Spinal anaesthesia is a commonly used regional anaesthesia technique for lower limb and lower abdominal surgeries owing to its well-known advantages like quick onset, excellent sensory and motor block and avoidance of complications of general anaesthesia [1]. The widely used local anaesthetic in spinal anaesthesia is bupivacaine 0.5% heavy which is available in a commercial preparation as a racemic mixture (50:50) of its two enantiomers, levobupivacaine, S (−) isomer and dextrobupivacaine, R (+) isomer [2,3]. Severe Central Nervous System (CNS) and cardiovascular adverse reactions reported in the literature after inadvertent intravascular injection or intravenous regional anesthesia have been linked to the R (+) isomer of bupivacaine [3]. In the last few years, its pure S-enantiomer levobupivacaine, has been introduced into clinical practice because of its lower toxic effects on heart and CNS [4-6]. Bupivacaine and levobupivacaine both have been evaluated in many studies and have been found to have almost similar anaesthesia profile [2], [7-15]. However, in some of the studies, the onset, intensity and duration of motor block with levobupivacaine has been found to be different from bupivacaine [16-23]. Since there aren’t enough studies on comparison of intrathecal bupivacaine and levobupivacaine in lower abdominal surgeries, the aim of the present study was to compare the safety and efficacy of isobaric bupivacaine 15 mg and isobaric levobupivacaine 15 mg in patients undergoing lower abdominal surgery under spinal anaesthesia.
Materials and Methods
The present study was a prospective, randomised, double blind clinical study which was carried out for a duration of 10 months from January 2014 to October 2014 after seeking approval from the Scientific and Ethical Research Committee of Government Medical College and S.S.G Hospital, Vadodara, Gujarat, India. The procedures followed were in accordance with the ethical standards of the Helsinki Declaration of 1975 that was revised in 2000. Written and informed consent was obtained from the patients.
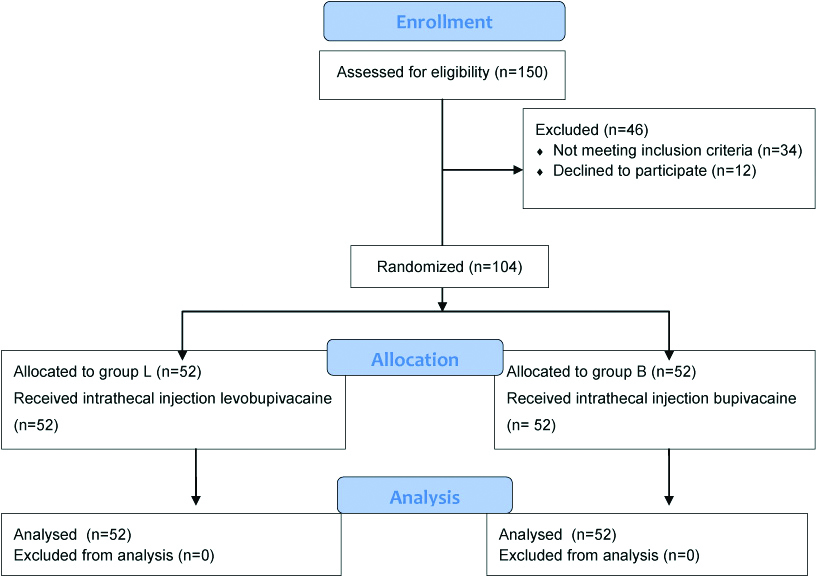
Sample size estimation was done using Epi Info version 7.0. We used hypotension (systolic blood pressure <20% of baseline) as the primary outcome. We undertook a pilot case study of 30 cases (15 cases in each group) to determine the difference of primary outcome between the two study groups. In the levobupivacaine group, 1 out of 15 patients (6.7%) developed hypotension and in the bupivacaine group, 4 out of 15 patients (26.7%) developed hypotension. Thus, percentage of outcome in levobupivacaine group was taken as 6% and that in bupivacaine group was taken as 26%. With two sided confidence level of 95% and power of 80%, minimum adequate sample size came out to be 52 patients in each group. A total of one hundred and fifty patients were assessed for eligibility [Table/Fig-1]. Patients in the age group of 18-60 years, ASA Grade I or II, average body weight, those undergoing planned lower abdominal surgery-inguinal hernia or hydrocele were enrolled for the study and thorough preoperative checkup was done. Patients who had contraindications to spinal anaesthesia, allergy to amide local anaesthetics, a significant history of drug or alcohol abuse, morbid obesity, diabetic, neurological and musculoskeletal diseases and those who refused to participate in the study were excluded from the study. All the selected patients were explained in detail about the purpose, procedure of the study and possible side effects. Patients were randomly allocated to two groups of 52 patients each using online tool Research Randomizer (www.randomizer.org).
