MR Imaging in Idiopathic Inflammatory Polymyositis: Case Report and Review of Literature
Pratiksha Yadav1, Ashim Wokhlu2
1 Professor, Department of Radiology and Imaging, Dr. D.Y. Patil Medical College, Hospital and Research Centre, Pune, Maharashtra, India.
2 Assistant Professor, Department of Orthopedics, SMT. Kashibai Navle Medical College and General Hospital, Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pratiksha Yadav, Professor, Department of Radiology and Imaging, Dr. D.Y. Patil Medical College, Hospital and Research Centre, Pimpri, Pune-411018, Maharashtra, India.
E-mail: yadavpratiksha@hotmail.com
Idiopathic Inflammatory Myopathies (IIM) are a group of rare autoimmune disorders which present clinically with proximal muscle weakness. Diagnosis of IIM involves clinical history, pathological investigation, imaging studies and histologic examination. It shows muscle weakness on Electromyography (EMG) and increased level of muscle enzymes. MRI is very useful to demonstrate the soft tissue and muscle changes in the IIM. MRI of whole body, especially peripheral limbs show typical findings which help in diagnosis, extent and severity of disease as well as follow up. We report a case of 31-year-old male who came with a complaint of muscle weakness since six months. The level of Creatinine Phosphokinase (CPK) was high. MRI of both upper and lower limbs showed diffuse symmetrical altered signal intensities involving the muscles of both upper and lower limbs. Biopsy was advised which was positive for idiopathic inflammatory polymyositis.
Creatinine phosphokinase, Dermatomyositis, Muscle weakness
Case Report
We present a case of a 31-year-old male who came with chief complaint of generalised muscle weakness since 6-7 months. Difficulty to walk, climb stairs and lift hands and legs since 6 months. Facial and extra-ocular muscles were normal. No bladder or bowel complaints were there. There was no history of trauma or fall. No history of diabetes mellitus was present.
On clinical examination, there were atrophy of the muscles of the bilateral upper and lower limbs. Muscle weakness was seen in upper and lower limbs. Strength of the specific muscles groups like ‘extensors’ and ‘flexor’ groups were examined against resistance and one limb muscles examination compared with other side. Decreased resistance observed in all the flexors and extensors of upper and lower limbs. Lower limb muscles were more affected. The skin of the limbs was normal and no evidence of any rash or erythema was seen. No subcutaneous oedema was observed on clinical examination. Joints were normal on examination. His Haemoglobin (Hb) was 13.2 gm/dL and TLC was 5800. Serum urea (22.8 mg/dL), serum creatinine (0.81 mg/dL), Serum bilirubin Total (0.81 mg/dL), direct (0.32 mg/dL), indirect (0.49 mg/dL) were in normal range. Serum Glutamic Oxaloacetic Transaminase (SGOT) was raised and showed value of 98 IU/L. Serum electrolytes investigations revealed normal range of Serum sodium 137 mEg/L, serum potassium 4.4 mEg/L, serum chlorides 99 mEg/L; however, serum CPK were highly raised and showed value of 14088 IU/L. Electromyography (EMG) was suggestive of primary muscle disease.
Antero-posterior and Lateral radiograph of both the upper limbs were normal. CT scan of the bilateral lower and upper limb was done on ‘128 slice Philips CT scanner’, which revealed no abnormality on bones and joints.
