Right Hilar Mass Diagnosed by Endobronchial Ultrasound Guided Transvascular Needle Aspiration
Asmita Anilkumar Mehta1, Arvind Perathur2
1 Professor, Department of Pulmonary Medicine, Amrita Institute of Medical Sciences, Kochi, Kerala, India.
2 Consultant and Clinical Head, Department of Pulmonary Medicine, Amrita Institute of Medical Sciences, Kochi, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Asmita Anilkumar Mehta, Professor, Department of Pulmonary Medicines, Amrita Institute of Medical Sciences, Amrita Vishwa Vidyapeetham, Ponekkara-682041, Kochi, India.
E-mail: asmitamehta@aims.amrita.edu
The Endo Bronchial Ultrasound–guided Transbronchial Needle Aspiration (EBUSTBNA) for diagnosis and staging of benign and malignant thoracic diseases is the standard of care nowadays. The complications associated with it are rare and minor. We report one case of a 47-year-old male, was evaluated by his primary care physician for complaints of cough, chest pain on right side and episodic dyspnea of one month duration. He was a non smoker and chef by occupation. He denied any history of fever, chills, sputum production, wheezing, or haemoptysis. Chest radiograph showed right lower zone mass. Computed tomography (CT) of the chest revealed well defined a 3×4 centimeter tumorous lesion arising from the right middle lobe bronchus. Fiberoptic bronchoscopy was normal. Endobronchial Ultrasound (EBUS) revealed 2.3×3.3 cm hypoechoic lesion at station 12R lying adjacent to a branch of right inferior pulmonary artery. We examined the pulmonary artery segment using color flow Doppler enhancement. It showed no blood flow over the mass. We next deployed the biopsy needle to its full length into the mass, traversing the near and far walls of the pulmonary artery branch in the process. Rapid on site evaluation by a cytopathologist revealed diagnosis of spindle cell neoplasm.
In present case, we did EBUSTBNA of a right hilar mass traversing the pulmonary artery. There was no vascular injury in the current procedure and with the small diameter needle and real-time guidance such procedures can be performed safely.
Carcinoid, Complications, Transpulmonary artery, Transvascular puncture
Case Report
A 47-year-old man presented with productive cough, occasional wheeze on exertion and chest pain on right side of one month duration. He was a non smoker and known case of systemic hypertension and Type 2 diabetes mellitus was on amlodepine 2.5 mg and diet control for the same since one month. On examination, he was comfortable at rest with respiratory rate of 20/minute and systolic blood pressure 130/80 mmHg. His oxygen saturation was 98% breathing room air. There was no clubbing, cyanosis, lymphadenitis, or dilated veins on general examination. Examination of respiratory system was unremarkable. Blood investigations were as following: Hemoglobin (HB) 14.8 gm/dL, Total white blood cell count 8,400/mm3, neutrophil 48%, lymphocytes 41% and eosinophil 7%. Renal function test, liver function test and prothrombin time were within normal limit. A posteroanterior chest radiograph demonstrated right paracardiac opacity [Table/Fig-1].
Chest radiograph showing solitary pulmonary nodule in right lower zone.

