Primary healthcare is an integral part of the overall socialeconomic development of the population [1]. Morbidity pattern at primary level care is of paramount importance in planning healthcare services in populations. This information facilitates program managers, decision makers, and policy planners for proper planning and adequate utilisation of scarce resources, subsequently, improvement in quality of health services [2]. India is in the transition phase of building its urban healthcare system as National Urban Health Mission as a part of National Health Mission [3]. Thus, data on morbidity pattern in urban slum will be helpful for policy planners and programme managers at local as well as national level.
Slums are defined as residential areas where dwellings are unfit for human habitation by reasons of dilapidation, overcrowding, faulty arrangements and design of such buildings, narrowness or faulty arrangement of street, lack of ventilation, light, or sanitation facilities or any such combination of these factors which are detrimental to the safety and health [4]. Limited opportunities in rural area and industrialisation result in large scale migration from rural to urban areas [5]. According to Census of India 2011, 17.4% households in urban areas are in slums [4]. In Chandigarh, slums constitute about 1/10th of total urban households. Population living in slums in Chandigarh is about 9.8% [6].
Poor living conditions in urban slums predispose the inhabitants to various communicable diseases [7]. On the other hand, the magnitude of NCDs is increasing due to unhealthy diet, lesser physical activity and increased prevalence of tobacco and alcohol consumption in such areas [8]. However, the exact burden of various diseases is not very well known. Therefore, the present study was planned to study the morbidity pattern at primary healthcare level in an urban slum of Chandigarh, India.
Materials and Methods
This cross-sectional study was a secondary data analysis of the patients those who attended Outpatient Department (OPD) of a Public Health Dispensary (PHD) in Chandigarh, India. PHD is a primary care level health facility attached with Department of Community Medicine, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh. It caters slum area with a population of approximately 30,000 as per the annual survey report, 2016 of the health facility. Majority of population are migrants from various states like Haryana, Punjab, Uttar Pradesh, Bihar, West Bengal, Tamil Nadu etc., [9]. PHD provides preventive, promotive and curative health care services to the community viz. health education, awareness campaign, immunisation, antenatal care, treatment of common diseases and minor injuries, and other services provided under various national health programmes.
Data about morbidity of patients who attended the OPD was collected as a part of routine healthcare services and were reported under national health programmes. In this study, the data were used from January to December 2016. Clinical diagnosis based on signs and symptoms of diseases was made by resident doctors from the Department of Community Medicine. In the OPD registers, separate entry was done for old and new cases attending the OPD. From the OPD register, morbidity of new patients was used to compile in monthly reports. In the monthly reports, the morbidity was further classified according to different organ systems like respiratory diseases, cardiovascular diseases, gastrointestinal diseases, skin diseases, musculoskeletal, urinary disorders, reproductive tract infections, vector borne diseases, eye and ear diseases, injuries, and other diseases which could not be categorised according to organ systems of the body.
Additionally, the diseases were categorised into CDs, NCDs, injuries and others for this study. CDs included gastrointestinal diseases (diarrhoea, dysentery, worm infestation, and acute peptic ulcer diseases), respiratory diseases (upper and lower respiratory tract diseases and tuberculosis), urinary tract infections, reproductive tract infections, conjunctivitis, ear diseases, skin diseases, dental caries and vector borne diseases (malaria, dengue, and chikungunya). NCDs included cardiovascular diseases mostly hypertension, diabetes, chronic obstructive pulmonary diseases, bronchial asthma, musculoskeletal diseases, constipation, cataract, epilepsy and psychiatric disorders. Injuries included minor injuries, burns and insect bites. “Others” included antenatal cases, nutritional disorders like anemia, malnutrition, and vitamin deficiency, symptoms like headache and weakness, and other diseases which could not be categorised into above mentioned groups [10-14].
Statistical Analysis
Data were entered in Microsoft Excel and analysed by using IBM SPSS Statistics for Windows, Version 16.0 (IBM Corp. Armonk, NY, USA). Descriptive statistics was used to present the results as frequency, percentage and proportions according to age groups, sex and disease groups. To determine the difference between proportions, the Chi-square test was used.
