Paraurethral Leiomyoma in a Young Female: A Case Report
Rohan Surendrakumar Batra1, Jaynil A Bagawade2, Phanindra Mohan Deka3
1 Resident, Department of Urology, Dispur Hospitals Pvt. Ltd., Guwahati, Assam, India.
2 Resident, Department of Urology, Dispur Hospitals Pvt. Ltd., Guwahati, Assam, India.
3 Professor, Chief Consultant Urologist and Head, Department of Urology, Dispur Hospitals Pvt. Ltd., Guwahati, Assam, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Phanindra Mohan Deka, Professor, Chief Consultant Urologist and Head, Department of Urology, Dispur Hospitals Pvt. Ltd., Ganeshguri, Guwahati-781006, Assam, India.
E-mail: pmdeka@yahoo.com
Leiomyomas are benign tumours which originate in the smooth muscle rest cells. The origin of the tumour in the paraurethral region is rare. Herein, we describe a case of a 30-year-old female patient with a mass at the paraurethral region which turned out to be leiomyoma. Paraurethral leiomyoma make up only approximately 5% of urethral tumours. This case depicts the presentation and subsequent management of the patient with paraurethral leiomyoma.
Benign, Dyspareunia, Tumour
Case Report
A 30-year-old female presented with complains of a swelling in the right periurethral region, slightly proximal to the urethral meatus since one year. She took treatment at a local hospital but the swelling gradually increased in size and she started experiencing discomfort because of the swelling. She also had dyspareunia which she thought attributed to the swelling. Otherwise, the swelling was painless. She had no history of urinary complaints like dysuria, hesitancy, decreased