Sudden death is defined by World Health Organization (WHO) as death within 24 hours from the onset of symptoms. Young south Asians make up approximately 60% of the world’s Coronary Artery Disease (CAD) load. India being a developing country is the CAD capital of the world according to WHO [1,2]. In contrast to the extensive study done on the pattern and prevalence of SD in western countries, this topic has been fairly untouched in the south Asian societies. It is partly due to a lack of systematic record acquisition, non uniform billing codes, varied payment strategies, absence of reporting and a social aversion to autopsy [3-6]. The present study was taken up as a means to shed light on the rate, pattern and underlying pathology of SD so as to promote strategies for prevention and therapy for the SD in this part of Indian population.
Materials and Methods
This was a retrospective cross-sectional study was conducted in Sri Devaraj Urs Medical College, Karnataka, India. The ethical clearance was obtained from Institutional Ethical Clearance Committee before starting the study. All autopsy cases of SD from 1 July 2012 to 30 June 2017 were collected from the archives of Pathology, Forensic Medicine and Toxicology Department. The sociodemographic data of the cases such as the age, gender, autopsy findings and cause of death were noted. Cases were considered to have SD, if they died at home or were found dead out of the hospital without a known cause and who were brought to the casualty for evaluation of cause of death. All study cases were known to have died within 24 hours of the onset of symptoms and presentation to the casualty. Patients with trauma, intoxication, poisoning and violent deaths were excluded from the study.
Autopsy methodology was in accordance to the routine procedure followed in the pathology department. Grossing of the heart, lungs, liver, spleen, kidneys were done by conventional method. The histomorphological findings from tissue sections of tissue bits from the representative areas were noted and analysed.
Atheromatous changes of the aorta and coronary arteries were graded based on the AHA 2011 criteria as; Grade 1: Initial lesion with isolated macrophages and foam cells, Grade 2: Fatty streak lesion with intracellular lipid accumulation, Grade 3: Grade 2 changes with small extracellular lipid pools, Grade 4: Atheroma lesion with Grade 2 changes and core of extracellular lipid, Grade 5: Fibroatheroma lesion with lipid core and fibrous cap, Grade 6: Complicated lesion with surface defect, haematoma, haemorrhage, and thrombus [7].
Cardiac abnormalities when found were considered to be Sudden Cardiac Death (SCD). Patients with non-cardiac pathology were considered to have non cardiac causes of SD. Absence of cardiac or non cardiac pathological findings indicated non structural causes of SD.
Statistical Analysis
The patient details along with gross and histomorphological findings were entered in Excel sheet. The descriptive statistical analysis was done. Results were expressed as percentages.
Results
During the five year study, out of 1467 autopsy cases, 11 (0.74%) cases underwent autopsy for SD. About 10 (91%) out of 11 cases were males. The age range was 28 to 78 years with mean age of 44.36 years (standard deviation=4.35, standard error=4.34) [Table/Fig-1]. In 9 (81%) cases SD was attributed to cardiac causes. Only 1 (9.09%) case had a non cardiac cause of SD attributed to hepatic cause i.e., steatohepatitis. In one (9.09%) case, there was no demonstrable cardiac or non cardiac pathology and hence it was categorised as non structural cause of SD. Out of the nine cardiac cases, atheromatous plaque in aorta and coronary arteries were seen in 5 (55.55%) cases ranging from AHA Grade 2 to Grade 5. Myocardial infarction was seen in 2 (22.22%) out of 9 cases. Intraventricular antemortem thrombus was seen in 3 (33.33%) out of 9 cases. One case had both thrombus as well as atheromatous plaque. The gross and histomorphology is shown in [Table/Fig-2,3,4,5,6,7 and 8]. The distribution of atheromatous plaque in AHA grades and percentage of obstruction in aorta, right/left coronary artery and anterior descending artery are shown in [Table/Fig-9]. Out of 9 cardiac cases, pulmonary congestion was seen in 2 (22.22%) cases and pulmonary oedema was seen in 3 (33.33%) cases.