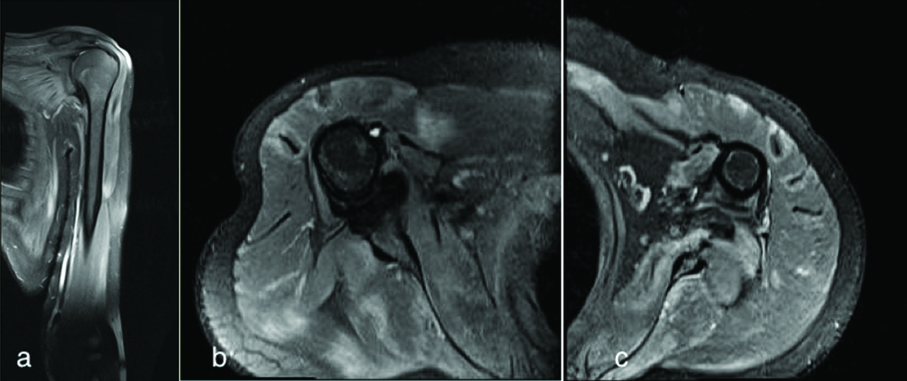
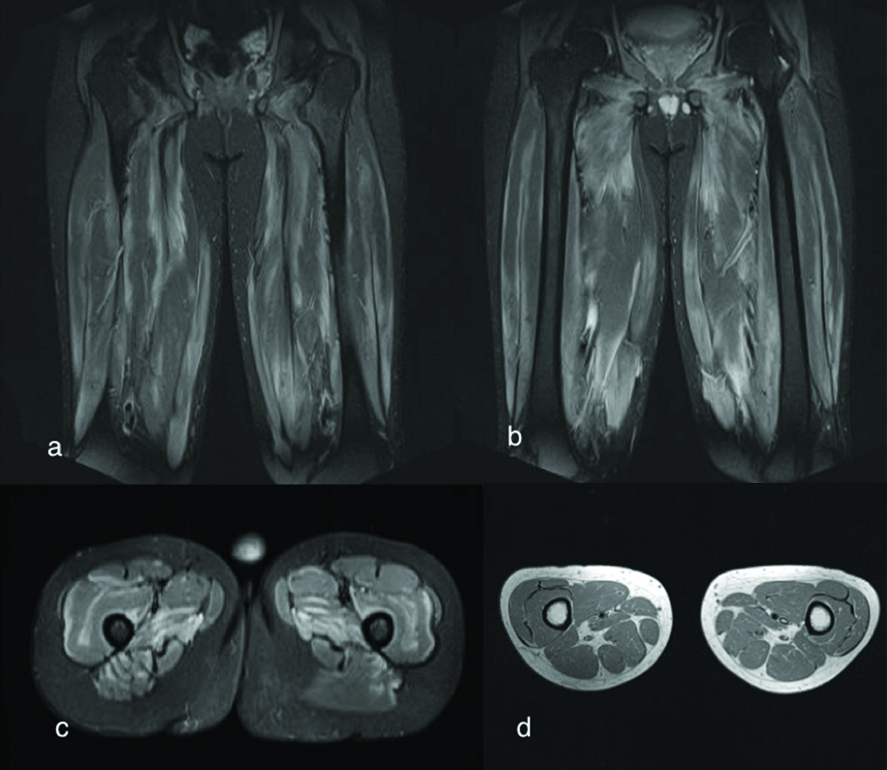
MRI of both the upper and lower limbs were advised. MRI was done on ‘1.5 Tesla Seimen’s Avanto machine’. Right and left shoulder MRI with upper limb were done on the dedicated shoulder coil separately. Axial and coronal T2WI, T1WI, STIR and PDFS were obtained and T2W sagittal images were obtained in 3 mm slice thickness. Both the lower limbs MRI were done on the body coil Axial and coronal T2WI, T1WI and STIR images were obtained in 3 mm slice thickness. On MRI there were diffuse patchy altered signal intensities seen in all the muscles of both arms and on the muscles of upper back (subscapularis, teres minor and teres major), which showed hyperintense signals on T2WI and STIR [Table/Fig-1a-c]. Altered signal intensity involved both thigh and leg muscles which are hyperintense on T2WI and STIR [Table/Fig-2a-c] and not visualised on T1WI. These altered signal intensities are bilaterally symmetrical and involving predominantly along the fascia [Table/Fig-2d]. These hyperintense signals on T2WI and STIR are suggestive of muscle oedema and inflammation. Muscles of arms appear atrophied. Subcutaneous tissue was not involved. Underlying bones were normal. The osseous structures appeared normal. No joint effusion was seen. These findings were suggestive of polymyositis.
a) Coronal T2WI of right shoulder showing hyperintense signal intensities involving the upper arm and shoulder muscles; b) STIR axial images of right shoulder and; c) STIR axial image of left shoulder showing diffuse symmetrical hyperintense signals involving the muscle along the fascia in the upper limb.
a,b) Coronal T2WI images of the bilateral thigh showing diffuse symmetrical hyperintense signals involving the muscle along the fascia; c) STIR Axial image of bilateral lower limb showing hyperintense signals; d) Axial T1WI of bilateral lower limb did not show any signal abnormality.