Patients in Group L received injection levobupivacaine 15 mg (3 mL isobaric 0.5%) and patients in Group B received injection bupivacaine 15 mg (3 mL isobaric 0.5%). Drug to be injected according to the group was prepared in an adjacent room by a supervisor not involved in the subsequent evaluation of the study patient. Following arrival in the anaesthetic room, IV access was established and an infusion of 500 mL Ringer’s lactate commenced. Patients were premedicated with 1 mg of midazolam intravenously and placed in left lateral position. Under all aseptic and antiseptic precautions and after skin infiltration with 2% lidocaine, a 23G spinal needle was inserted at the L3/4 interspace in the midline. Correct needle placement was identified by free flow of cerebrospinal fluid and then 3 mL (15 mg) of the study drug was injected over 10 seconds. After the injection of the drug the spinal needle was removed and the patient placed supine.
Standard monitoring was used throughout the operation. Electrocardiogram (ECG) and oxygen saturation (SpO2) were monitored continuously. Heart rate, arterial pressure and respiratory rate were recorded before giving the block and then at 1, 3, 5, 10 and 15 minutes after giving spinal anaesthesia, After that, every 15 minutes till the end of surgery and then immediately after surgery, 30 minutes, 1 hour, 2 hours and 4 hours postoperatively was recorded. Any incidence of hypotension (blood pressure <20% of baseline) or bradycardia (heart rate <20% of baseline) were treated with intravenous ephedrine 5 mg or atropine 0.5 mg increments respectively. A decrease in SpO2 to <95% was defined as hypoxia and treated with supplemental oxygen.
The level of sensory block was evaluated by loss of pinprick sensation (20G hypodermic needle) which was checked every 30 seconds till the onset of sensory block, then every minute for the next 10 minutes, and then every 10 minutes until its full recovery. We checked bilaterally L1, T12, T10, T8, T6 or higher (T4) dermatomes and we used C5-6 as a baseline point for normal sensation. Motor block was assessed using modified Bromage scale [24] (Grade 0-no weakness-full power, Grade 1-Can flex knees but cannot raise legs, Grade 2-Only foot movements, Grade 3-complete paralysis). The maximum Bromage score reached and duration of motor block (from spinal injection until Bromage 0 score) were recorded every five minutes after drug’s injection until full recovery.
The onset of sensory or motor blockade was defined as interval between intrathecal administration and loss of pinprick sensation at L1 level, or a Bromage score of 1, respectively. Sensory block parameters like onset of sensory block at L1 level, peak sensory level achieved, time to attain peak sensory level, two segment regression time from peak sensory level and time for regression back to L1 level from highest sensory level were recorded. Motor block parameters like onset of motor block, maximum motor block achieved, time to attain maximum motor block and duration of motor block were recorded. Duration of surgery and anaesthesia, duration of effective analgesia and intraoperative and postoperative complications like hypotension, bradycardia, respiratory depression, nausea/vomiting, cardiac arrhythmias, rigors, post-dural puncture headache, backache, urinary retention and neurological complications were recorded.
Statistical Analysis
All statistical analyses were performed using MedCalc statistical software. Quantitative data were presented as mean and standard deviation (mean±sd). Intergroup data were analysed by unpaired t-test. Significance was judged as follows: p>0.05 not significant, p<0.05 significant and p<0.001 highly significant.
Results
The two groups were comparable to each other with respect to demographic data parameters and duration of surgery [Table/Fig-2]. Type of surgeries were also comparable; 30 patients in Group L and 34 patients in Group B underwent inguinal hernioplasty (p=0.42) and 22 patients in Group L and 18 patients in Group B underwent hydrocele excision (p=0.42).
Demographic data and duration of surgery.
| Parameter | Group L(n=52) | Group B(n=52) | p-value |
|---|
| Age in years (mean±SD) | 44.04±12.36 | 45.5±13.38 | 0.56 |
| Weight in kg (mean±SD) | 61.13±5.34 | 60.04±5.47 | 0.30 |
| Sex (male:female) | 50:2 | 50:2 | - |
| ASA grading (I:II) | 30:22 | 27:25 | 0.89 |
| Mean duration of surgery (minutes) | 86.83±17.01 | 80.96±10.34 | 0.08 |
p-value calculated using unpaired t-test
[Table/Fig-3] compares the characteristics of sensory and motor block between the two groups. As it can be seen, there was no statistically significant difference between the two groups in terms of sensory block characteristics. Both groups were also comparable in motor block characteristics, except time to attain maximum Bromage grade (Grade 3) which was faster for Group B compared to Group L, the difference being highly statistically significant (p<0.0001).