Shows the age/sex distribution with cause and specific lesions of sudden death cases of present study.
| Cases | Age (years) | Sex | Cause of sudden death | Lesion |
|---|
| 1 | 28 | M | Sudden cardiac death | Antemortem thrombus in right ventricle |
| 2 | 29 | M | Sudden cardiac death | Grade 2 atheroma in right and left coronary arteries. Pulmonary congestion |
| 3 | 35 | M | Sudden cardiac death | Grade 4 atheroma in aorta. Grade 5 atheroma in right and left coronary arteries. Pulmonary oedema |
| 4 | 35 | M | Liver disease | Steatohepatitis |
| 5 | 40 | M | Sudden cardiac death | Myocardial infarction in left ventricle. Pulmonary congestion. |
| 6 | 42 | M | Non-structural | No structural abnormality |
| 7 | 42 | M | Sudden cardiac death | Grade 1 atheroma in aorta. Grade 3 atheroma in right and left coronary arteries. |
| 8 | 50 | M | Sudden cardiac death | Grade 5 atheroma in left coronary artery. Pulmonary oedema. |
| 9 | 54 | M | Sudden cardiac death | Antemortem thrombus in right ventricle.Grade 4 atheroma in aorta. Grade 5 atheroma in RCA. Grade 3 atheroma in LAD. Pulmonary oedema |
| 10 | 55 | M | Sudden cardiac death | Antemortem thrombus in left ventricle |
| 11 | 78 | F | Sudden cardiac death | Myocardial Infarction in right ventricle |
| Mean = 44.36 | M:F=10:1 | | |
M: Male, F: Female
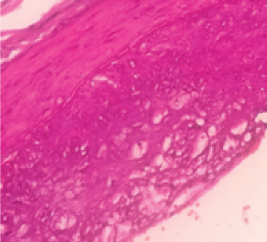
Microphotograph showing grade 2 atheroma in left coronary artery (H&E, 10X).
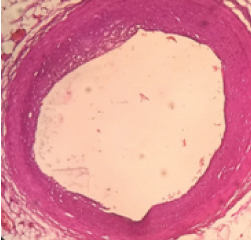
Microphotograph showing grade 2 atheroma in left coronary artery (H&E, 40X).
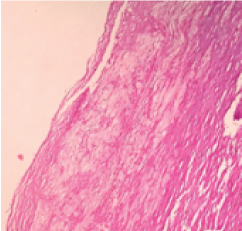
Microphotograph showing grade 3 atheroma in aorta (H&E, 40X).
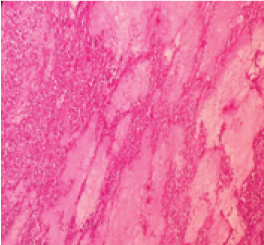
Microphotograph showing grade 5 atheroma in right coronary artery (H&E, 10X).

Gross photograph showing antemortem thrombus in the right ventricle.

Microphotograph of antemortem thrombus in right ventricle (H&E, 40X).
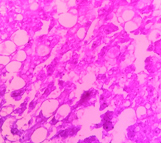
Microphotograph showing features of steatohepatitis (H&E, 40X).
Shows distribution of atheromatous plaque in aorta/coronary arteries with histological grade and percentage of obstruction.
| Location of atheromatous plaque | Histological grade in numbers | Gross obstruction in percentage | Total number of atheromatous plaques (out of 5) |
|---|
| Aorta | Grade 1=1 | 0% | 3 |
| Grade 4=2 | 25% |
| 25% |
| Left coronary artery | Grade 2=1 | 05% | 3 |
| Grade 3=1 | 20% |
| Grade 5=1 | 80% |
| Right coronary artery | Grade 2=1 | 05% | 3 |
| Grade 3=1 | 25% |
| Grade 5=1 | 75% |
| Left anterior descending artery | Grade 3=1 | 25% | 1 |
Discussion
In recent years India has shown an increase in the incidence of SD which is due to increase in CAD deaths [6]. This is attributed to an increase in westernisation and a changing lifestyle leading to an increase in comorbidities [2,3,5-9]. Sheppard M and Davies MJ, suggested sequential autopsy examination in the evaluation of SD as; the first step is considering a natural cause of death followed by excluding non cardiac natural death. The next step is to consider gross and microscopic findings in the heart and other organs. These findings were correlated with history and toxicological results to derive final conclusion and cause of SD [10].
The SCD has a bimodal peak of incidence. The first peak being less than six months of age as seen in Sudden Infant Death Syndrome (SIDS) and the second peak being between 45 and 75 years of age [11-21]. The present study has a mean age of 44 years. The studies by Srivatsa U et al., and Pandian J et al., reported a mean age group of 50 years and 40 years respectively [2,6].
The present study had 11 (0.7%) cases of SD out of 1467 autopsy cases. Madhavan SR et al., found 309 (17%) cases of SD out of 1827 autopsies over two years and Pandian J et al., had 120 (8.61%) cases of SD of a total of 1034 autopsies performed over a period of 13 years [4,6]. In the present study, we had low prevalence of SD probably because of less awareness and knowledge of autopsy in the local population as most (approximately 75%) of present patients come from rural areas who are illiterate.