Biopsy of the inner vastus medialis muscles was done, which revealed endomysial mononuclear cell infiltrates and muscle fibers necrosis suggestive of polymyositis. Patient was advised corticosteroids, prednisone is 0.5-1 mg/kg/day and physiotherapy. On follow up, four weeks later he showed improvement. Patient was improved on the muscle weakness, the patient was able to walk and climb stairs. MRI was not repeated on follow up.
Discussion
The IIM are a group of autoimmune disorders in which polymyositis and dermatomyositis are more recognised forms [1]. The IIM is a rare disorder and estimated annual incidence of only 10 new cases per million people [2]. It is characterised by inflammation of the muscles which leads to muscle weakness, Muscle enzyme elevation. Facial and extraocular muscle are spared though pharyngeal or respiratory muscles can be involved [3]. It can be associated with fatigue, dysphagia and respiratory problems. On biopsy of the muscle it shows inflammation. The diagnosis and treatment often delayed, as frequently the patient present with vague complaints of fatigue, muscle weakness and arthralgia. The serum level of Creatinine Kinase (CK) is a most commonly performed enzyme investigation for diagnosis of myositis [1,4,5]. The MR imaging of peripheral limbs shows a typical finding in the polymyositis which is very useful along with clinical findings and pathological investigation in accurate diagnosis of IIM. It helps in the severity, extend of the disease, follow up of disease treatment and response to treatment [6].
Inflammatory Myopathies/polymyositis is an autoimmune disorder which is characterised by symmetric muscle weakness, characteristic EMG findings, increase in serum muscle enzyme levels and muscle biopsy shows inflammation.
Bohan A classified idiopathic inflammatory myopathies in to 7 categories [7].
I) Primary idiopathic polymyositis
II) Primary idiopathic dermatomyositis
III) Polymyositis or dermatomyositis associated with malignancy
IV) Childhood polymyositis or dermatomyositis
V) Polymyositis or dermatomyositis associated with other connective tissue disease
VI) Inclusion body myositis
VII) Misclleneus–Eosinophilic myositis, myositis ossificans, Giant cell myositis, focal myositis.
Dermatomyositis is similar in muscle distribution; however, it involves skin and presents with skin rash like heliotrope rash. Pathogenesis differs in dermatomyositis as it involves vascular endothelium of capillaries. Polymyositis and dermatomyositis both may be associated with malignancy [8].
It is an autoimmune disorder, secondary to defective cellular immunity, it may have diverse causes which can occur alone or in association with connective tissue disorder, viral infections or malignancies.
Imaging studies with ultrasound and MRI are very useful. On ultrasound polymyositis can demonstrate muscle atrophy and can show increased echogenicity as compare to normal muscle echogenicity. The MRI is more sensitive modality for evaluation of myositis, it can evaluate the muscle involvement, extent of fatty replacement, muscle atrophy and severity of the disease. Short TI Inversion Recovery (STIR)sequence is very sensitive to depict the change in water content and inflammation which demonstrated as increased signal intensity in the involved muscles. The MRI is a useful imaging modality to localise the site for muscle biopsy. More recently Ultrasound can also demonstrate the changes in muscle [9]. Histopathology after muscle biopsy in polymyositis demonstrate lymphocytic infiltration, mostly in fascicles, fiber necrosis, degenerative and regenerative fibers [10]. Result of biopsy can be normal in 10-15% of myositis cases because of patchy nature of the inflammation [11,12]. Five years survival rate for IIM patients range from 63%-95% [13].
Mimics of myositis are of many kind and it is essential to differentiate, it from other causes of myalgias and weakness. Endocrinopathies, food supplements, drugs, dystrophies and psychiatric conditions are some causes for muscle weakness and myalgias [10].
Main aim of the treatment was to regain muscle strength, control inflammation and to prevent the other organ damage. Treatment was immunosuppression, physical therapy and avoidance of complications. High dose corticosteroids was the first line of treatment. Initial dose of prednisone was 0.5-1 mg/kg/day. Dose of prednisone tapered after few weeks to lowest dose. Monitoring serum enzyme level and muscle strength should be evaluated to observe the treatment response. Common side effects of high dose corticosteroids were sleep disturbances, psychosis, glaucoma, avascular necrosis, hypertension and osteoporosis. Second line treatment can start in severe cases or after several months of prednisone. Second line treatment include methotrexate, azathioprine and intravenous immunoglobin. Side effects of methotrexate are gastrointestinal pain and alopecia [13].