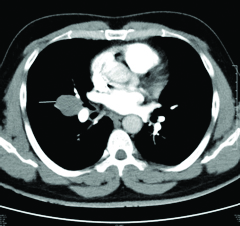
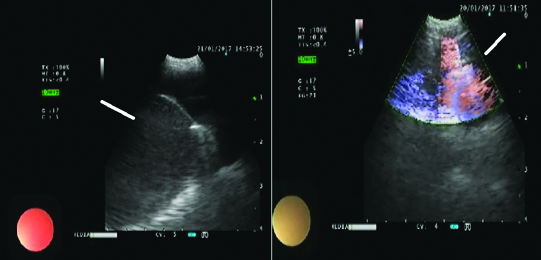
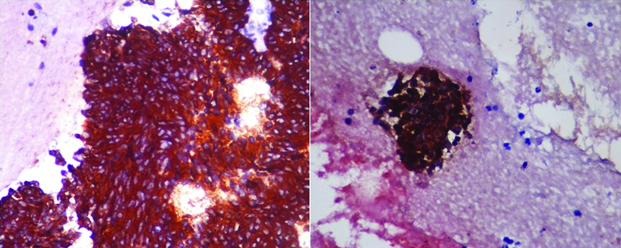
Computerised tomographic pulmonary angiogram revealed a soft tissue lesion with smooth rounded borders measuring 2.6x2.9 cm at the right hilum along the descending pulmonary artery and the right middle lobe bronchus. A small blind ending bronchus was seen arising from the main middle lobe bronchus extending to the lesion with medial and lateral segment branches of middle lobe seen separately. The differential diagnosis of bronchogenic cyst, bronchogenic carcinoma or rare lymphoma were considered. Fiberoptic bronchoscopy was done which showed extrinsic compression on right middle lobe bronchus. [Table/Fig-2]. Following, the patient underwent EBUS. It was done using a bronchoscope equipped with a distal 7.5 MHz linear ultrasound transducer probe and dedicated ultrasound image processor (Olympus model) It showed 2.3×3.3 cm hypoechoic lesion at station 12R with pulmonary artery lying above it. We examined the pulmonary artery segment using color flow Doppler enhancement to demonstrate blood flow. The mass was not showing any blood flow. Next, the needle was deployed into the mass. The needle traversed through the near and far walls of the pulmonary artery branch for the process. Four separate passes were made and minimal bleeding was noted [Table/Fig-3]. The patient tolerated the procedure well. Rapid on-site cytopathologic evaluation confirmed the presence of adequate tissue for evaluation with few suspicious cancerous cells. Cell block was prepared from EBUS aspirate which was processed for Immune Histochemistry (IHC). The IHC came positive for synaptophysin and chromographin [Table/Fig-4]. Final diagnosis was spindle cell neuroendocrine neoplasm. Post procedure period was uneventful without any complications. Positron emission tomography was done for staging and it showed FDG avid lesion in middle lobe with Standardised uptake value (SUV) of 6.9. No other lesions were seen and staging was T2N0M0-Stage 1 b. He was referred to cardiothoracic surgeon for right middle lobectomy but due to personal reason he deferred the procedure.
Computed tomography image showing a 2.6×2.9 cm well defined soft tissue lesion at the right hilum along the descending pulmonary artery and the middle lobe bronchus.
Endobronchial ultrasound image showing a 2.3×3.3 cm hypoechoic lesion at station 12R with pulmonary artery lying above it. Doppler showed vascular flow above mass.
Histopathology image: Immunohistochemistry (40X) showing cluster of spindle cells positive for synaptophysin and chromogranin.
Discussion
The EBUS guided transbronchial needle aspiration has rapidly evolved in to the standard of care for diagnosis and staging of benign and malignant thoracic lesions [1]. Use of EBUS allows realtime sampling of lesions. By using doppler, we can also avoid vascular puncture [1]. But accidental vascular punctures happen often with no reported complications. Using convex probe EBUS (CP-EBUS) gives unique ability to show blood flow using the colour Doppler US in addition to the US real time images, helping us to differentiate Lymph Nodes (LN), necrotic areas, and mediastinal cysts from vascular structures [1,2]. To identify various thoracic vessels is an integral part of EBUS procedure. Current staging system uses vascular landmarks to delineate several lymph node stations [3]. In rare cases, the clinician face difficult situation in which a minimally invasive approach to the lymph nodes or mass through vessel is required. We present a case of right middle lobe mass for which the diagnosis was obtained by doing transvascular neddle aspiration. We found only few cases reported on transvascular EBUS guided TBNA and getting successful diagnosis in literature [Table/Fig-5] [4-8]. As shown in [Table/Fig-5] there was no significant bleeding or any other complications reported by various authors after Transvascular Needle Aspiration (TVNA) [4-8]. The reason is that the pulmonary artery is a high flow, low-pressure system, it is possible to traverse its wall with a fine needle of 21 or 22G and it is likely to be immediately sealed upon removal of the needle, if there is no laceration of the vessel. Some authors also suggested that low pressure vessels such as PA bleeding would cease without packing and there is no risk of haematoma or pseudoaneurysm as they are packed between mediastinal structure unlike pleural cavity or open air space.
