Continuity of Care Following Intraoperative Cardiac Arrest due to Thymoglobulin®-induced Anaphylaxis
Jose R Navas-Blanco1, Stephanie A Cook2, David A Rico-Mora3, Murali S Patri4, Trevor J Szymanski5
1 Resident, Department of Anaesthesia, Pain Management and Perioperative Medicine, Henry Ford Hospital, Detroit, Michigan, USA.
2 Resident, Department of Anaesthesia, Pain Management and Perioperative Medicine, Henry Ford Hospital, Detroit, Michigan, USA.
3 Resident, Department of Anaesthesia, Pain Management and Perioperative Medicine, Henry Ford Hospital, Detroit, Michigan, USA.
4 Attending Physician, Department of Anaesthesia, Pain Management and Perioperative Medicine, Division of Interventional Pain Management, Henry Ford Hospital, Detroit, Michigan, USA.
5 Attending Physician, Department of Anaesthesia, Pain Management and Perioperative Medicine, Division of Cardiothoracic Anaesthesia, Henry Ford Hospital, Detroit, Michigan, USA.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jose R Navas-Blanco, Resident, Department of Anaesthesia and Perioperative Medicine, Henry Ford Hospital, 2799, West Grand Boulevard, CFP-341, Detroit, Michigan, USA.
E-mail: jnavas1@hfhs.org
Rabbit anti-thymocyte globulin (Thymoglobulin®, Sanofi-Aventis, Quebec, Canada) a purified gamma immune globulin obtained from the serum of rabbits immunised against human thymocytes, is widely used as an immunosuppressant agent to prevent acute rejection during solid organ transplantation. Anaphylaxis after first-time exposure to the drug is rare, but may be associated with devastating consequences. We present the case of a patient undergoing renal transplantation who developed intraoperative cardiac arrest due to severe allergic reaction immediately after initiation of Thymoglobulin® intravenous infusion. The patient was successfully resuscitated, but developed chronic chest pain from left-sided rib fractures sustained during chest compressions, and was evaluated by the same senior staff anaesthesiologist as an outpatient in the pain clinic.
A high level of suspicion from anaesthesia providers is paramount in the diagnosis and management of intraoperative drug-induced severe allergic reactions, furthermore there is an opportunity for continued care of these patients by anaesthesia providers beyond the return of spontaneous circulation.
Cardiopulmonary resuscitation complication, Rabbit anti-thymocyte globulin, Severe drug-induced allergic reaction
Case Report
A 51-year-old male with medical history of end stage renal disease presented to our facility for deceased donor kidney transplant. His medical history was significant for uncontrolled hypertension, end stage renal disease on peritoneal dialysis, had no documented allergies, and denied prior anaesthetic complications. Preoperative examination revealed a functionally independent patient with stable vital signs, body mass index of 26.4 kg/m2, and normal preoperative airway and physical exams. Baseline laboratory analyses included: potassium 4.7 mmol/L, creatinine 1016 μmol/L, and blood urea nitrogen 15 mmol/L. Intraoperatively, general anaesthesia was induced with propofol (200 mg), fentanyl (100 μg) and lidocaine (80 mg), followed by uneventful tracheal intubation after administration of rocuronium (80 mg). Anaesthesia was maintained with isoflurane. A left internal jugular central venous catheter was placed for haemodynamic monitoring. Antibiotic prophylaxis was administered (cefazolin, 2 gm), followed by methylprednisolone (250 mg) and diphenhydramine (50 mg). Incision was made fifty minutes after induction of general anaesthesia.
Ten minutes after the incision, Thymoglobulin® was started (125 mg intravenous infusion at 31.2 mg/hr) via the central venous line. Three minutes after initiation of Thymoglobulin®, the patient developed sudden hypotension (blood pressure reduced from 145/80 mmHg to 75/46 mmHg), followed by a decrease in the end tidal carbon dioxide (from 30 mmHg to 7 mmHg) and tachycardia (heart rate 130-137 beats per minute). Immediately, Thymoglobulin® infusion and volatile anaesthetic agent were discontinued, and Cardiopulmonary Resuscitation (CPR) was initiated for Pulseless Electrical Activity (PEA). Chest compressions were started, intravenous bolus of epinephrine (1 mg) was administered and a norepinephrine infusion was initiated (20 μg/min) via central access.