Conclusion
The MRI is very useful imaging technique for the diagnosis and evaluation of idiopathic inflammatory myopathies. The MR imaging is useful in the guidance for muscle biopsy and to evaluate the treatment response.
[1]. Miller FW, Inflammatory Myopathies: Polymyositis, dermato-myositis, and related conditionsIn: Arthritis and Allied Conditions. W. Koopman and L. Moreland Lippincott Eds. A Textbook of Rheumatology 2005 PhiladelphiaWilliams and Wilkins:1593-620. [Google Scholar]
[2]. Rider LG, Miller FW, Deciphering the clinical presentations, pathogenesis, and treatment of the idiopathic inflammatory myopathiesJ Am Med Assoc 2011 305(2):183-90.10.1001/jama.2010.197721224460 [Google Scholar] [CrossRef] [PubMed]
[3]. Gazeley DJ, Cronin ME, Diagnosis and treatment of the idiopathic inflammatory myopathiesTher Adv Musculoskeletal Dis 2011 3(6):315-24.10.1177/1759720X1141530622870489 [Google Scholar] [CrossRef] [PubMed]
[4]. Munsat TL, Baloh R, Pearson CM, Fowler WJ, Serum enzyme alterations in neuromuscular disordersJ Am Med Assoc 1973 226(13):1536-43.10.1001/jama.1973.03230130024009 [Google Scholar] [CrossRef]
[5]. Rider LG, Miller FW, Laboratory evaluation of the inflammatory myopathiesClin Diagn Lab Immunol 1995 2(1):1-9. [Google Scholar]
[6]. Elessawy SS, Abdelsalam EM, Abdel Razek E, Tharwat S, Whole-body MRI for full assessment and characterization of diffuse inflammatory myopathyActa Radiologica Open 2016 5(9):205846011666821610.1177/205846011666821627708860 [Google Scholar] [CrossRef] [PubMed]
[7]. Bohan A, History and classification of polymyositis and dermatomyositisClin Dermatol 1988 6(2):3-8.10.1016/0738-081X(88)90044-2 [Google Scholar] [CrossRef]
[8]. Zampieri S, Valente M, Adami N, Biral D, Ghirardello A, Rampudda ME, Polymyositis, dermatomyositis and malignancy: a further intriguing linkAutoimmun Rev 2010 9(6):449-53.10.1016/j.autrev.2009.12.00520026430 [Google Scholar] [CrossRef] [PubMed]
[9]. Botar-Jid C, Damian L, Dudea SM, Vasilescu D, Rednic S, Badea R, The contribution of ultrasonography and sonoelastography in assessment of myositisMed Ultrason 2010 12(2):120-26. [Google Scholar]
[10]. Castro C, Gourley M, Diagnosis and treatment of inflammatory myopathy: issues and managementTher Adv Musculoskelet Dis 2012 4(2):111-20.10.1177/1759720X1142509222870499 [Google Scholar] [CrossRef] [PubMed]
[11]. Bohan A, Peter JB, Polymyositis and dermatomyosistis (First of two parts)N Eng J Med 1975 292(7):344-347.10.1056/NEJM1975021329207061090839 [Google Scholar] [CrossRef] [PubMed]
[12]. Bohan A, Peter JB, Polymyositis and dermatomyosistis (Second of two parts)N Eng J Med 1975 292:403-07.10.1056/NEJM1975022029208071089199 [Google Scholar] [CrossRef] [PubMed]
[13]. Ng KP, Ramos F, Sultan SM, Isenberg DA, Concomitant diseases in a cohort of patients with idiopathic myositis during long-term follow-upClin Rheumatol 2009 28(8):947-53.10.1007/s10067-009-1181-419387765 [Google Scholar] [CrossRef] [PubMed]
[14]. Villalba L, Hicks JE, Adams EM, Sherman JB, Gourley MF, Leff RL, Treatment of refractory myositis: a randomized crossover study of two new cytotoxic regimensArthritis Rheum 1998 41(3):392-99.10.1002/1529-0131(199803)41:3<392::AID-ART3>3.0.CO;2-X [Google Scholar] [CrossRef]