Most of the studies have a male preponderance of SD as studies by Srivatsa U et al., had 3.47:1, Madhavan SR et al., had 1.61:1 and Pandian J et al., had a male to female ratio (M:F ratio) of 6.5:1 [2,4,6]. The present study had a similar M:F ratio of 10:1. Increased prevalence in males may be due to increased rate of cardiovascular pathology in males.
As seen in most of the studies, the major contributors of SDs are the cardiac causes followed by pulmonary diseases, hepatobiliary diseases, neurological diseases and finally gastrointestinal diseases. The major cardiovascular diseases which lead to an increased risk of SDs are as follows in decreasing order; CAD, electrophysiological abnormalities, cardiomyopathies and valvular heart disease [10-15].
Cardiac cause of SD can be classified as CAD, cardiomyopathies and valvular heart disease. The cardiomyopathies can be idiopathic dilated cardiomyopathy, hypertrophic cardiomyopathy or arrythmogenic right ventricular dysplasia. The most common valvular heart disease resulting in SD death is aortic stenosis [21].
From the 11 autopsied cases of SD in the present study, 9 deaths (81.81%) were due to cardiovascular pathology. CAD was found to be the most common cardiac cause of SD (55.55%). These results were similar to the study conducted by Pandian J et al., and Farb A et al., which were 53.7% and 57% respectively [6,13]. Majority of the cases were male with the mean age of 44 years. Contrastingly Pandian J et al., had a lower age group of 30-40 years. However, the finding in our study was similar to that of Madhavan SR et al., who had a mean age of 45 years [4]. Atheromatous changes were the most common finding in the present study followed by intraventricular thrombus. Atheromatous plaques coupled with obstruction causes SD due to sudden alteration in the plaque probably with emotional or physical stress [2-13,22].
The most common cause of pulmonary disease leading to SD is pulmonary embolism and pulmonary congestion. Other causes include pulmonary hypertension, pulmonary obstruction, pneumonia and rarely tuberculosis [2,3,4,5]. Pandian J et al., attributed 16.67% of SDs to pulmonary diseases [6]. The present study did not have any case specifically attributing to pulmonary cause of SD; however, we had pulmonary pathology as pulmonary oedema and congestion which are secondary (comorbid factors) to cardiac pathology.
Liver and gastrointestinal diseases leading to SD include severe hepatic steatosis and severe peptic ulcers. This leads to complications such as massive gastrointestinal bleeding and perforation [2,9-12,17-21]. Pandian J et al., reported 13.3% hepatobiliary related SDs [6]. The present study also had a similar finding of 1 (9.09%) case of severe steatohepatitis. The mechanism of death in these cases remains obscure. One study has reported 11 cases of steatohepatitis as cause of SD stating that the patients had severe electrolyte disturbances especially hypomagnesaemia. It was concluded that various metabolic disturbances triggered by the combination of massive ethanol intake and starvation was the most probable cause of these deaths in steatohepatitis [23,24].
Cerebrovascular accidents are the main cause of SD due to neurological diseases. In contrast to Pandian J et al., who reported an incidence of 3.33%, present study had no neurological aetiology for SD [2-6].
Patients without any underlying structural disease are usually strikingly younger approximately 40 years old. About 80% of non structural SDs are attributed to ventricular fibrillation [9]. Srivatsa U et al., reported non structural SDs in 8.2% cases [2]. The present study reported this entity in 1 (18.3%) case. Other causes of non structural SDs are long QT syndrome, Brugada syndrome, short QT syndrome, catecholaminergic polymorphic ventricular tachycardia [2-9].
Limitation
The main limitation of this study was that the study was retrospective and has small number of cases. This is partly due to social stigma and religious views associated with autopsy. Since, this was a retrospective study, the details of the smoking habits, tobacco chewing habits, alcohol consumption and medical history could not be elicited. As our hospital is situated in a rural area, many of our patients are illiterate and are therefore unaware of the importance of an autopsy. Hence, large number of SDs goes unreported. However, the important data deduced from this study as high prevalence of cardiac diseases which were giving rise to SD. This is especially predominant in young male adults in their prime of productivity and therefore needs special attention for a change in lifestyle and knowledge about preventive measures.
Conclusion
In this study, we found that majority of SDs occurred in young male adults, posing a health concern in our society. Cardiac causes contributed the maximum number and atherosclerosis being the main culprit in causing CAD. Awareness regarding preventive measures and affordable interventions should be made available by the health authorities.
M: Male, F: Female