Pitfalls in Diagnosing Seropositive Rheumatoid Arthritis: Haematologic Malignancy Presenting as an Autoimmune Disease
Bijit Kumar Kundu1, Eashan Srivastava2, Vijesh Vijayan3, B Manojprabhakaran4, Mukesh Verma5
1 Associate Professor, Department of Medicine, PGIMER, Dr RML Hospital, New Delhi, Delhi, India.
2 Resident, Department of Medicine, LHMC and Associated Hospitals, New Delhi, Delhi, India.
3 Resident, Department of Medicine, LHMC and Associated Hospitals, New Delhi, Delhi, India.
4 Resident, Department of Medicine, PGIMER, Dr RML Hospital, New Delhi, Delhi, India.
5 Resident, Department of Medicine, LHMC and Associated Hospitals, New Delhi, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Eashan Srivastava, D-62, Pushpanjali Enclave Pitampura, New Delhi-110034, Delhi, India.
E-mail: eashan.srivastava@gmail.com
Carcinomatous Polyarthritis (CP) is defined as the development of arthritis in association with a malignancy but distinct from that associated with metastasis or direct invasion. It can occur before, with, or after onset of malignancy or with treatment. CP usually affects large joints and is negative for Anti Citrullinated Protein Antibodies (ACPA). CP is rarely if ever considered in the differential diagnosis of a case of symmetric polyarthritis with ACPA positivity. Presence of autoimmune disease related antibodies further obscures the diagnosis. We present a case of a young lady with symmetrical inflammatory polyarthritis with positive ACPA who was found to have haematological malignancy. This is one of the very few cases of CP of small joints with ACPA positivity reported worldwide and highlights the need to be vigilant for red flags while evaluating any case presenting with rheumatologic symptoms.
Autoantibodies, Cyclic citrullinated peptide, Globulins, Leukaemia, Neoplasms, Rheumatoid factor
Case Report
A 24-year-old lady presented to the Rheumatology clinic of a tertiary care hospital with complaints of painful swelling of small joints of bilateral upper limbs, knees and ankles associated with early morning stiffness lasting more than half an hour for almost six months. This was associated with a feverish feeling which was intermittent, and without chills and rigors. However, there was no documented fever. Initial fever workup done by the treating physician on OPD basis was unremarkable. With time, the shoulders and elbows also were affected. Past medical, family, personal and social history were insignificant. Her blood counts, liver and renal function tests were within normal limits [Table/Fig-1]. However, she was found to be positive for ACPA in high titers (375 IU/mL, normal <5 IU/mL) though the Rheumatoid Factor (RF) was negative. She was diagnosed as Rheumatoid Arthritis (RA) and started on daily tablet hydroxychloroquine 200 mg twice daily and tablet diclofenac 50 mg on demand. She did not show any improvement even after three months. Later on she developed shortness of breath on exertion for which she was evaluated and revealed to have anaemia and thrombocytopenia for which she had been referred to our centre. General and systemic examination revealed severe pallor, pericardial rub, flow murmurs over the heart and hepatosplenomegaly. Musculoskeletal examination revealed synovitis of wrists, metacarpophalangeal, proximal interphalangeal, elbows and ankle joints. She was admitted as a case of connective tissue disorder probably Systemic Lupus Erythematosus (SLE) based on presence of polyarthritis, anaemia and pericardial rub and for further evaluation in this regard. Laboratory results revealed anaemia, leukocytosis, thrombocytopenia [Table/Fig-1]. Erythrocyte Sedimentation Rate (ESR) was 30 mm in first hour (normal range 0-20 mm in first hour for females by Westergrens method). Antinuclear Antibody (ANA) and RF were negative. ACPA was in high titers. Rest of the biochemical parameters such as renal function tests, liver function tests, electrolytes, thyroid function tests were normal. Her urine routine and microscopic examination was normal. Echocardiograph of the heart did not reveal any abnormality. Culture of blood and urine remained sterile after 72 hours. Tests for malarial antigen, Kala Azar (recombinant K39 antigen) and serological markers for human immunodeficiency virus, hepatitis B virus and hepatitis C virus as well as Mantoux test turned out to be negative. Her chest radiograph was within normal limits. Radiographs of both hands were normal with no joint space narrowing or erosions. However, her peripheral smear revealed presence of atypical cells, with blastoid morphology having large pleomorphic, folded and lobulated nuclei, constituting 25% of the cell count. A bone marrow aspiration showed 44% blasts which were 2-3 times the size of small mature lymphocyte, with moderate granular cytoplasm with Auer rods. The cells stained strongly with myeloperoxidase and were suggestive of promyelocytic blast cells [Table/Fig-2,3]. A diagnosis of Acute Promyelocytic Leukaemia (APML) was made. In view of the anaemia, she was transfused with 2 units of packed red blood cells and then referred to a specialised oncology center for further evaluation and management where she succumbed to her illness.