All information collected in the present study was a part of routine services existing in the PHD. For this study purpose, unique identifiers were removed from the data and all the information collected was kept confidential. This study was a secondary data analysis, hence, ethical approval was not obtained. However, the prior permission to use data was obtained from the appropriate authority for the PHD.
Results
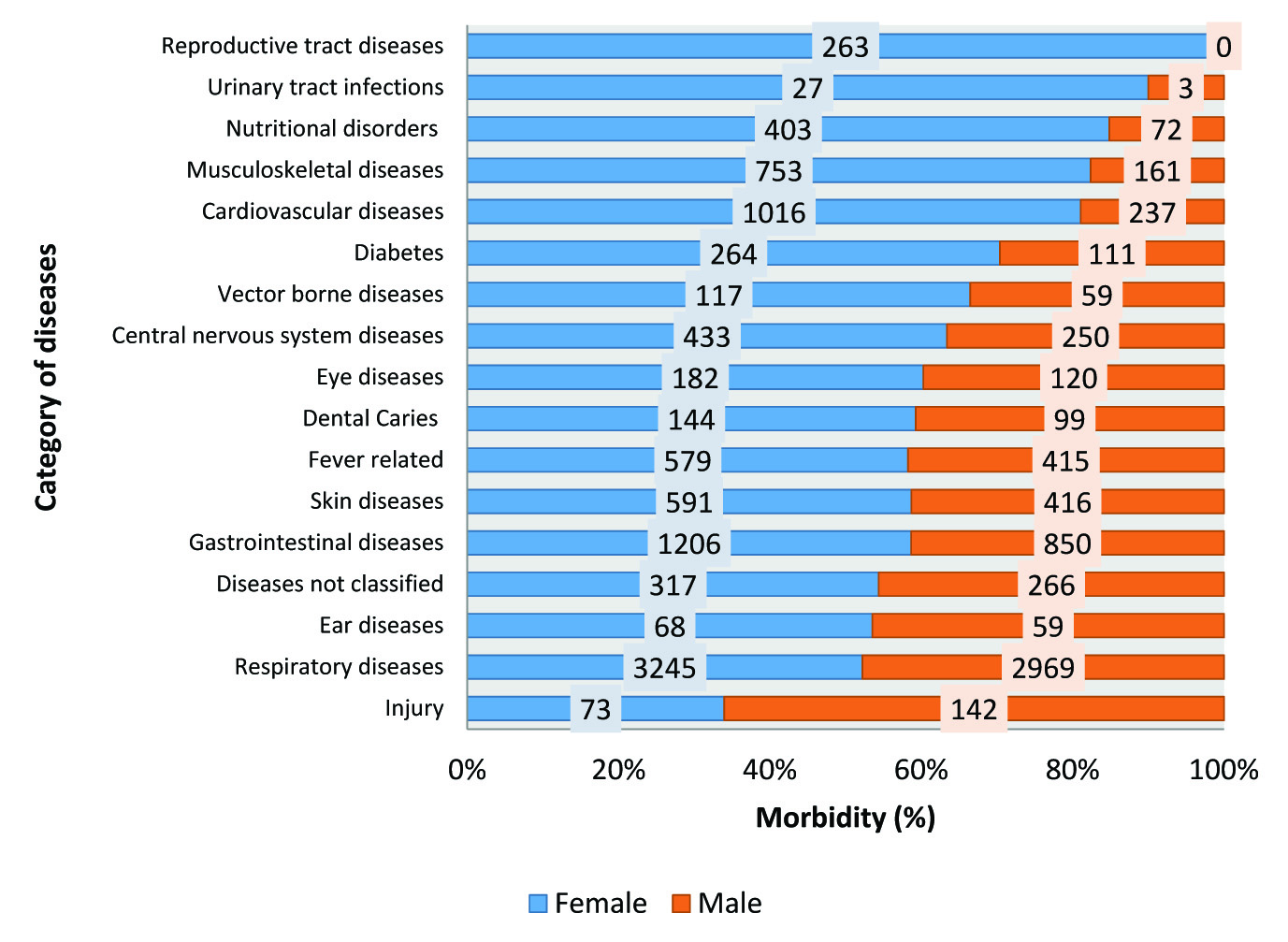
A total of 14,153 patients attended the outpatient department of PHD, Chandigarh during 2016. These patients had 16,483 morbidity, as some patients suffered from multiple problems. Of the total 16,483 cases morbidity, 62.2% were in females. Morbidity distribution was variable between males and females [Table/Fig-1]. Highest morbidity was reported from age groups under 15 years (5826, 35%) and 15-44 years (5678, 34%).
