Pulmonary Embolism Following Varicella Infection
A S Sandhya1, Brijesh Prajapat2
1 Assistant Professor, Department of Chest and Respiratory Diseases, Pt. BD Sharma PGIMS, Rohtak, Haryana, India.
2 Senior Resident, Department of Pulmonary and Critical Care Medicine, Pt. BD Sharma PGIMS, Rohtak, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Brijesh Prajapat, House No-324, Sector-14, Rohtak, Haryana, India.
E-mail: dr.brijeshprajapat@gmail.com
Venous Thromboembolism (VTE) post varicella infection is a rare complication owing to vascular endothelial damage, accelerated atherosclerosis and antibody-mediated hypercpagulable state. Pulmonary embolism (PE) is a life threatening condition presented with sudden onset dyspnoea and refractory hypoxemia. We report a case of post varicella extensive thrombotic complication which involved deep veins of lower limbs and pulmonary vasculature.
Atherosclerosis, Endothelium, Hypercoagulability, Refractory hypoxemia, Thrombolytics
Case Report
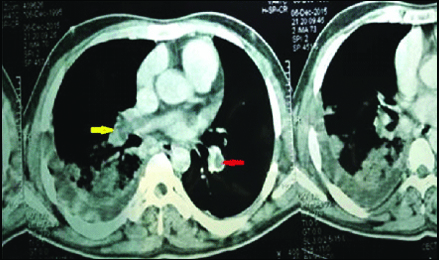
A 20-year-old immunocompetent male patient who was a student from Rohtak, India, presented with sudden onset breathlessness for two days, cough and minimal hemoptysis for one day in the emergency department. Patient was being treated for Varicella Zoster (VZ) infection before presentation for the past 7-8 days as an outpatient basis with acyclovir therapy and local application of calamine lotion. He had rashes all over his body which were in various stages of healing. He did not have any history of other previous illness, comorbidities or other significant family history. He was a non-smoker and there was no history of drug abuse or addiction. On examination, patient was conscious, oriented, afebrile and in severe respiratory distress. His blood pressure was 80/60 mmHg, heart rate was 110/min, oxygen saturation 64% at room air and respiratory rate was 38/minutes. His total leucocyte count was 17000/cumm, haemoglobin was 12 mg/dL. Liver and kidney function tests were within normal limits and arterial blood gases revealed respiratory alkalosis and hypoxemia (pH= 7.45; paO2= 48 mm/hg; paCO2=29). He was managed with oxygen, fluid therapy, vasopressor support and antibiotics in the emergency department. Chest X-ray revealed right lower zone homogenous opacity, cardiomegaly and bilateral hilar prominence [Table/Fig-1]. Electrocardiography (ECG) revealed sinus tachycardia with right axis deviation. There was swelling over the left leg and later venous Doppler showed thrombus in left common femoral, superficial femoral, deep femoral and popliteal veins. CT pulmonary angiography showed thrombus in right main pulmonary artery and in left descending pulmonary artery [Table/Fig-2,3]. There was right lower lobe consolidation which was suggestive of infarct. In view of his deranged haemodynamic profile and presence of Right Ventricle (RV) dysfunction assessed by echocardiography, Patient was immediately thrombolysed with alteplase following which there was improvement in his oxygenation and haemodynamic status of the patient. He was gradually taken off vasopressors slowly and started on enoxaparin (60 mg) twice a day along with warfarin. Warfarin dose was slowly escalated to maintain the Internatonal Normalised Ratio (INR) between 2-3. Patient improved clinically and had no further episodes of hemoptysis and was discharged after seven days on warfarin at a dose of 6 mg once a day.
Chest X-ray revealing right lower zone opacity.
CT cut showing thrombus in right pulmonary artery which is seen as filling defect (yellow arrow) with area of infarction in the right lower lobe (red arrow).

Thrombus in right pulmonary artery (yellow arrow) and in left descending pulmonary artery (red arrow) with area of infarction on right side.
Discussion
Out of all chickenpox infections (VZ virus) encountered, only 2% occur in adults; however, it is responsible for 25% of the fatalities in this age group [1]. Varicella infection is responsible for various systemic complications like encephalitis, bacterial infections, sepsis, thrombocytopenia, thromboembolism, keratitis, conjunctivitis, uveitis, nephritis, the Syndrome of Inappropriate Antidiuretic Hormone secretion (SIADH), myocarditis, orchitis, and Henoch–Schonlein purpura [2]. Post-mortem studies have shown involvement of the liver, spleen, pancreas, lymph nodes, and esophagus [3]. Here we present a case of a young immunocompetent man who developed VZ pneumonitis and later Deep Vein Thrombosis (DVT) and massive PE.
