Unilateral Pulmonary Aplasia with Dextroposition of Heart: A Case Report
Sanjib Kumar Das1, Ipsita Acharya2, Jayashree Mohanty3, Sasmita Parida4, Basanta Manjari Swain5
1 Junior Resident, Department of Radiodiagnosis, SCB Medical College and Hospital, Cuttack, Odisha, India.
2 Junior Resident, Department of Radiodiagnosis, SCB Medical College and Hospital, Cuttack, Odisha, India.
3 Professor, Department of Radiodiagnosis, SCB Medical College and Hospital, Cuttack, Odisha, India.
4 Associate Professor, Department of Radiodiagnosis, SCB Medical College and Hospital, Cuttack, Odisha, India.
5 Associate Professor, Department of Radiodiagnosis, SCB Medical College and Hospital, Cuttack, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ipsita Acharya, Junior Resident, Department of Radiodiagnosis, SCB Medical College and Hospital, Cuttack-753007, Odisha, India.
E-mail: dripsitaacharya@gmail.com
‘Pulmonary Aplasia’ is a rare condition where there is absence of unilateral or bilateral lung tissue with a rudimentary bronchus which separates it from the similar looking ‘Pulmonary Agenesis’. The aetiology is not completely understood, though a defect in chromosome number two is often associated. Failure of development of primary lung bud leads to aplasia/agenesis. It is often associated with other anomalies involving skeletal, cardiovascular, genitourinary and gastrointestinal system. We present a case of right sided pulmonary aplasia with dextroposition/levorotation of heart in a 10-month-old female child.
Levorotation of heart, Lung herniation, Respiratory distress
Case Report
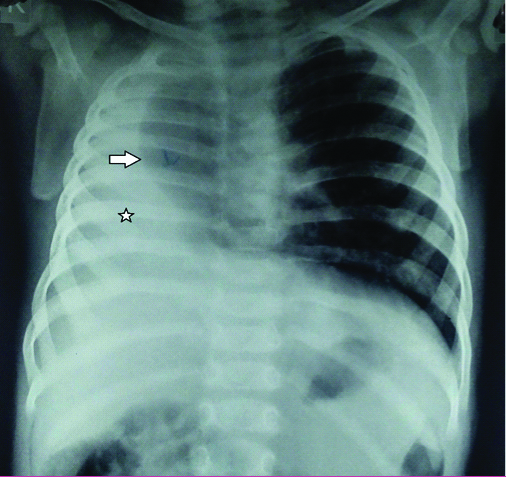
A 10-month-old female child born from non-consanguineous Indian parents presented to the department of Radiodiagnosis, with history of recurrent episodes of fever and shortness of breath shortly after birth. Being from tribal areas of Odisha, the mother never had any antenatal ultrasound. There was no significant history of prenatal medication. Birth history was uneventful and the baby cried immediately after birth. She was normal at birth, but developed on and off fever after three months of age. Previous child birth was uneventful and the last baby is 3-year-old and doing well. The baby was unsuccessfully treated at many peripheral hospitals and finally referred to us. On examination, there was low grade fever with signs of respiratory distress. Respiratory rate was 52 per minute with subcostal retraction and nasal flaring. There was tachycardia. Echocardiography report suggested dextrocardia. Chest X-ray revealed homogenous hyperopacity over right lung field with mild mediastinal shift to right [Table/Fig-1].
Chest X-ray PA view shows complete whiteout of right hemithorax (asterisk) with mild tracheal deviation to right and lucency over medial side of right lung suggesting lung herniation (arrow).
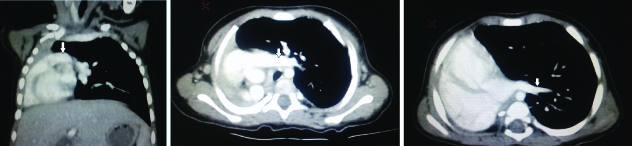
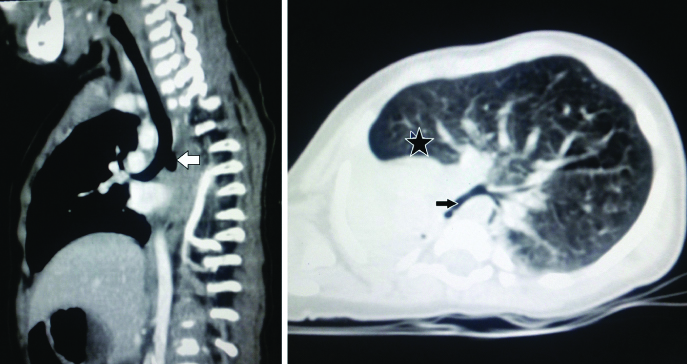
Radiolucency was noted on the medial aspect of right lung field corresponding to left lung herniation. Cardiac shadow could not be recognised on chest X-ray. A provisional diagnosis of right lung whiteout was given. Foreign body entrapment in the main bronchus was suspected with pulmonary aplasia/agenesis as a close differential. Contrast enhanced CT Scan was advised to look for the exact cause which showed absence of right lung tissue with a rudimentary right main bronchus [Table/Fig-2a-c,3a,b]. Right pulmonary artery and vein were also absent. Cardiac apex was on the left side suggesting dextroposition rather than dextrocardia of heart. A final diagnosis of “Right lung aplasia with dextroposition” was given. Symptomatic treatment was given in paediatrics department. Bag and mask ventilation and endotracheal intubation were done for supportive breathing. Patient was observed for eight days in the hospital and then discharged. Patient was being followed-up. She was doing well with occasional low grade fever as seen in the last follow up.
a) Coronal CT image showing absence of right lung tissue with hyperinflated left lung. Left pulmonary artery (arrow); b) Axial CT image showing similar findings as in Table/Fig-2a arrow-left pulmonary artery; c) Axial image showing absence of right lung with hyperinflated left lung herniating to right side and left pulmonary vein (arrow). Right pulmonary artery and vein were absent.
a) Sagital oblique CT image showing rudimentary right bronchus (arrow); b) Axial CT image in lung window shows absence of right lung with rudimentay right main bronchus (arrow) and herniating left lung (asterisk).