Distribution of morbidity in a primary care facility by age and sex, 2016.
| S. No. | Age group (years) | Morbidity in males n (%) | Morbidity in females n (%) | Total n (%) |
|---|
| 1 | 0-4 | 1232 (46.8) | 1400 (53.2) | 2632 (100) |
| 2 | 5-14 | 1431 (44.8) | 1763 (55.2) | 3194 (100) |
| 3 | 15-44 | 1645 (29) | 4033 (71) | 5678 (100) |
| 4 | 45-64 | 1248 (36.6) | 2164 (63.4) | 3412 (100) |
| 5 | ≥65 | 673 (42.9) | 894 (57.1) | 1567 (100) |
| Total | 6229 (37.8) | 10254 (62.2) | 16483 (100) |
Chi-square - 365.6, p-value <0.001
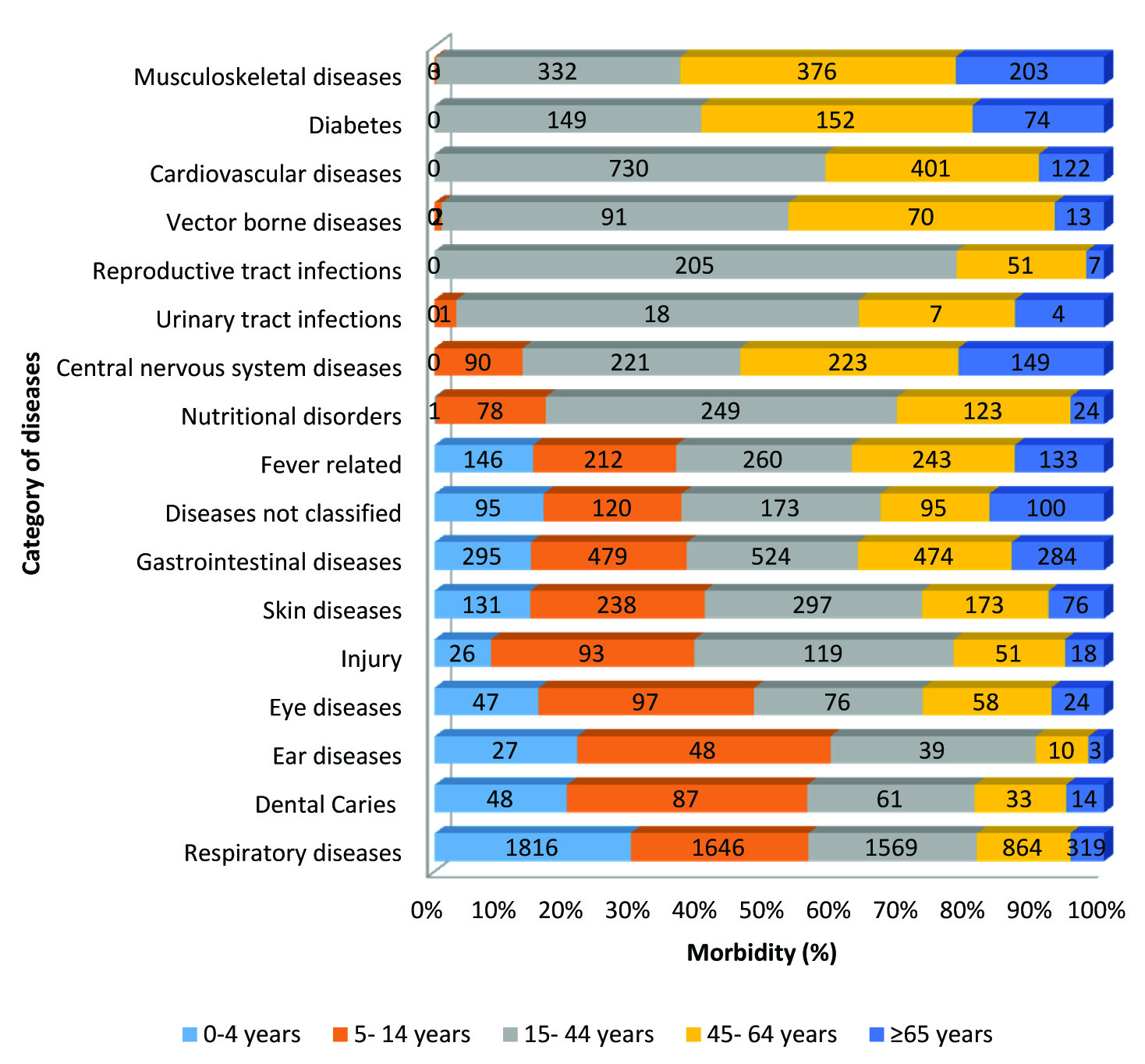
Most common morbidity in this primary healthcare facility was respiratory diseases (n=6214) followed by gastrointestinal diseases (n=2056), cardiovascular diseases (n=1253) mostly hypertension, and skin diseases. Respiratory diseases (1816, 29.2%) were highest in children aged 0-4 years with almost equal distribution in both the sexes. Dental caries, eye and ear diseases were highest in the age group 5-14 years with female preponderance. Urinary and reproductive tract infections (18, 60% and 205, 77.9%, respectively) were more common in reproductive age females (15-44 years). Antenatal care (n=573) contributed to 3.5% of the total morbidity. The cardiovascular