Digital Gangrene in Association with Retinoblastoma
Sarthak Das1, Barath Jagadisan2, Niranjan Biswal3, Sriram Krishnamurthy4, Subashini Kaliaperumal5
1 Assistant Professor, Department of Paediatrics, JIPMER, Karaikal, Puducherry, India.
2 Associate Professor, Department of Paediatrics, JIPMER, Karaikal, Puducherry, India.
3 Senior Professor, Department of Paediatrics, JIPMER, Karaikal, Puducherry, India.
4 Additional Professor, Department of Paediatrics, JIPMER, Karaikal, Puducherry, India.
5 Additional Professor, Department of Opthalmology, JIPMER, Karaikal, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sarthak Das, Block D4, JIPMER Hostel Complex Velatheeru, Karaikal-605006, Puducherry, India.
E-mail: drsarthakdas2222@gmail.com
We report a 5-year old boy, diagnosed with Retinoblastoma (RB) in the right eye and subsequently developed digital gangrene as a result of Raynaud’s phenomenon. Color Doppler ultrasound showed occlusion of radial and ulnar arteries of the left upper limb. Antinuclear Antibody, Antiphospholipid Antibody (APLA) and rheumatoid factors were negative. The patient was treated with low molecular weight heparin (enoxaparin), nifedipine, and analgesics. Raynaud’s syndrome and digital gangrene constitute a rare paraneoplastic process, which was not reported with retinoblastoma earlier.
Paraneoplastic syndrome, Raynaud’s phenomenon, Color doppler ultrasound
Case Report
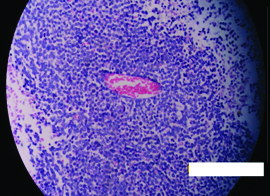
A 5-year-old boy presented with progressive proptosis, pain and progressive visual loss of the right eye for one month and was provisionally diagnosed to have RB on the basis of these features. Without delay, enucleation was done and histopathology of the tissue confirmed retinoblastoma with Flexner-Wintersteiner rosettes and areas of calcification [Table/Fig-1,2]. The child was advised chemo radiation in view of choroidal, scleral and optic nerve invasion by the tumour along with involvement of the resected margins as seen histopathologically.
Child after enucleation with swollen soft tissue around the eye.

Histopathology of retinoblastoma: Flexner wintersteiner rosette with necrosis (H&E stain 40X).
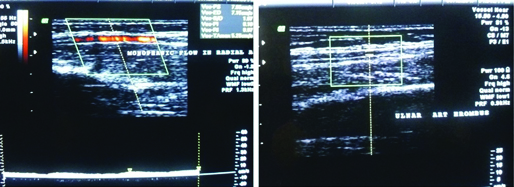
After 10 days of enucleation, the patient presented with multiple episodes of convulsions and vomiting which were not associated with fever. Cardio-respiratory and neurological examination were normal. The peripheral pulses in all limbs were equally palpable. Clinically suspecting increased intracranial pressure patient started treatment empirically with mannitol and phenytoin. Patient improved symptomatically within 48 hours of admission and on day 3 of admission, the patient developed pain and bluish discolouration of the digits of the left hand [Table/Fig-3,4]. The left hand was less warm than the right. The left radial pulse was not palpable. The child did not have a history suggestive of collagen vascular disease or Raynaud’s phenomenon in the past. Color Doppler showed occlusion of radial and ulnar arteries of the left limb [Table/Fig-5].
Pallor and early gangrene at presentation Progression of gangrene.

Occlusion of radial and ulnar arteries of the left limb.
Complete blood count, prothrombin time, erythrocyte sedimentation rate, HBsAg, IgM anti HBc, serum triglycerides and serum cholesterol were within normal limits. Antinuclear antibody, APLA and rheumatoid factor were negative. The patient was treated with low molecular weight heparin (enoxaparin), nifedipine and analgesics. The bluish discoloration progressed to gangrenous lesions of the fingers of the left hand within 3-5 days with a line of demarcation above the wrist [Table/Fig-4].
There was no involvement of any other part of the body. After a definite demarcation line was confirmed, the patient underwent surgical amputation of left hand above the wrist. Patient was discharged with antiseizure medication and continued chemoradiation on follow-up. Within one month of discharge, patient developed status epilepticus in home and died on the way to hospital.
