In various industrial workplaces, workers are exposed to different occupational and environmental risk factors such as heat stress, vibration, radiation and noise, that may threaten human health, productivity and performance [1]. Among these, noise is considered as one of the most influential and harmful physical agents at workplaces and it is categorised as an environmental risk factor [2,3]. Due to the rapid development of industries, it has become one of the threatening factors for physical and psychological health of individuals [4,5].
Many workers are employed in textile industry and this industry is among the most important industries of any country [6,7]. In textile industries, noise is caused by high speed rotation of various components of weaving machines. The produced noise is one of the main challenges for employees of this industry [8-10]. In these industries, workers are exposed to high level noise (about 95 dBA) in the weaving room [6,7]. The results of a study by Talukdar MK et al., indicated that the noise level in textile industry varies between 80 dBA to 99 dBA with the lowest and highest levels belonging to the blow room and loom shed respectively [10].
Research has shown that noise is associated with hearing loss, and in addition to the auditory effects, many other adverse effects such as stress, annoyance, sleepiness, hypertension, reduced cognitive performance and cardiovascular disease are also attributed to noise exposure [3,5,11-13]. Sleep disturbance is one of the most important adverse effect of noise exposure which has attracted the attention of many researchers [14-16].
Noise can affect the quality and quantity of sleep, subsequently adversely affecting performance, capacity and health. The effect of noise on sleep, based on the type of exposure is divided into two categories: acute and chronic sleep disturbance [17,18]. Acute sleep disorders can occur immediately or shortly after exposure to noise, whereas chronic sleep disorders arise from noise exposure for a long period of time. Decreased sleep duration, delay in falling asleep, early morning awakening, increased awakening during sleep and changes in sleep phases are the most important symptoms of sleep disturbance [18]. Sleep deprivation can cause decreased function of the immune system, hypothalamus, pituitary and adrenal glands. Sleep disturbance may also cause high blood pressure and reduce an individual’s talent and ability to work [19].
Textile industry involves a large number of workers who are subjected to high level of occupational noise that may affect their sleep. Thus, this study was conducted to investigate the effects of occupational noise exposure on sleep disturbance among the workers of textile industry.
Materials and Methods
This present cross-sectional study was conducted from October to December 2016, involving the employees of textile industry located in the Savadkuh city, Iran. The study population was selected through census, this means that the entire volunteer staff took part in the study. Due to the voluntary participation of people, the consent was not necessary. The study population consisted of total 60 volunteers involving weavers, repairmen and officials of the textile industry. In this study, ESS [20] and an author developed sociodemographic questionnaire (consisting of demographic information such as age, experience, etc.) were used to collect sleep disturbance and sociodemographic data respectively. Eight-hour equivalent noise level was measured to assess worker’s noise exposure. Ethical consideration such as keeping the personal information confidential was considered by authors. Inclusion criteria: staff exposed to noise above 80 dBA, with at least one year of work experience and no history of sedative drug use for at least one year. Exclusion criteria: staff with history of drug addiction and invalid questionnaires were excluded from the study.
Epworth Sleepiness Scale
Data regarding sleep disturbance was collected with the help of ESS [20]. The sleepiness of the workers was measured in eight different situations with the help of eight questions having response in Likert scale (0=lack of sleepiness and 3=excessive sleepiness). The scores ranged from 0 to 24. Individual score range from 0 to 8 was regarded as normal, 9 to 12 as mild, 13 to 16 as moderate and more than 16 as severe sleepiness [21].
Noise Measurement
Noise measurement was performed according to standard ISO 9612:2009 [22]. The level of worker’s noise exposure, was determined for all the work stations during all the shifts. The 15-minute equivalent noise level was measured using the dosimeter model SET-1355. In the end, eight-hour equivalent sound level was calculated using the formula [22]:
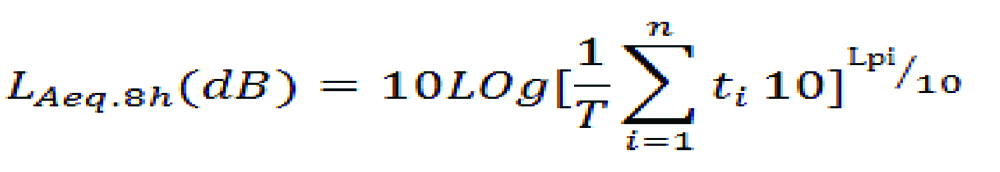
In this formula:
LAeq.8h=8-hour equivalent sound level,
ti=time within which the LAeq.ti levels occur,
T=sum of all ti,
Lpi=noise pressure level which is measured during ti
n=number of intervals in which the sound is measured.