flow or retention. The patient was married since five years and had a 3-year-old healthy child. The patient had normal menses every month. She had no history of any discharge or bleeding from the mass.
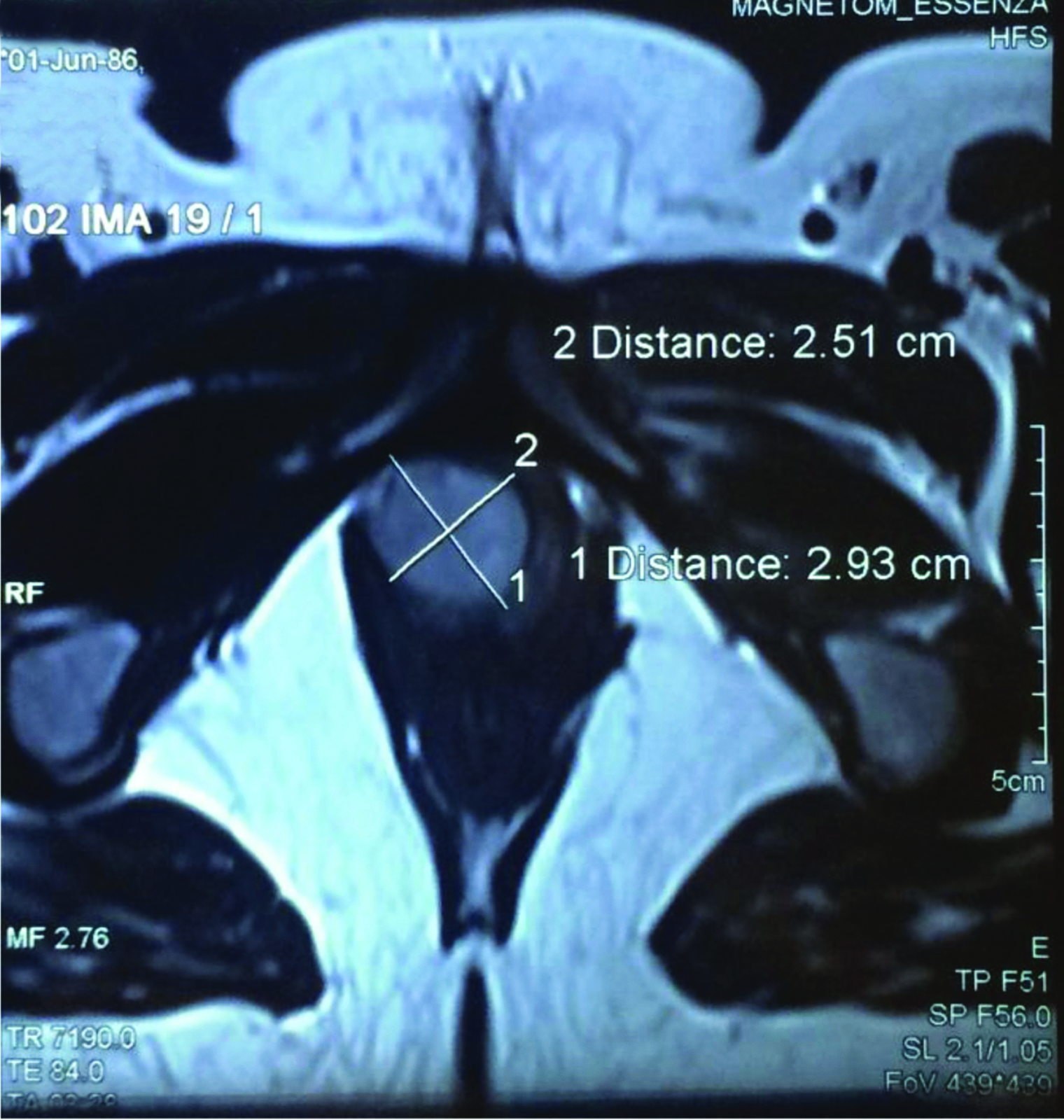
Examination of the patient revealed a 4×4 cm swelling in the right paraurethral region which was ovoid in shape, non tender, non fluctuant with no signs of inflammation [Table/Fig-1]. The routine blood reports conducted were all within the normal limits. An Megnetic Resonance Imaging (MRI) showed a well defined oval altered intensity lesion of size 26×24×20 mm in relation to the distal anterior wall of vagina predominantly on the right side compressing the distal urethra anteriorly [Table/Fig-2]. It showed heterogeneous post contrast enhancement