1(4):217-20.10.4103/2249-4847.10600524027731 [Google Scholar] [CrossRef] [PubMed]
[14]. Snelling CM, Davies GA, Isolated gastroschisis in successive sibling: a case report and review of the literatureJ Obstet Gynaecol Can 2004 26(6):591-93.10.1016/S1701-2163(16)30378-4 [Google Scholar] [CrossRef]
[15]. Sudhakar G, Annapurna P, Sasank R, Narasimhulu K, Gastroschisis in both conjoint twinsJ Case Rep 2015 5(1):141-43.10.17659/01.2015.0035 [Google Scholar] [CrossRef]
[16]. Barisic I, Clementi M, Hausler M, Gjergja R, Kern J, Stoll C, valuation of prenatal ultrasound diagnosis of fetal abdominal wall defects by 19 European registriesUltrasound Obstet Gynecol 2001 18(4):309-16.10.1046/j.0960-7692.2001.00534.x11778988 [Google Scholar] [CrossRef] [PubMed]