Statistical Analysis
The data were entered into the SPSS Version 20.0 software and statistical analysis was performed. The Shapiro-Wilk test was applied for assessing normality. According to the results of Shapiro-Wilk test, data had non normal distribution. Thus, non parametric Mann-Whitney test and Kruskal-Wallis test were applied to study the mean sleep disturbance differences between the variables with two levels and three levels, respectively. To study the effect of noise exposure, age and duration of work experience linear regression test was applied. The spontaneous effects of understudied variables on sleep disturbances were assessed using stepwise multiple regression test.
Results
A total of 60 workers (45 males, 15 females) were investigated. The mean±standard deviation score for sleep disturbance was 12±4.1. Equivalent sound level was measured to be 94±4.1 dB. The mean±standard deviation for age and experience was 35±7.6 years and 10±6.2 years, respectively. The level of sound exposure for weavers, other repairmen and officials, single, married, workers who use HPDs, workers without HPDs, workers with sedative drug use, workers without sedative drug use was 94.1±5.2 dB, 93.9±3.8 dB, 95.9±2.4 dB, 94±4.1 dB, 95±3.3 dB, 91.7±4.7 dB, 95±3.3 dB and 91.7±4.7 dB, respectively.
Sleep disturbance in the workers without HPDs, workers with history of sedative drug use, workers working in the morning shift, workers with education level less than diploma and single workers was more than others. The results were statistically insignificant for workers of morning shift and education less than diploma.
The results of Kruskal-Wallis test showed that there was a statistically significant difference of mean sleep disturbance among age and work experience groups. There was no significant difference among other variables. The results of Kruskal-Wallis test is presented in [Table/Fig-1].
Comparison of mean value of sleep disturbance among classified variables such as age, experience, type of shift work and educational level.
| Variables | Frequency | Sleep disturbance mean (Standard deviation) | T | Significant with Kruskal-Wallis test |
|---|
| Age (year) | 20-30 | 21 (35%) | 7.6 (3.6) | 41.119 | < 0.001 |
| 30-40 | 22 (36.6%) | 13.3 (1.7) |
| 40-60 | 17 (28.4%) | 15.6 (1) |
| Shifts | Morning | 32 (53.3%) | 12.5 (3.3) | 3.132 | 0.209 |
| Evening | 15 (25%) | 10.8 (4.5) |
| Night | 12 (20%) | 10.8 (5.2) |
| Level of education | < Diploma | 12 (20%) | 13.3 (3.2) | 1.447 | 0.485 |
| Diploma | 36 (60%) | 11.4 (4.4) |
| > Diploma | 12 (20%) | 12.4 (4) |
| Work experience (year) | <5 year | 21 (35%) | 8.1 (3.6) | 31.458 | < 0.001 |
| 5-15 | 22 (36.6%) | 13.0 (3.1) |
| 15-25 | 17 (28.4%) | 15.4 (1.4) |
The results of Mann-Whitney test showed that the mean sleep disturbance was significantly different among workers with history of sedative drug use, non usage of HPDs and marital status (p-value <0.001). The results are shown in [Table/Fig-2].
Comparison of mean value of sleep disturbance among understudy variables such as history of sedative drug use, HPDs, marital status and type of job.
| Variables | Frequency | Sleep disturbance mean (Standard deviation) | T | Significant with Mann-Whitney test |
|---|
| History of sedative drug use | Yes | 40 (66.7%) | 14.2 (3.2) | 85 | < 0.001 |
| No | 20 (33.3%) | 10.9 (4.1) |
| Hearing protection devices (HPDs) | Yes | 40 (66.7%) | 10.0 (4) | 131.5 | < 0.001 |
| No | 20 (33.3%) | 14.8 (2.5) |
| Marital status | Married | 15 (25%) | 6.8 (3.3) | 52.5 | < 0.001 |
| Single | 45 (75%) | 13.7 (3.7) |
| Job | Weaver | 48 (80%) | 11.8 (4.3) | 253.5 | 0.521 |
| Other | 12 (20%) | 12.7 (3.4) |
Simple linear regression test was used to study the effects of noise induced from weaving machines, age and job tenure on sleep disturbance. Based on the results of this test it was observed that noise exposure could justify 18% of the dependent variables. The results also showed that each 1 dB increase of noise exposure is accompanied by 0.43 unit increase in sleep disturbance.
The results also showed that age and duration of work experience had a significant effect on sleep disturbance so that they could justify 73% and 47% of sleep changes, respectively. Based on the results of this simple linear regression test, each one year increase in age and duration of work experience is accompanied by 0.86 and 0.68 unit increase of sleep disturbance, respectively.
To study the spontaneous effects of independent variables on sleep disturbances, stepwise multiple regression test was used. Stepwise multiple regression results showed that during the five steps, by adding a new variable to the previous steps, five variables, including age, noise exposure, marital status, HPDs and history of sedative drug use could predict sleep disturbance significantly. The results of stepwise multiple regression test are presented in [Table/Fig-3].