representing a soft tissue mass. She was planned for urethrocystoscopy and mass excision. Urethrocystoscopy revealed no communication between the mass and the urethra.
Swelling in right paraurethral region with a urethral dilator in the urethra.

MRI showing well defined oval altered intensity lesion of size 26×24×20 mm.
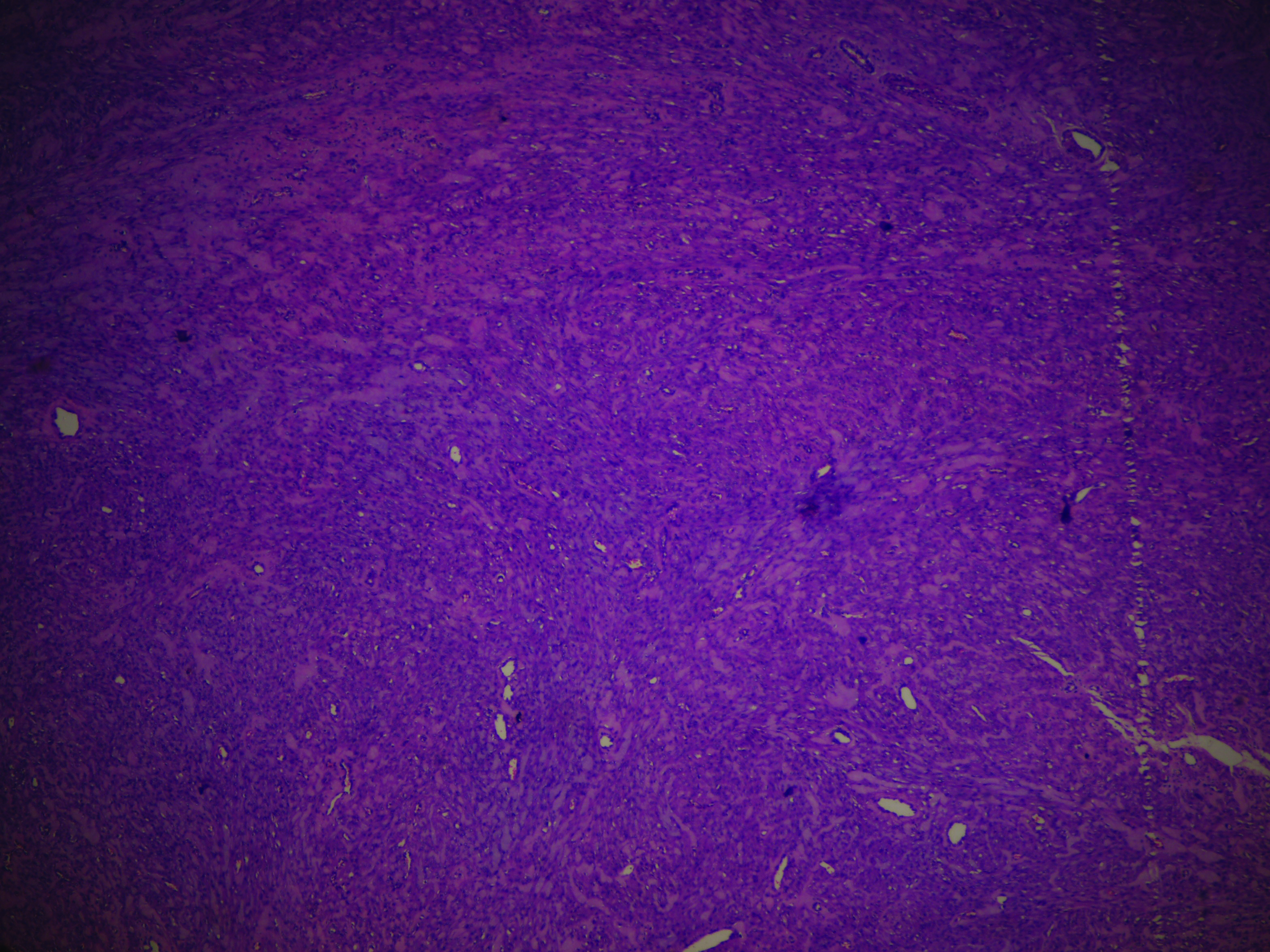
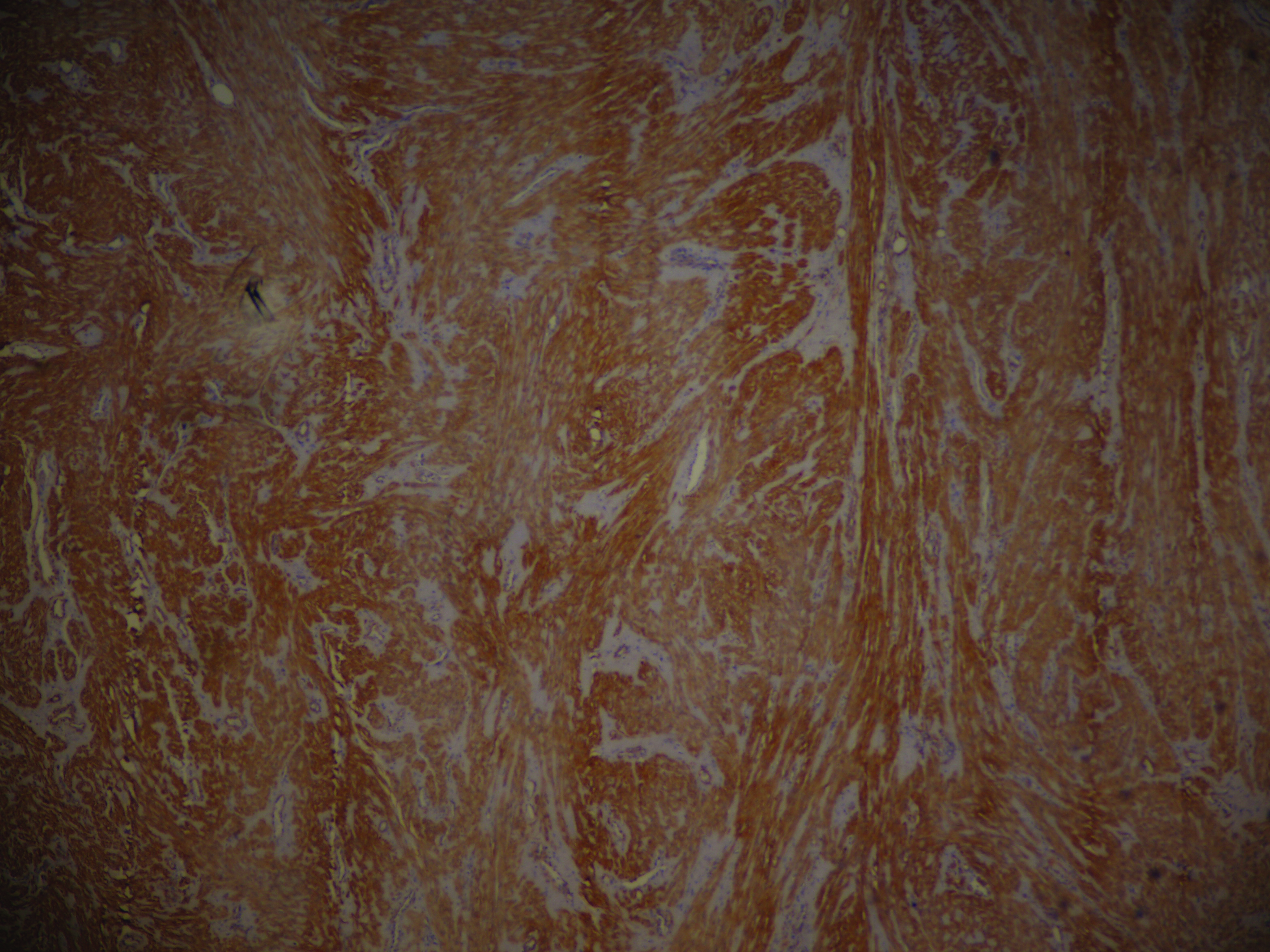
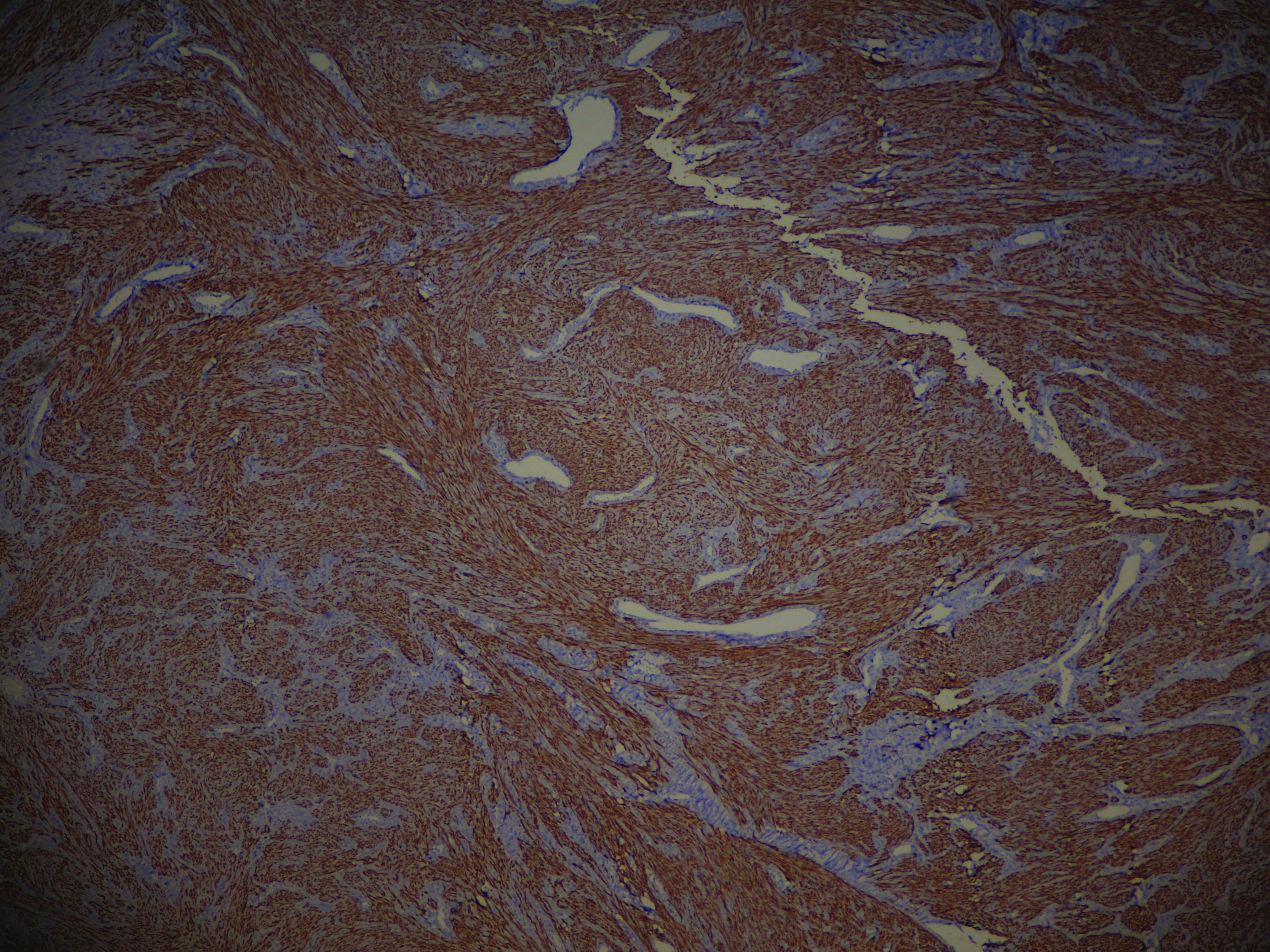
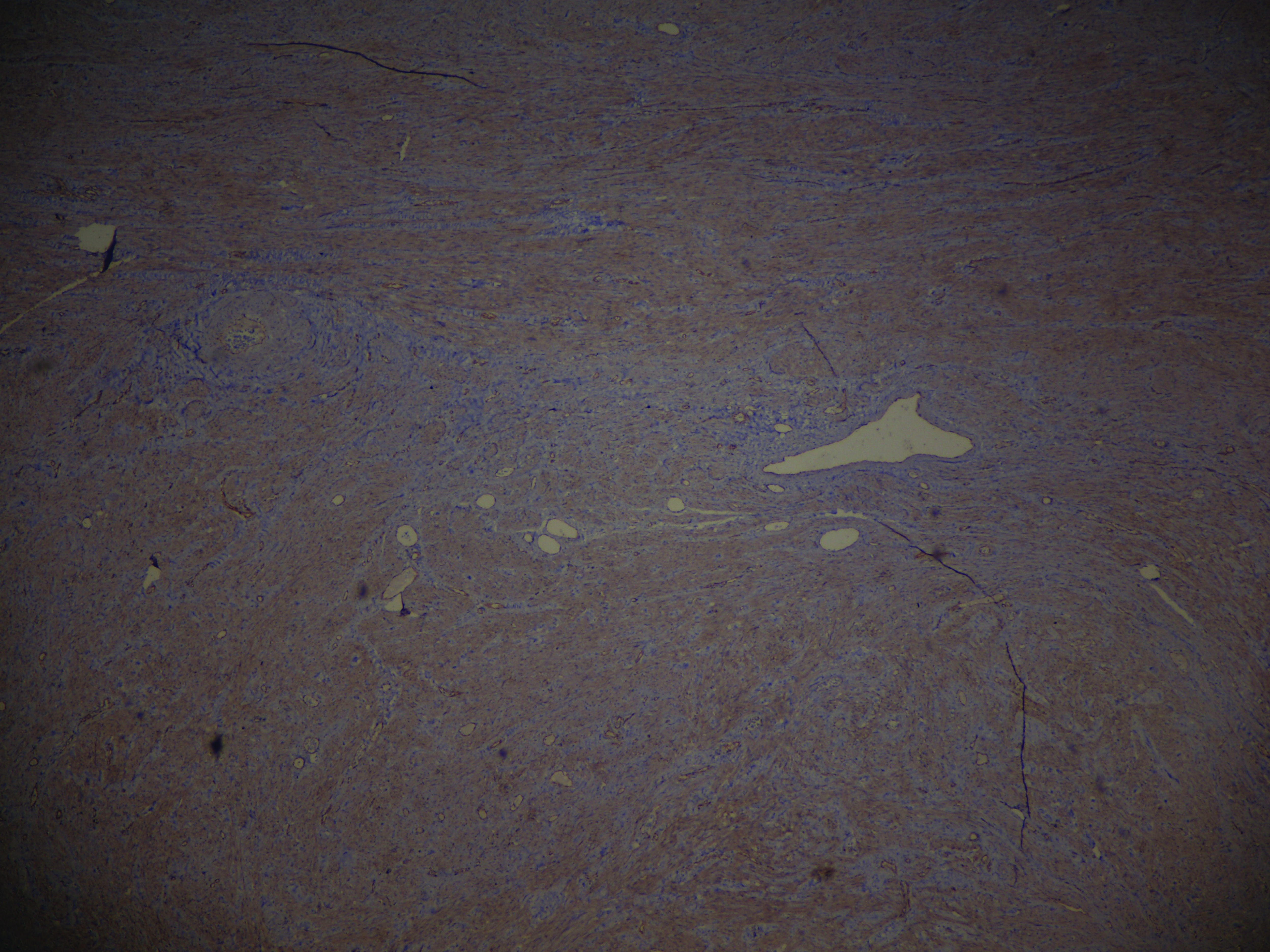
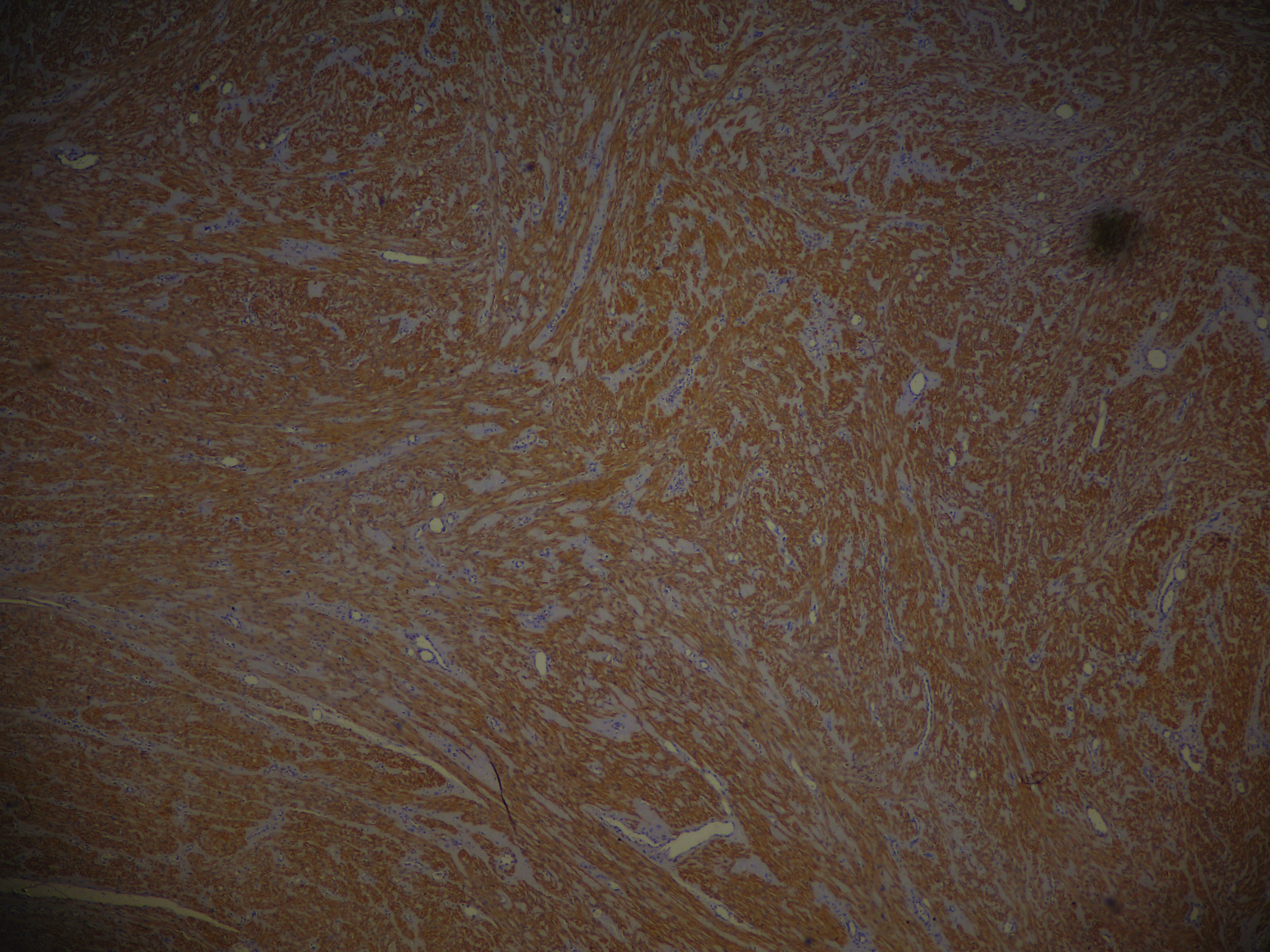
The mass was excised under general anaesthesia. Urethra was identified and the mass was excised using a diamond shape incision [Table/Fig-3]. After achieving complete haemostasis, the walls of the cavity were closed with a double layer of 4-0 vicryl. The foley’s catheter was kept