diseases mostly hypertension (n=730 and 401) and diabetes (n=149 and 152) were common in both the age groups 15-44 years and 45-64 years respectively for both males and females. Musculoskeletal diseases were highest in 45-64 years (n=376) and more common in females. Vector borne diseases were more common in 15-44 years (n=91) followed by 45-64 years (n=70). Males have higher morbidity (n=142) due to injuries than females (n=73) [Table/Fig-2,3].
Distribution of morbidity by organ systems and sexes, 2016.
Antenatal females visiting the primary health centre are not included.
Distribution of morbidity by organ systems and age groups, 2016.
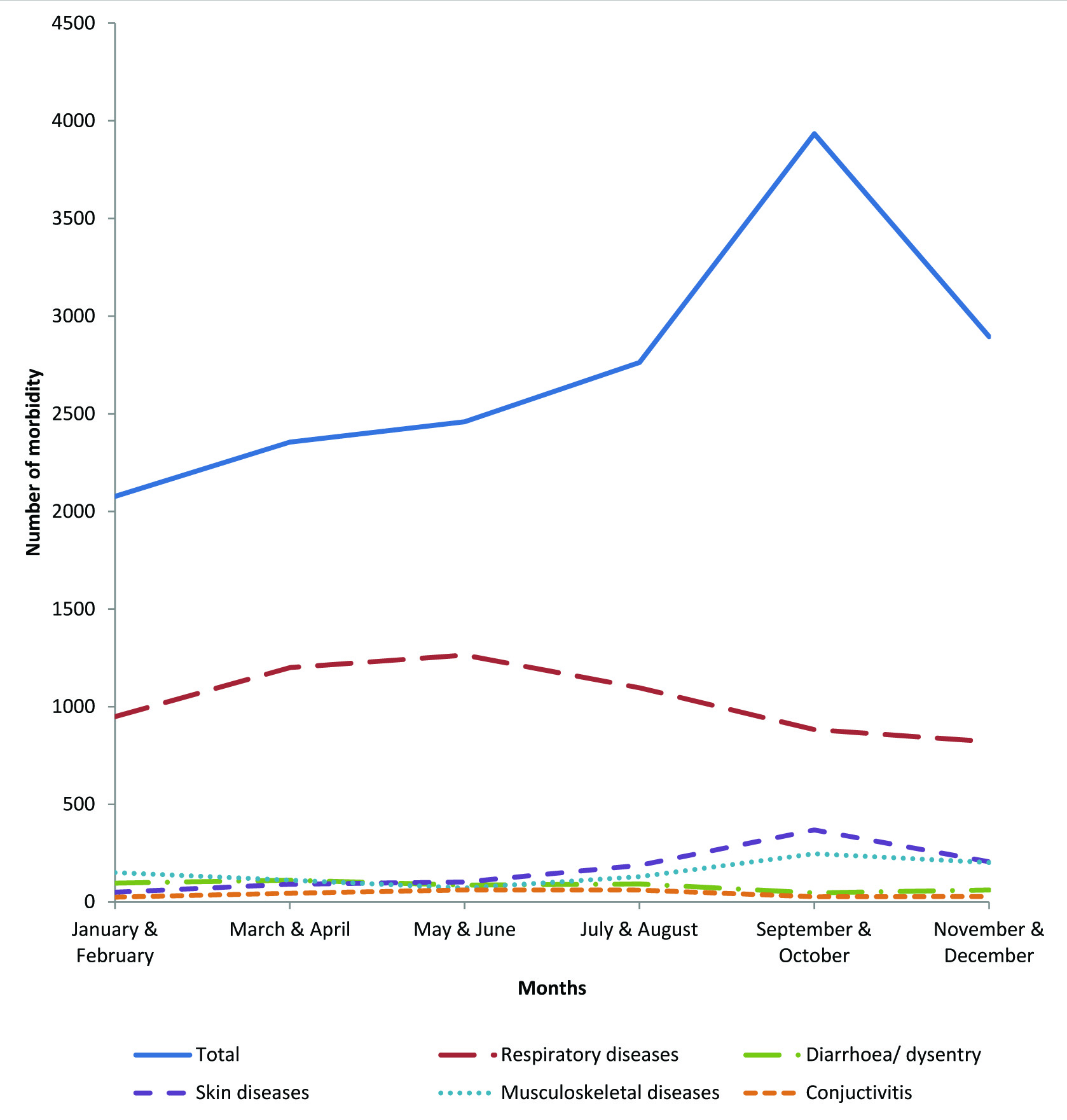
Seasonal pattern of morbidity revealed an increasing trend in the month of May to October season with a peak in September. Respiratory diseases were higher from March to June. Diarrhoea and dysentery was higher in March and July and gradually decreased thereafter. Conjunctivitis cases were reported maximum in July and least in November to January. Skin diseases were highest in the month of July to December. Musculoskeletal diseases were higher in the months of September to December [Table/Fig-4].
Seasonal pattern of morbidity in a primary level care by major disease groups, 2016.