Sensory and motor block characteristics.
| Parameter | Group L (n=52) | Group B (n=52) | p-value |
|---|
| Sensory block |
| 1 | Onset of sensory block at L1 (minutes) | 1.58±0.21 | 1.59±0.21 | 0.80 |
| 2 | Peak sensory level achieved | T6:T8:T1013:37:2 | T6:T8:T106:42:4 | |
| 3 | Time to attain peak sensory level (minutes) | 5.63±1.39 | 5.38±0.94 | 0.28 |
| 4 | Two segment regression time (minutes) | 73.63±12.37 | 72.98±5.53 | 0.73 |
| 5 | Time for regression up to L1 (minutes) | 146.17±21.44 | 151.44±14.08 | 0.14 |
| Motor block |
| 1 | Onset of motor block (minutes) | 3.39±0.75 | 3.30±0.68 | 0.52 |
| 2 | Maximum Bromage grade achieved (II:III) | 0:30 | 0:30 | |
| 3 | Time to attain maximum Bromage grade (minutes) | 10.06±1.38 | 8.03±1.91 | <0.0001 |
| 4 | Duration of motor block (minutes) | 252.31±18.98 | 255.28±9.85 | 0.31 |
p-value calculated using unpaired t-test
The mean preoperative vital parameters were comparable between the two groups [Table/Fig-4]. [Table/Fig-4] also shows changes in mean pulse rate, systolic and diastolic BP intraoperatively following spinal anaesthesia and postoperatively which were comparable among both groups. There was no statistically significant change in ECG, mean arterial oxygen saturation and mean respiratory rate intraoperatively as well as postoperatively in both the groups.
Changes in mean pulse rate, systolic and diastolic blood pressure.
| Time | Pulse rate (per minute) | Systolic BP (mmHg) | Diastolic BP (mmHg) |
|---|
| Group L (n=52) | Group B (n=52) | p-value | Group L (n=52) | Group B (n=52) | p-value | Group L (n=52) | Group B (n=52) | p-value |
|---|
| Pre-operative | 78.69±9.97 | 82.15±10.61 | 0.08 | 128.08±10.51 | 126.62±12.11 | 0.51 | 81.38±8.23 | 80.31±7.91 | 0.50 |
| Post intrathecal injection |
| 1 minute | 77.92±10.11 | 81.69±10.60 | 0.06 | 125.38±10.72 | 122.38±9.93 | 0.14 | 80.65±7.28 | 80.19±7.82 | 0.75 |
| 3 minutes | 77.90±9.74 | 81.92±10.93 | 0.05 | 122.92±11.81 | 119.53±10.58 | 0.12 | 79.54±7.79 | 79.04±7.43 | 0.73 |
| 5 minutes | 79.08±9.77 | 81.92±10.81 | 0.16 | 116.69±13.67 | 114.86±11.91 | 0.46 | 76.69±10.03 | 77.07±6.93 | 0.82 |
| 10 minutes | 78.77±9.99 | 81.54±11.45 | 0.19 | 116.26±12.02 | 115.30±11.57 | 0.67 | 76.92±9.41 | 77.04±6.51 | 0.93 |
| 15 minutes | 79.13±10.11 | 81.63±11.38 | 0.23 | 119.08±10.67 | 116.80±10.04 | 0.26 | 78.00±8.80 | 77.35±6.38 | 0.66 |
| 30 minutes | 78.73±10.58 | 82.04±11.42 | 0.12 | 119.96±10.72 | 117.92±9.08 | 0.29 | 78.34±8.04 | 77.31±6.67 | 0.47 |
| 45 minutes | 79.21±10.18 | 81.94±11.49 | 0.20 | 122.11±10.02 | 119.27±9.08 | 0.13 | 78.61±7.51 | 77.73±6.84 | 0.53 |
| 60 minutes | 78.13±10.03 | 81.69±10.88 | 0.08 | 122.5±10.45 | 120.27±10.27 | 0.27 | 78.61±8.31 | 77.61±6.59 | 0.49 |
| 75 minutes | 78.90±10.54 | 82.00±10.89 | 0.14 | 123.5±10.64 | 121.48±11.01 | 0.34 | 78.42±8.15 | 78.04±6.31 | 0.79 |
| 90 minutes | 78.92±9.80 | 82.34±10.60 | 0.09 | 124.96±10.63 | 121.31±11.08 | 0.08 | 77.43±8.29 | 77.89±6.76 | 0.75 |
| Postoperative |
| Immediate | 79.27±10.19 | 81.15±10.52 | 0.35 | 125.73±10.21 | 123.86±10.87 | 0.36 | 81.85±7.61 | 80.15±7.84 | 0.26 |
| 30 minutes | 78.46±9.87 | 81.96±10.35 | 0.08 | 125.19±10.53 | 123.77±11.09 | 0.50 | 82.19±8.11 | 80.35±8.12 | 0.25 |
| 1 hour | 79.02±10.22 | 81.96±10.56 | 0.15 | 125.65±12.19 | 123.96±10.48 | 0.45 | 81.96±7.71 | 80.11±8.23 | 0.23 |
| 2 hours | 78.65±10.19 | 82.38±10.45 | 0.06 | 125.80±11.71 | 124.15±10.79 | 0.45 | 82.62±7.05 | 80.27±7.98 | 0.11 |
| 4 hours | 78.77±10.19 | 82.86±10.37 | 0.05 | 126.5±11.36 | 124.58±10.42 | 0.37 | 82.04±7.87 | 80.42±8.14 | 0.30 |
Data are presented as mean±standard deviation p-value calculated using unpaired t-test