Thrombotic complications post varicella infection is not common and can present as purpura fulminans, necrotising vasculitis, cerebral venous thrombosis, DVT and PE. Ali MS et al., described a case of iliofemoral vein thrombosis in a patient with chickenpox and postulated this as a direct result of the VZV infection [4]. Choi WY et al., and recently Mohanty B, too described cases of DVT in patients of varicella infection [5,6]. Cases of extensive thrombosis involving cortical venous sinus, deep veins of leg, pulmonary vasculature and right atrium has been reported [7]. Pulmonary embolism is a rare but serious complication of varicella infection. Endothelial damage and accelerated atherosclerosis resulting from varicella infection seems to be the cause of VTE in these patients. The varicella virus has specifically been linked with vascular damage in various organs including the lungs, pleura, and brain [8]. Vascular endothelial wall damage or endothelial activation or antiphospholipid antibodies are implicated in the pathophysiology of thrombosis [9,10]. Varicella infected endothelium shows enhanced thrombin generation and platelet binding. Thromboembolic events could also be secondary to transient Protein-S deficiency, which has been documented after varicella infection, caused by antiprotein-S antibodies [3]. Due to underdiagnosis epidemiological data regarding the incidence of thromboembolism in VZ infection are lacking. Most of the cases have been reported in children till now. Thus, high index of suspicion is needed for the identification of thrombotic complications of this disease.
Conclusion
Embolic phenomenon should be considered in the differential diagnosis of pulmonary symptoms associated with varicella infection since, their early diagnosis and treatment is necessary in preventing mortality.
[1]. Feldman S, Varicel la-zoster virus pneumonitisChest 1994 106(1 Suppl):22S-7S.10.1378/chest.106.1_Supplement.22S8020329 [Google Scholar] [CrossRef] [PubMed]
[2]. Dahan E, Simsolo C, Merei M, Vigder F, Tatoor I, Blum A, Varicella zoster infection and pulmonary complicationsEuropean Journal of Internal Medicine 2005 16(6):449-50.10.1016/j.ejim.2005.02.01116198910 [Google Scholar] [CrossRef] [PubMed]
[3]. McColl MD, Chalmers EA, Rafferty I, Pulmonary embolism associatedwith varicella infectionBr J Haematol 1998 102(5):1384-85. [Google Scholar]
[4]. Ali MS, Kutty MS, Corea JR, Kutty K, Iliofemoral thrombosis in a case of chicken poxAngiology 1984 35:577-78.10.1177/000331978403500905 [Google Scholar] [CrossRef]
[5]. Choi WY, Cho YK, Ma JS, Herpes zoster complicated by deep vein thrombosis : a case reportKorean J Pediatr 2009 52:607-10.10.3345/kjp.2009.52.5.607 [Google Scholar] [CrossRef]
[6]. Mohanty B, Deep vein thrombosis: A rare complication of varicella zoster infectionArch Gen Intern Med 2017 1(2):1-2. [Google Scholar]
[7]. Paul G, Paul BS, Singh G, Unseen face of varicella-zoster infection in adultsIndian J Crit Care Med 2016 20:731-34.10.4103/0972-5229.19571328149032 [Google Scholar] [CrossRef] [PubMed]
[8]. Minik CR, Fabricant CG, Fabricant J, Litrenta MM, Atherosclerosis induced by infection with herpes virusAm J Pathol 1979 96:673-706. [Google Scholar]
[9]. Gogos CA, Apostolidou E, Bassaris HP, Vagenakis AG, Three cases of varicella thrombophlebitis as a complication of varicella zoster virus infectionEur J Clin Microbiol Infect Dis 1993 12:43-45.10.1007/BF019970568462561 [Google Scholar] [CrossRef] [PubMed]
[10]. Andrew C, Nicholson Hajjar DP, Herpes viruses and thrombosis: Activation of coagulation on the endotheliumClinical Chimica Acta 1999 286:23-29.10.1016/S0009-8981(99)00091-1 [Google Scholar] [CrossRef]