indwelling for one day post surgery. The mass was sent for histopathology which revealed spindle and plump cells in a collagenous stroma [Table/Fig-4]. Due to rarity of such a lesion in the paraurethral region, Immunohistochemistry (IHC) was performed which revealed Smooth Muscle Actin (SMA) ] and desmin diffusely positive, beta catenin negative and calponin strongly positive suggestive of a leiomyoma [Table/Fig-5,6,7 and 8]. The patient was asymptomatic and returned to normal activity without any restrictions within four weeks of surgery.
Gross specimen of mass after excision.

Spindle and plump cells in a collagenous stroma (H&E, 40X).
SMA diffusely positive (IHC, 40X).
Desmin diffusely positive (IHC, 40X).
Beta catenin negative (IHC, 40X).
Calponin strongly positive (IHC, 40X).
Discussion
Leiomyomas are benign tumours which originate in the smooth muscle rest cells. Paraurethral leiomyoma is a rare cause of periurethral mass and it is believed to develop from the smooth muscle fibres of the lower urinary tract [1]. The exact aetiology of bladder, urethral and paraurethral leiomyoma is unknown. However, they are relatively more found in the reproductive age women (compared to younger and older women or men) and it has led to the speculation that leiomyoma growth is enhanced by circulating female hormones [2]. Paraurethral tumours occur in the paraurethral space or vesicovaginal septum and are mostly asymptomatic but are sometimes associated with pain, dyspareunia and voiding problems [3]. Paraurethral tumours can clinically present as urethral and vaginal-wall leiomyoma because they grow in spaces that have no communication with the urethra, bladder or vagina [4,5]. They have to be differentiated from urethral diverticulae, urethral mucosal prolapsed, skene duct cyst, gartner cyst, urethral carcinoma and vaginal mass.
Paraurethral leiomyomas usually present in the reproductive age group from 30-50 years [6]. Most of the patients are asymptomatic and present as a painless mass at the external genitalia. They may complain of dyspareunia or urinary complains like decreased flow, dysuria and rarely, retention of urine. Very rarely, bleeding from leiomyoma may occur [7]. The physical examination usually reveals a firm, non fluctuant mass at the paraurethral region. It may be difficult to differentiate between urethral, vaginal and paraurethral leiomyomas during the physical examination alone.