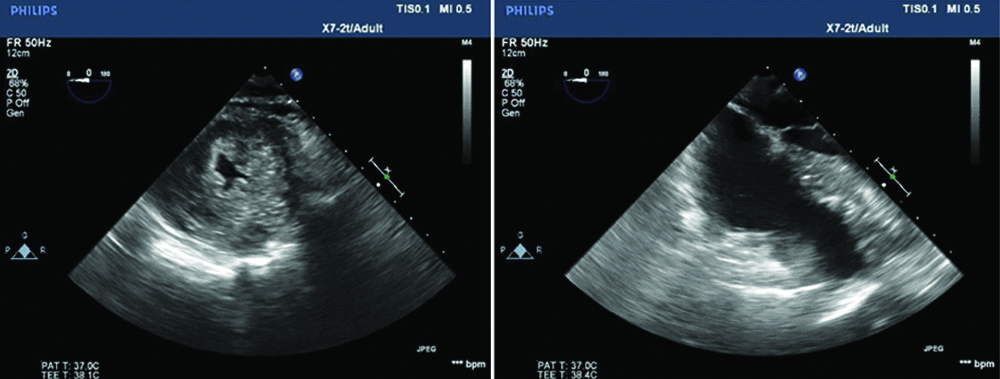
Within 10 minutes of the onset of CPR the patient regained pulsatility on the arterial line, but remained tachycardic and hypotensive. Breath sounds were difficult to auscultate. Transoesophageal Echocardiography (TOE) revealed a hyperdynamic, severely underfilled left ventricle, without evidence of right ventricle strain, regional wall motion abnormalities, aortic root dilation or pericardial effusion [Table/Fig-1]. Left hemithorax needle decompression and chest tube placement failed to reveal the presence of haemothorax or pneumothorax. The patient received three units of packed red blood cells and one unit of fresh frozen plasma with marked improvement of haemodynamics and left ventricle filling on TOE.
Transoesophageal echocardiographic imaging of the patient during cardiac arrest, showing severely underfilled left ventricle in the midoesophageal short axis view (left), no evidence of pericardial effusion and normal right ventricle dimensions in the midoesophageal four chamber view (right).
The procedure was aborted and the patient was taken to the intensive care unit, intubated and sedated. Postoperatively, allergy and immunology specialists were consulted and the patient was started on diphenhydramine and prednisone as per their recommendations. Serum tryptase levels drawn at 0, 6 and 12 hours were: 549 ng/mL, 373 ng/mL and 141 ng/mL respectively (normal range: <11 ng/mL). Physical exam showed significant swelling around neck, tongue, face, lips, and oral mucosae. The patient was extubated on postoperative day one and discharged home on postoperative day five without sequelae.
Over the next two months, the patient developed persistent left-sided chest pain that worsened on deep inspiration. Chest radiography revealed a fracture of the left sixth rib, which was attributed to chest compressions as part of the resuscitative efforts during the cardiac arrest. He was referred to pain management services for management of intercostal neuralgia and was started on gabapentin and cyclobenzaprine for pain control; with the option of fluoroscopy-guided intercostal nerve block, should the pain persist. The same staff anaesthesiologist that cared for the patient for the aborted kidney transplant, was the pain medicine specialist consulted for management of chronic rib pain. The patient’s pain improved with two weeks of conservative therapy.
Discussion
Rabbit anti-thymocyte globulin (Thymoglobulin®) constitutes the purified IgG fraction obtained from the serum of rabbits immunised against human thymocytes [1]. Currently Thymoglobulin® represents the best therapeutic intervention to prevent acute organ rejection, with the best long-term graft survival profile among transplant recipient patients [2,3]. Intraoperative severe allergic reactions, both immune (anaphylactic, IgE mediated) and non-immune (anaphylactoid, non-IgE mediated), represent potential challenges to anaesthesiologists, with latex and neuromuscular blocking agents being the most common culprits [4,5]. Anaphylactic reactions against rATG are exceedingly rare (estimated to be <3%) [1,2,6]. Life-threatening clinical presentations have been previously described in the literature [Table/Fig-2][1,2,5,7].
Previous reports of anaphylaxis against rabbit anti-thymoglobulin.
| Reference | Patient Age, Gender | Procedure | Reaction to Thymoglobulin® |
|---|
| Brabant S et al., [1] | 24-year-old, male | Renal Transplant | Anaphylactic reaction |
| Kandil E et al., [2] | 39-year-old, female | Renal Transplant | Anaphylactic reaction |
| Sebeo J et al., [5] | 13-year-old, female | Renal Transplant | Anaphylactoid reaction |
| Roncati L et al., [7] | 62-year-old male | Liver Transplant | Anaphylactic reaction, intraoperative death |
Circulatory support is the paramount component during cardiac arrest and while chest compressions are the principal strategy in maintaining adequate perfusion to vital organs, they are related to skeletal injuries with rib fractures representing the most common direct complication [8-10]. Beom JH et al., described a retrospective analysis of 185 patients with both in and out-of-hospital cardiac arrest who had successful resuscitation and rib fractures were present in 62-78% of the population analysed, with the majority having multiple rib fractures. Additionally, sternum fractures were present in 26-30% of the patients. The authors concluded that performing deeper and faster chest compressions were associated with increased return of spontaneous circulation, but also increased risk of skeletal injuries [8].