The duration of effective analgesia was 185.30±8.30 for Group L, while in Group B it was 188.00±7.22 minutes. The difference was not statistically significant (p=0.08). [Table/Fig-5] shows that there was no statistically significant difference in the incidence of intraoperative complications in both the groups. None of the patients in either group had any postoperative complication like bradycardia, hypotension, cardiac arrhythmias, respiratory depression, nausea/vomiting, urinary retention, post dural puncture headache or neurological problems.
Intra operative complications.
| Parameter | Group L (n=52) | Group B (n=52) | p-value |
|---|
| Number of patients | % | Number of patients | % |
|---|
| Bradycardia | 1 | 1.92% | 2 | 3.84% | 0.56 |
| Hypotension | 5 | 9.61% | 8 | 15.38% | 0.37 |
| Nausea/ vomiting | 3 | 5.77% | 2 | 3.84% | 0.64 |
p value calculated using unpaired t- test
Discussion
This study shows that intrathecal administration of 15 mg bupivacaine or 15 mg levobupivacaine was well tolerated and adequate block for lower abdominal surgery was achieved in all patients. Intergroup differences between levobupivacaine and bupivacaine were insignificant with regard to onset of sensory blockade, maximum cephalic spread, time to attain peak sensory level, two segment regression time, time for regression up to L1 level and duration of effective analgesia. The two groups were also comparable to each other with respect to onset of motor blockade, maximum Bromage grade achieved and duration of motor block. However, time to attain maximum Bromage grade was significantly faster in bupivacaine group compared to levobupivacaine group. These results were partially in agreement with those of other investigators. The majority of clinical studies that have compared levobupivacaine and bupivacaine have discovered fewer differences between them and have reported that both agents perform similarly [2], [7-15].
Glaser C et al., compared isobaric 3.5 mL solutions of 0.5% levobupivacaine and 0.5% bupivacaine in 80 patients undergoing hip replacement surgery under spinal anaesthesia. They found no significant difference between the two drugs and concluded that both drugs were equipotent and offered similar onset time, duration and haemodynamic effects [9]. Similar results were reported by Alley EA et al., who randomised 18 healthy volunteers into three equal groups to receive two spinal anaesthetic drugs, levobupivacaine and bupivacaine, of equal milligram doses and found that hyperbaric levobupivacaine has equivalent clinical efficacy to racemic bupivacaine for spinal anaesthesia in doses from 4-12 miligrams [10]. In the study of Fattorini E et al., 60 patients undergoing major orthopaedic procedures were divided into two groups; one group received 3 mL of 0.5% isobaric bupivacaine and the other received 3 mL of 0.5% isobaric levobupivacaine. There was no statistically significant difference in anaesthetic potencies between the two drugs [11]. Vanna O et al., compared 2.5 mL solution of 0.5% isobaric levobupivacaine with 2.5 mL solution of 0.5% hyperbaric bupivacaine in 70 patients undergoing elective transurethral endoscopic surgery and concluded that both these drugs showed equally effective potencies for spinal anaesthesia with regards to both sensory and motor blockade [12]. Lee YY et al., used 2.6 mL of isobaric levobupivacaine and bupivacaine in urological surgeries and found no significant difference between the two drugs [8]. Bergamaschi F et al., found levobupivacaine and bupivacaine to be equally effective for epidural anaesthesia also in patients undergoing LSCS [14]. Luck JF et al., used hyperbaric solutions instead of isobaric and found that both drugs were indistinguishable from each other in their clinical effects in spinal anaesthesia [15].