Imaging modalities for these masses include MRI which typically provide typically rounded, well-circumscribed, whorl-appearing masses of low T1-signal intensity with homogeneous enhancement after gadolinium administration [7,8]. T2-weighted images show masses with low to intermediate signal intensity, which is typical of smooth muscle tumours located elsewhere in the body. Any communication with the urethra can be delineated in the MRI. Cystourethroscopy is essential to rule out any urethral diverticulum and any communication between the mass and urethra. Migliari R et al., reported six cases of female paraurethral leiomyomas and suggested pelvic MRI as a primary examination, followed by lesion biopsy [9]. According to Navarro PH et al., paraurethral leiomyoma present as benign neoplasms of mesenchymal origin contained in a fibrous capsule not adherent to adjacent structures [10]. Surgical excision is the mainstay of treatment. In some cases, stress urinary incontinence may develop after surgery. If the mass is small, then conservative approach can be tried in medically unfit patients. No recurrences have been reported till date.
Conclusion
Paraurethral leiomyoma is a rare benign tumour found in the paraurethral region and requires a high degree of suspicion for diagnosis. A sound knowledge of female urethral and vaginal anatomy is required to treat and completely excise the tumour.
[1]. Adams-Piper E, Jacobs S, Ghoniem GM, Paraurethral leiomyoma in a 20 year-old woman: a case reportUrol Case Rep 2016 4:14-16.10.1016/j.eucr.2015.10.00826793567 [Google Scholar] [CrossRef] [PubMed]
[2]. Özel B, Ballard C, Urethral and paraurethral leiomyomas in the female patientInt Urogynecol J 2005 17(1):93-95.10.1007/s00192-005-1316-315905997 [Google Scholar] [CrossRef] [PubMed]
[3]. Hubert KC, Remer EM, Rackley RR, Goldman HB, Clinical and magnetic resonance imaging characteristics of vaginal and paraurethral leiomyomas: can they be diagnosed before surgery?BJU Int 2010 105(12):1686-88.10.1111/j.1464-410X.2009.09046.x19889060 [Google Scholar] [CrossRef] [PubMed]
[4]. Selli C, Dal Canto M, Campani D, Bartoletti R, De Benedetto A, Leiomyoma of the female urethraUrol Int 1995 54(3):179-80.10.1159/0002827197604466 [Google Scholar] [CrossRef] [PubMed]
[5]. Cheng C, Mac-Moune Lai F, Chan PS, Leiomyoma of the female urethra: a case report and reviewJ Urol 1992 148(5):1526-27.10.1016/S0022-5347(17)36957-4 [Google Scholar] [CrossRef]
[6]. Bennett GH, Erlich MM, Myoma of the vaginaAm J Obstet Gynecol 1941 42:314-20.10.1016/S0002-9378(16)40639-3 [Google Scholar] [CrossRef]
[7]. Shadbolt CL, Coakley FV, Qayyum A, Donat SM, MRI of vaginal leiomyomasJ Comput Assist Tomogr 2001 25:355-57.10.1097/00004728-200105000-0000511351183 [Google Scholar] [CrossRef] [PubMed]
[8]. Pavlica P, Bartolone A, Gaudiano C, Barozzi L, Female paraurethral leiomyoma: ultrasonographic and magnetic resonance imaging findingsActa Radiol 2004 45(7):796-98.10.1080/0284185041000137615624526 [Google Scholar] [CrossRef] [PubMed]
[9]. Migliari R, Buffardi A, Mosso L, Female paraurethral leiomyoma: treatment and long-term follow-upInt Urogynecol J 2015 26(12):1821-25.10.1007/s00192-015-2776-826224380 [Google Scholar] [CrossRef] [PubMed]
[10]. Navarro PH, Ruiz MJ, Sanchíz MC, Teruel PM, Martín SM, Pastor-Guzma JM, Paraurethral leiomyomaArch Esp Urol 2013 66(8):820-23. [Google Scholar]