Discussion
Lung development starts as early as four weeks of gestation from respiratory diverticulum arising from foregut. Defect in development can lead to pulmonary hypoplasia, aplasia or agenesis [1]. The later, being the severest, presents with complete absence of lung tissue, bronchus and vascular supply. In pulmonary aplasia, rudimentary bronchus will be present with absence of pulmonary tissue and vascular supply while pulmonary hypoplasia shows hypodevelopment of pulmonary tissue, bronchial and vascular supply [2,3]. Bilateral pulmonary agenesis is often fatal and even 50% of unilateral lung agenesis patients die within five years of diagnosis [4]. Associated anomalies of cardiovascular, skeletal (limb and vertebral anomalies), genitourinary and gastrointestinal system (tracheoesophageal fistula, imperforate anus) may be noted. Unilateral pulmonary aplasia is often associated with malposition of heart in the form of dextrocardia and dextroposition [5].
Antenatal diagnosis is often a challenge to the radiologist, though experienced radiologists can diagnose cardiac malposition with unilateral pulmonary agenesis with little effort [5].
Shortly after birth patients usually present with respiratory distress with recurrent infections. Signs of respiratory distress such as subcostal and intercostal retraction and nasal flaring with decreased air entry to one side of chest on auscultation leads to suspicion of this congenital anomaly [4]. Echocardiography often elicits the malpositioned heart.
Chest X-ray in a case of pulmonary aplasia shows unilateral homogenous hyperopacity with compensatory hyperinflation and herniation of the contralateral lung, elevation of ipsilateral dome of diaphragm and mediastinal shift. Cardiac malpositions such as dextrocardia or dextroposition may be noted [4].
Contrast enhanced CT scan shows absence of lung tissue with rudimentary main bronchus and absence of ipsilateral vascular supply. Compensatory hyperinflation of contralateral lung is noted with herniation to affected side. Pulmonary artery and vein of the opposite side are often normal. Mediastinal and cardiac shift is often seen [6].
A recent retrospective study from Barcelona that studied 60 cases of pulmonary hypoplasia from 1995 to 2014 found a mortality rate of 47% in the first 60 days of life and upto 75% in the first day of life [7].
Management usually involves symptomatic treatment of the cases. In case of unsuccessful symptomatic treatment, ipsilateral upward translocation of diaphragm can be helpful [8].
Total lung atelectasis can sometimes mimic aplasia of lung, but bronchi and bronchioles can be traced in these cases [9]. Pneumonectomy can also be confused with aplasia unless proper history is taken.
Conclusion
Radiologists should always keep pulmonary agenesis/aplasia in a newborn or infant with respiratory distress, recurrent infections and unilateral opacity on chest X-ray and associated anomalies should always be sought for. Most of the cases are treated symptomatically.
[1]. DiFiore JW, Wilson JM, Lung developmentSemin Pediatr Surg 1994 3(4):221-32. [Google Scholar]
[2]. Kisku KH, Panigrahi MK, Sudhakar R, Nagarajan A, Ravikumar R, Daniel JR, Agenesis of lung-A report of two casesLung India 2008 25(1):28-30.10.4103/0970-2113.4413620396661 [Google Scholar] [CrossRef] [PubMed]
[3]. Boyden E, Developmental anomalies of the lungAM J Surg 1955 89(1):79-88.10.1016/0002-9610(55)90510-9 [Google Scholar] [CrossRef]
[4]. Nandan D, Bhatt GC, Dewan V, Pongener I, Complete right lung agenesis with dextrocardia: An unusual cause of respiratory distressJ Clin Imaging Sci 2012 2:8110.4103/2156-7514.10514023393637 [Google Scholar] [CrossRef] [PubMed]
[5]. Zhang Y, Fan M, Ren WD, Xie LM, Ding CW, Sun W, Prenatal diagnosis of fetal unilateral lung agenesis complicated with cardiac malpositionBMC Pregnancy and Childbirth 2013 13:7910.1186/1471-2393-13-7923530545 [Google Scholar] [CrossRef] [PubMed]
[6]. Mendelson DS, Hahn P, Cohen BA, Padilla ML, Hypoplasia of the lung: CT appearanceMt Sinai J Med 1986 53(4):297-98. [Google Scholar]
[7]. Delgado-Peña YP, Torrent-Vernetta A, Sacoto G, de Mir-Messa I, Rovira-Amigo S, Gartner S, Pulmonary hypoplasia: An analysis of cases over a 20-year periodAn Pediatr (Barc) 2016 85(2):70-76.10.1016/j.anpedi.2015.10.00826625967 [Google Scholar] [CrossRef] [PubMed]
[8]. Krivchenya DU, Rudenko EO, Lysak SV, Dubrovin AG, Khursin VN, Krivchenya TD, Lung aplasia: anatomy, history, diagnosis and surgical managementEur J Pediatr Surg 2007 17(4):244-50.10.1055/s-2007-96520017806020 [Google Scholar] [CrossRef] [PubMed]
[9]. Yetim TD, Bayaroğullari H, Yalçin HP, Arıca V, Arıca SG, Congenital agenesis of the left lung: a rare caseJ Clin Imaging Sci 2011 1:4710.4103/2156-7514.8517522059149 [Google Scholar] [CrossRef] [PubMed]