Literature review of TVNA cases till date and comparison with present case.
| Authors | No. of cases | Location of target | Diagnosis | Needle | Complications |
|---|
| Vincent B et al., [4] | 1 | Left hilar mass adjacent to the left inferior pulmonary artery | Carcinoid tumour | EBUS/22G | None |
| Folch E et al., [5] | 4 | Station 5 LN | Definitive diagnosis of malignancy in 3 cases, fourth case required thoracoscopy | EBUS/21G | None |
| Boujaoude Z et al., [6] | 2 | 1. LN in station 11R through right pulmonary artery.2. Right perihilar lung nodule through right lower branch of pulmonary artery | 1. Adenocarcinoma with lung primary2. Papillary adenocarcinoma of lung | EBUS/21G | None |
| Panchabhai TS et al., [7] | 5 | Station 5 lesions through pulmonary artery (n=3) Station 6 lesions through Aorta (n=2) | Three cases diagnosed with malignancy. One biopsy bronchogenic cyst. One biopsy was non-diagnostic | EBUS/21G | None |
| Folch E et al., [8] | 10 | Station 5 lesions | Cases got confirmed diagnosis, one showed atypical cells requiring VATS | EBUS/21G | None |
| Present case | 1 | Station 12R through right pulmonary artery | Neuroendocrine tumour | EBUS/21G | None |
Conclusion
In summary, we performed successful diagnostic EBUS-guided TBNA of a hilar mass traversing the pulmonary artery. There was no vascular injury. We believe that as the procedure was done under real time guidance with small diameter needle, there was no complications.
[1]. Silvestri GA, Gonzalez AV, Jantz MA, Margolis ML, Gould MK, Tanoue LT, Methods for staging non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of chest physicians evidence-based clinical practice guidelinesChest 2013 143(5 suppl):e211S-e2150. [Google Scholar]
[2]. Kinsey CM, Arenberg DA, Endobronchial ultrasound-guided transbronchial needle aspiration for non-small cell lung cancer stagingAm J Respir Crit Care Med 2014 189(6):640-49.10.1164/rccm.201311-2007CI24484269 [Google Scholar] [CrossRef] [PubMed]
[3]. Navani N, Nankivell M, Lawrence DR, Lock S, Makker H, Baldwin DR, Lung cancer diagnosis and staging with endobronchial ultrasound-guided transbronchial needle aspiration compared with conventional approaches: an open label, pragmatic, randomised controlled trialLancet Respir Med 2015 3(4):282-89.10.1016/S2213-2600(15)00029-6 [Google Scholar] [CrossRef]
[4]. Vincent B, Huggins JT, Doelken P, Silvestri G, Successful real-time endobronchial ultrasound-guided transbronchial needle aspiration of a hilar lung mass obtained by traversing the pulmonary arteryJ Thorac Oncol 2006 1(4):362-64.10.1097/01243894-200605000-0001617409884 [Google Scholar] [CrossRef] [PubMed]
[5]. Folch E, Santacruz J, Machuzak M, Gildea T, Majid A, Safety and efficacy of EBUS-guided TBNA through the pulmonary artery: A preliminary reportChest J 2011 140(4):600A10.1378/chest.1119000 [Google Scholar] [CrossRef]
[6]. Boujaoude Z, Pratter M, Abouzgheib W, Transpulmonary artery needle aspiration of hilar masses with endobronchial ultrasound: a necessary evilJ Bronchology Interv Pulmonol 2013 20(4):349-51.10.1097/LBR.000000000000001124162122 [Google Scholar] [CrossRef] [PubMed]
[7]. Panchabhai TS, Machuzak MS, Sethi S, Vijhani P, Gildea TR, Mehta AC, Endobronchial ultrasound guided transvascular needle aspiration A single center experienceJ Bronchol Intervent Pulmonol 2015 22(4):306-11.10.1097/LBR.000000000000022726492603 [Google Scholar] [CrossRef] [PubMed]
[8]. Folch E, Santcruz JF, Fernandez BS, Gangadharan S, Kent MS, Jantz M, The feasibility of EBUS guided TBNA through the pulmonary artery in highly selected patientsJ Bronchology Interv Pulmonol 2016 23(1):7-13.10.1097/LBR.000000000000024526705006 [Google Scholar] [CrossRef] [PubMed]