In the case presented, we based our clinical diagnosis following the algorithm recommended by the American Heart Association for Advance Cardiac Life Support [9], as such: TOE evaluation was performed and showed profound hypovolemia without evidence of myocardial ischaemia (no regional wall motion abnormalities), pericardial effusion (absent increased fluid in pericardial space), aortic dissection (no signs of aortic root dilation), or pulmonary embolism (absent right ventricle strain or d-shape). Tension pneumothorax and haemothorax, potentially related to central venous line placement, were unlikely following left thorax needle decompression and chest tube placement without evidence of air or blood in the chest. Ultimately, the diagnosis of severe intraoperative allergic reaction was made clinically and the patient’s haemodynamics improved significantly after aggressive fluid resuscitation and vasopressor therapy. Diagnosis was confirmed during recovery in the intensive care unit with elevated tryptase levels. Due to the magnitude of the allergic reaction and the presence of significantly elevated tryptase levels, the Allergy and Immunology team was involved for further expert input and concluded that the patient experienced an anaphylactic shock secondary to Thymoglobulin®, associated to a cytokine storm, although further testing is necessary (skin test for Thymoglobulin®, IgE levels), to exclude an anaphylactoid reaction as a possible cause.
During the recovery period the patient had persistent left-sided chest pain related to a left sixth rib fracture and intercostal neuralgia. Non-opioid therapy was prescribed and an ultrasound-guided intercostal nerve block was offered, if the symptoms persist or recur.
Conclusion
While this case highlights the different clinical roles the same anaesthesiologist may play in the care of a patient (management of intraoperative general anaesthesia and outpatient acute/chronic pain management), the case also identifies another opportunity for the anaesthesiologist. Evaluation by an anaesthesiologist postoperatively, but prior to discharge, may have provided an opportunity to improve medical management of the patient’s CPR related rib fracture pain. Because musculoskeletal injuries are common in patients who survive CPR, there may be an opportunity to identify patients that have undergone in-hospital or out-of-hospital chest compressions, and have an anaesthesiologist participate in the development of a multimodal plan for pain prior to discharge from the hospital.
[1]. Brabant S, Facon A, Provôt F, Labalette M, Wallaert B, Chenivesse C, An avoidable cause of thymoglobulin anaphylaxisAllergy Asthma Clin Immunol 2017 13:1310.1186/s13223-017-0186-928250777 [Google Scholar] [CrossRef] [PubMed]
[2]. Kandil E, Alabbas H, Distant D, Anaphylaxis thymoglobulin®: a case report and literature reviewJ La State Med Soc 2009 161(5):279-81. [Google Scholar]
[3]. Martins L, Fonseca I, Almeida M, Henriques AC, Dias L, Sarmento AM, Immunosuppression with antithymocyte globulin in renal transplantation: better long-term graft survivalTransplant Proc 2005 37(6):2755-58.10.1016/j.transproceed.2005.05.00316182802 [Google Scholar] [CrossRef] [PubMed]
[4]. Mertes PM, Laxenaire MC, Alla F, rouped’ Etudes des Réactions Anaphylactoédes Peranesthésiques. Anaphylactic and anaphylactoid reactions occurring during anaesthesia in France in 1999-2000Anaesthesiology 2003 99(3):536-45.10.1097/00000542-200309000-0000712960536 [Google Scholar] [CrossRef] [PubMed]
[5]. Sebeo J, Ezziddin O, Eisenkraft JB, Severe anaphylactoid reaction to thymoglobulin in a pediatric renal transplant recipientJ Clin Anesth 2012 24(8):659-63.10.1016/j.jclinane.2012.04.01423164644 [Google Scholar] [CrossRef] [PubMed]
[6]. Millar MM, Grammer LC, Case reports of evaluation and desensitization for anti-thymocyte globulin hypersensitivityAnn Allergy Asthma Immunol 2000 85(4):311-16.10.1016/S1081-1206(10)62535-5 [Google Scholar] [CrossRef]
[7]. Roncati L, Barbolini G, Tiziana Scacchetti A, Busani S, Maiorana A, Unexpected death: anaphylactic intraoperative death due to thymoglobulin carbohydrate excipientForensic Sci Int 2013 228(1-3):e28-32.10.1016/j.forsciint.2013.02.03623540837 [Google Scholar] [CrossRef] [PubMed]
[8]. Beom JH, You JS, Kim MJ, Seung MK, Park YS, Chung HS, Investigation of complications secondary to chest compressions before and after the 2010 cardiopulmonary resuscitation guideline changes by using multi-detector computed tomography: a retrospective studyScand J Trauma Resusc Emerg Med 2017 25(1):810.1186/s13049-017-0352-628122604 [Google Scholar] [CrossRef] [PubMed]
[9]. Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, Part 7: adult advanced cardiac life support. 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular CareCirculation 2015 132(suppl 2):S444-464.10.1161/CIR.000000000000026126472995 [Google Scholar] [CrossRef] [PubMed]
[10]. Zaw AA, Murry J, Hoang D, Chen K, Louy C, Bloom MB, Epidural analgesia after rib fracturesAm Surg 2015 81(10):950-54. [Google Scholar]