Simultaneous effects of age, noise exposure, marital status, HPDs and history of sedative drug use on the sleep disturbance.
| Predictor variables | Beta | B | Standard error | T | p-value |
|---|
| Age | 0.691 | 0.37 | 0.041 | 9.06 | 0.001 |
| Noise exposure | 0.44 | 2.5 | 0.45 | 5.54 | 0.001 |
| Marital status | 0.335 | 3.16 | 0.59 | 5.32 | 0.001 |
| Hearing protection devices (HPDs) | 0.222 | 1.92 | 0.51 | 3.74 | 0.001 |
| History of sedative drug use | 0.195 | 1.93 | 0.68 | 2.83 | 0.006 |
In the first step, based on the results of Kruskal-Wallis test and regression statistical indices it was clear that age could justify dependent variable changes statistically, so that it was able to predict 72% of changes in sleep. In the second step, age and noise exposure were included in the model and they could simultaneously predict 81% of changes in sleep. In the next step, age, noise exposure and marital status were simultaneously entered into the model and they could predict 83% of changes in sleep. In the fourth step, the three above mentioned variables along with HPDs were included in the model simultaneously and they could predict a total of 85% of the sleep disturbance. In the final step, history of sedative drug use was added to the model and it was observed that predictors could justify 87% of sleep disturbance. The results of stepwise multiple regression test are presented in [Table/Fig-3].
Discussion
The results of the present study, showed that occupational noise is one of the important factors that can affect sleep. The literature had confirmed that noise exposure can cause indirect effects in addition to the hearing damage. Amongst these indirect effects, decreased general health and sleep disturbance are some of the most important effects that have caused a number of complaints from individuals who are exposed to noise [4,5,18]. Textile industry, due to the interactions of various rotating components of spinning and weaving machines produces high level of sound that exceeds the standard level. This study was conducted to investigate the effects of occupational noise exposure on sleep among the workers of textile industry.
The results of the present study showed that there was a significant relationship between sleep disturbance and age, which is consistent with other studies [16,23]. Abbasi M et al., showed that age can directly affect sleep and sleep disturbance is higher in the elderly compared to young [16]. Circadian rhythm is affected by age and it is reasonable to expect that advancing age disturbs sleep. Based on the results of Kruskal-Wallis test, mean sleep disturbance was different among workers with different work experience. It can be said that workers with higher work experience are more exposed to occupational risk factors such as noise, which can affect their sleep and thus their sleep is more disturbed.
In the present study a significant relationship between marital status and sleep disturbance was also revealed. These results are contrary to the results of the study by Lallukka T et al., [24]. They showed that married individuals with high and low income had more sleep disturbances compared to the single individuals. Nuaim R et al., conducted a study on the aluminium industry workers in 2015 and showed that there was a significant relationship between sleep disturbance and marital status [25]. Knudsen HK et al., showed marital status as the measure of trouble falling asleep [26].
The results of the present study revealed that there was a significant association between history of sedative drug use and sleep disturbance. Izadi F et al., said that there is a significant relationship between sleep quality and use of hypnotics [27]. Frighetto L et al., stated that people who use hypnotic drugs were not satisfied with their sleep [28]. An association of HPDs with sleep disturbance was observed in this study [Table/Fig-2]. Considering the results of this study that noise can affect worker’s sleep, it can be said that workers who don’t use HPDs are exposed to lower levels of occupational noise but they perceive higher level of noise and subsequently they experience more sleep disturbance. HPDs as a control device can reduce the level of individual’s noise exposure to about 15 dB. Workers with HPDs were exposed to 95±3.3 dB noise; however, HPDs can reduce their exposure to 80 dB and it can be assumed that although this group is exposed to higher level of noise but they perceive lower level of noise compared to workers without HPDs.
The present study investigated the effects of occupational noise exposure on sleep among the workers. The results of the study showed that there was an impact of occupational noise exposure on workers’ sleep. This result is confirmed by other researchers [15,16,18]. Abbasi M et al., reported that wind turbine noise had a potential effect on the sleep of wind farm workers. They also stated that sleep disturbance can be caused by noise annoyance and subsequently it can cause adverse health effects [29]. Sunde E et al., noted that equivalent noise level and the sleep variables such as time in bed, sleep interval duration, average duration of awakenings, percentage mobility and sleep efficiency have a statistically significant association [30].
Limitation
This study had some limitations. The study design was cross-sectional and sleep disturbance was assessed by a subjective method. Subjective methods are intrinsically prone to bias.
Conclusion
As per the findings of the present study it may be concluded that age, duration of work experience, sedative drug use, non usage of HPDs and marital status may be responsible for sleep disturbance; however, occupational noise exposure should also be regarded as a factor that may cause sleep disturbance among the workers of textile industry. Thus, noise control methods should be employed as an essential strategy for reducing sleep disturbance.