Discussion
Digital gangrene is a rare and recognised paraneoplastic phenomenon. It has been described in association with various tumours including lymphoma, breast, renal, lung, and gastrointestinal cancers [1,2]. Retinoblastoma is the most common intraocular tumour in children worldwide with a mortality of up to 50-70% in underdeveloped countries [3]. Current management for intraocular RB include chemo reduction, enucleation, external beam radiation therapy and focal treatment (e.g. cryotherapy, photocoagulation and brachytherapy) [4]. Prognosis is largely related to early detection [3,4].
Paraneoplastic syndromes refer to pathological conditions that are caused by a cancer but not brought about directly by local infiltration or metastatic spread [1]. They are relatively common with a reported prevalence of 5-10% in the general cancer population [1,2]. Raynaud’s phenomenon is defined as episodes of cold-induced pallor and/or cyanosis of the distal portions of fingers and toes [1,2]. In most of the cases, the problem is an isolated phenomenon known as primary Raynaud’s phenomenon or Raynaud’s disease [1,2]. In secondary Raynaud’s phenomenon, it is associated with underlying diseases which may be connective tissue diseases and rarely malignancies (paraneoplastic Raynaud’s phenomenon) [1,2].
Raynaud’s phenomenon has been reported in association with a variety of different malignancies including sarcomas, gastrointestinal, haematological, lymph reticular and pulmonary malignancies [1,2]. On a PubMed search, the authors could not find any prior report of digital gangrene associated with retinoblastoma. In the absence of a definite emboli and lack of evidence of rheumatologically and autoimmune diseases, the digital gangrene seen in the patient points towards a paraneoplastic phenomenon.
The possible pathogenetic mechanisms of paraneoplastic Raynaud’s phenomenon include arteritis, hyperviscosity and hypercoagulability probably related to tumour antigen-antibody complexes with activation of complement system [1,2,5]. Hyperviscosity has also been reported as a mechanism of ischaemia [3,5]. Hyperviscosity resulting from an increase in the number of circulating blood cells has been described earlier in chronic granulocytic leukemia [1]. Elevated cryoglobulin levels leading to pseudo-Raynaud’s disease with progression to gangrene has been described in pulmonary adenocarcinoma [2]. The arterial thrombosis seen in the present case progressed rapidly despite anticoagulant therapy. The relative resistance to treatment in this form of hypercoagulability has been well described in literature [1].
Various treatment modalities for Raynaud’s phenomenon include non-pharmacological (keeping the hand warm), pharmacological and surgical (sympathectomy) interventions. Pharmacological agents effective in this condition are vasodilators such as calcium channel blockers (e.g., nifedipine) and angiotensin II inhibitors and selective serotonin reuptake inhibitors [2].
Conclusion
The authors emphasise that due to the rarity of gangrene complicating retinoblastoma, many clinicians may not be familiar with the presentation encountered in the present study. Retinoblastoma should be added to the compendium of malignancies that may be complicated by paraneoplastic Raynaud’s phenomena.
[1]. Schildmann EK, Davies AN, Paraneoplastic Raynaud’s phenomenon-good palliation after a multidisciplinary approachJ Pain Symptom Manage 2010 39(4):779-83.10.1016/j.jpainsymman.2009.09.00620199852 [Google Scholar] [CrossRef] [PubMed]
[2]. Smith IE, de Boer RH, Paraneoplastic syndromes other than metabolic. In: Souhami RL, Tannock I, Hohenberger P, Horiot JC, edsOxford textbook of oncology 2002 2nd edOxford, UKOxford University Press:933-58. [Google Scholar]
[3]. Jabbour P, Chalouhi N, Tjoumakaris S, Gonzalez LF, Dumont AS, Chitale R, Pearls and pitfalls of intraarterial chemotherapy for retinoblastomaJ Neurosurg Pediatr 2012 10(3):175-81.10.3171/2012.5.PEDS127722793160 [Google Scholar] [CrossRef] [PubMed]
[4]. Khetan V, Gupta A, Gopal L, Retinoblastoma: Recent trends a mini review based on published literatureOman J Ophthalmol 2011 4(3):108-15.10.4103/0974-620X.9126522279397 [Google Scholar] [CrossRef] [PubMed]
[5]. Onitilo AA, Demos-Bertrand J, Depke J, Resnick JM, Engel J, Digitalis chemia as a paraneoplastic consequence of squamous cell lungcarcinomaWMJ 2012 111(3):138-41. [Google Scholar]