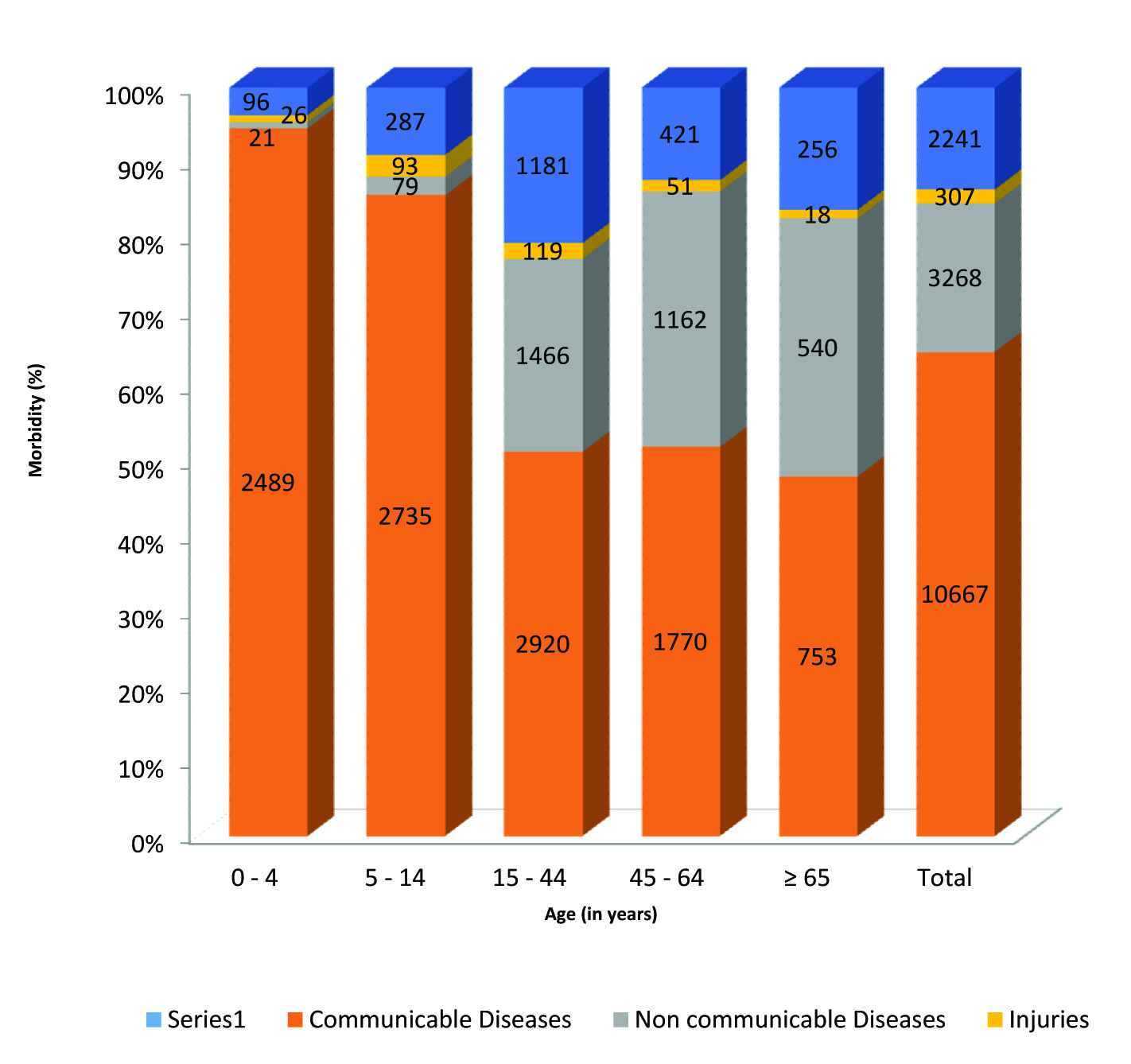
Of the total, 64.7% (n=10667) morbidity was due to communicable diseases, 19.8% (n=3268) due to NCDs, 1.9% (n=307) due to injury, and 13.6% (n=2241) due to nutritional disorders, antenatal care, and symptoms based morbidity which could not be classified. Most common CD was upper-and lower-respiratory tract diseases (6214, 37.7%), followed by gastrointestinal diseases (2056, 12.5%). Most common NCD was hypertension (1078, 6.5%) followed by musculoskeletal pain (914, 5.5%). Morbidity due to CD was highest in children. With increasing age, the proportion of morbidity due to communicable diseases decreased while morbidity due to NCDs increased. In under five children, 94.6% (n=2489) morbidity was due to CDs, while in 65 years and older, CDs contributed 48.1% (n=753) of the morbidity. NCDs caused one third of the morbidity in the age group ≥45 year patients. Injuries were most common among 5-14 years age group followed by 15-44 years [Table/Fig-5].
Distribution of diseases categories in different age groups.
Discussion
This study presented the spectrum of health problems of slum dwellers attending OPD of a primary healthcare facility in a fast-growing city of North India. Largely, the magnitude of morbidity in females outweighed that of the males in an urban primary healthcare facility. Communicable diseases constituted approximately two third of the morbidity, and children under the age of five were the most affected age group (more than 90%). NCDs contributed one-fifth of the morbidity.
Higher female morbidity in our study may be due to higher participation of female patients attending OPD. Our study findings were in conformity with Yadav V et al., [15]. Females, largely being non earning members therefore staying at home, find services at a local primary healthcare facility affordable and accessible. As male members usually go in the day time for earning a livelihood; hence, they may not find convenient time to avail these facilities. Male patients usually do not depend on others to consult at secondary level or other private hospitals where more services are available. This pattern became more evident when we explore distribution of morbidity by sex and age groups. Distribution of morbidity was not much affected by sex in younger ages (under 15 years: males - 45.7%, females - 54.3%). However, the sex differential was observed in adults (15-64 years: males-31.8%, females-68.2%).