On the other hand, the following studies reported differences in sensory and motor effect the of two drugs. Héctor J and Malachy O observed potency of motor block to be less by 13% in levobupivacaine group compared to bupivacaine [16]. This may be more important in obstetric, elderly patients and day care surgeries where less motor block may contribute towards less haemodynamic changes intraoperatively and early ambulation post operatively. Sari R et al., compared levobupivacaine and bupivacaine in spinal anaesthesia given for percutaneous nephrolithotomy and concluded that bupivacaine had faster onset time of sensory and motor block and longer duration of motor block [17]. Similar results of faster onset and longer duration of motor block with bupivacaine compared to levobupivacaine have been reported by Altun D et al, Guler G et al., and Goksu H et al., [18-20]. Celik F et al., also reported longer duration of motor block but with slower onset in bupivacaine group patients compared to levobupivacaine [21]. Gulec D et al., compared 3 mL levobupivacaine and 3 mL of bupivacaine in elderly patients undergoing spinal anaesthesia and found slower onset of motor block, shorter sensory block duration with insignificant haemodynamic changes in levobupivacaine compared to bupivacaine [22]. Vellosillo M et al., compared 12.5 mg of isobaric levobupivacaine and 12.5 mg of isobaric bupivacaine in patients undergoing knee arthroscopy. Faster onset of sensory and motor block, longer duration of sensory block and longer pain free postoperative period with similar haemodynamics were seen in bupivacaine group compared to levobupivacaine [23]. Thus, it is clear that while some studies find levobupivacaine and bupivacaine to be equally effective in spinal anaesthesia without significant complications, other studies find levobupivacaine to be less potent in motor block and show less incidence of hypotension in levobupivacaine group compared to bupivacaine. The reason for the observed differences between our results and those seen in the above mentioned studies is not apparent, but it could be attributed to methodological differences, such as difference in the dosage used, in the population studied, or in the potency.
In terms of safety, both intrathecal levobupivacaine and bupivacaine provided a high degree of cardiovascular stability. There was no significant difference in the incidence of perioperative complications between the two groups. Similar findings have been reported in the studies of Glaser C et al., Lee YY et al., Vanna O et al., Luck JF et al., Goksu H et al., Celik F et al., Gulec D et al., Vellosillo M et al., and Bergamaschi F et al., [9,8,12,14,15,20-23]. However few studies reported higher or lower incidence of hypotension in bupivacaine group compared to levobupivacaine group. In the study of Fattorini F et al., two elderly patients of bupivacaine group developed hypotension (70/40 mmHg), bradycardia (40 beats per minute) nausea and weakness within few minutes of spinal puncture [10]. They responded well to oxygen, IV fluids, ephedrine and atropine. In the study of Mantouvalou M et al., requirement of ephedrine was significantly more in bupivacaine group compared to levobupivacaine (42.5% vs. 17.5%), showing greater number of patients developing hypotension (MAP<60 mmHg) in bupivacaine group [2]. Incidence of bradycardia, hypotension (fall greater than 25% or SBP <100 mmHg) and nausea was significantly more in bupivacaine-fentanyl group compared to levobupivacaine-fentanyl group in the study of Guler G et al [19]. In contrast to higher incidence of hypotension in bupivacaine group in the studies mentioned above, Sari R et al., reported hypotension to be more frequent in levobupivacaine group [17].
Limitation
Limitations of our study were a small sample size and only two specific lower abdominal surgeries were selected (inguinal hernioplasty and hydrocele excision).
Conclusion
Intrathecal administration of either 15 mg levobupivacaine or 15 mg bupivacaine was well tolerated and provided similar, effective anaesthesia for lower abdominal surgeries like inguinal hernioplasty and hydrocele excision.
p-value calculated using unpaired t-test
p-value calculated using unpaired t-test
Data are presented as mean±standard deviation p-value calculated using unpaired t-test
p value calculated using unpaired t- test