The pattern of common morbidity in our study was similar to that reported by other studies at primary care level [16-19]. Highest proportion of respiratory morbidity in slum area might be due to overcrowding, traffic-related, household air pollution, tobacco and second-hand smoke, occupational exposures, and allergenic sensitisation [20]. High reproductive and urinary tract infections in 15-44 years females is in coherence with findings of Kumari R et al., [21]. Biological factors (for e.g., short urethra and more exposed area in females), lack of personal hygiene, female illiteracy, and gender disadvantage particularly spousal violence were common explanations for higher reproductive tract infections burden in females [22]. In injuries, male predominance was apparent despite lower male attendance in the facility. This pattern is evident in Global Burden of Disease and Million Death Study [23,24]. Again, this finding might be linked to more outdoor exposure and livelihood related activities, and more exposure to road traffic. Musculoskeletal disorders were higher in females that may be explained by their posture during routine household work and osteoporosis after menopause. Woolf AD et al., also reported higher prevalence of musculoskeletal conditions among females [25]. Age group of 15-64 years was more affected with vector borne diseases might be due to more outdoor activities of this age group.
We found an increasing trend from May to October season with a peak in September. Along with seasonal change in epidemiology of diseases, availability of medicine in health facility and number of holidays (festival season when migrant population prefer to go to their native place) in a month may also play an important role in seasonal pattern of morbidity at primary level care. Seasonal pattern of morbidity showed a peak in September mainly because of outbreak of vector borne diseases in the region. A synchronised peak in September was also observed for skin and musculoskeletal diseases due to more number of cases of joint pain and pruritus associated with this outbreak of dengue and chikungunya in Chandigarh [26]. We observed relatively high number of cases with musculoskeletal diseases in winter. This may be associated with cold exposure in winter season [27]. Conjunctivitis showed seasonal pattern with abundance in summer and rainy seasons which corroborate the findings of Sharma S et al., [16].
Low proportion of nutritional disorders (2.9%) was revealed in this study as compared to National Family Health Survey (NFHS-4). According to NFHS-4, about one-fourth children under the age of five years were underweight and more than 70% females of reproductive age group and children were anaemic in Chandigarh [28]. It points towards underdiagnosed cases or not writing nutritional disorders in diagnosis by doctors. It may be due to a missed opportunity, as patients mostly consult the health facilities due to some other reasons and only fewer patients reported to health facility because of symptoms due to nutritional disorders.
Higher morbidity burden due to CDs may be indicative of poor living conditions in urban slums where environment is favorable to the growth of micro organism and vectors. Higher burden of CD was observed in children. This is in concurrence with studies by Sharma S et al., and Gupta A et al., [16,17]. This may be explained by lower immunity in children as innate and adaptive immune systems are still maturing in them [29]. Proportion of morbidity due to NCDs in our study was 19.8 %, similar to that reported by Kumari R et al., [21]. Although, no national data on proportion of morbidity due to NCDs is available, few studies undertaken at primary care level described 10-35% of morbidity is attributed by NCDs [16,21,30]. At national or global level burden of diseases due to NCDs was described in terms of proportion of deaths due to NCDs [31]. Lower proportion of morbidity due to NCDs in this study might be due to limited diagnostic and treatment facilities related to NCDs at primary care level (limited diagnostics and medication of hypertension and diabetes were available, that too intermittently in the facility). It might also be reflection of lesser NCDs burden in the community as compared to CDs in the urban slum.
Limitation
This was a health centre based cross-sectional study and may not represent actual burden of community. Results may be inclined towards over representation of the females; although, it is common for such kind of primary care facilities in urban slums. In this study, the diagnosis of diseases was based on clinical judgment only because of limited resources at primary healthcare facility. These results should be generalised cautiously as the data were collected from a single health facility.
Conclusion
Our study concludes that there is still preponderance of CDs among slum dwellers with higher attendance of females in primary care settings. Although morbidity pattern of outpatients at urban primary care facility depends on various factors, it is essential for program managers and policy makers to plan and manage health care services at primary care level. These findings emphasize the need of further research and more attention on the distribution of morbidity and associated social determinant of health in vulnerable populations.
Chi-square - 365.6, p-value <0.001