Various investigations in the case done at different points of time.
| Investigations | Investigation with Primary Care Physician | Investigations at the time of referring to the hospital | Investigations in our hospital at presentation |
|---|
| Haemoglobin (gm/dL) | 10.8 | 5.6 | 3.2 |
| Total leukocyte count (cells × 109/L) | 6.8 | 12.7 | 38.6 |
| Differential count (percent) | Polymorphs 66% Lymphocyte 34% | Polymorphs 68% Lymphocyte 32% | Polymorphs 40% Lymphocyte 56% Eosinophil 4% |
| Platelet count (cells × 109/L) | 150 | 100 | 40 |
| Urea (mg/dL) | 28 | 45 | 36 |
| Creatinine (mg/dL) | 0.9 | 0.8 | 0.8 |
| Total bilirubin (mg/dL) | 0.3 | Not available | 1.3 |
| Aspartate aminotransferase (IU/L) | 41 | Not available | 32 |
| Alanine aminotransferase (IU/L) | 24 | Not available | 28 |
| Alkaline phosphatase (IU/L) | 147 | Not available | 152 |
| Total serum protein (gm/dL) | 5.8 | Not available | 5.9 |
| Serum albumin (gm/dL) | 2.9 | Not available | 2.4 |
| Typhidot IgM | Negative | Not available | Negative |
| Malaria antigen | Negative | Not available | Negative |
| Widal | Negative | Not available | Negative |
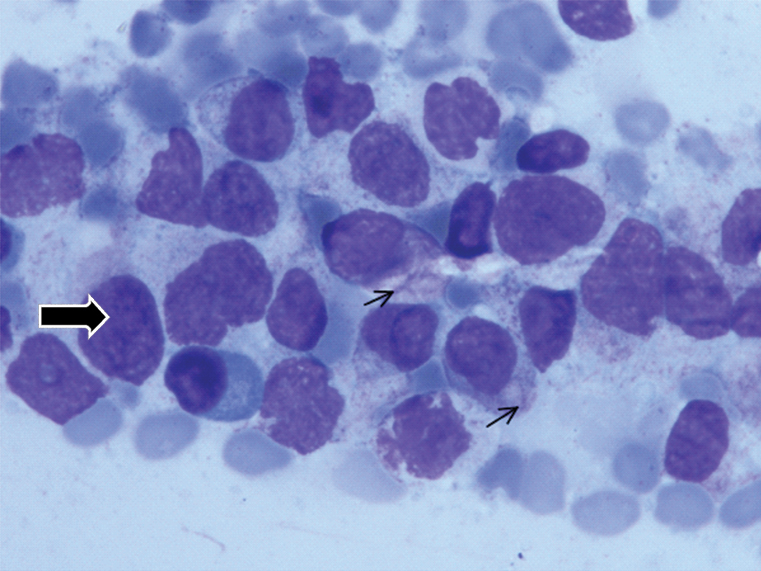
Light microscopy picture of Bone Marrow Aspirate showing blasts (black arrow) which were two to three times the size of small mature lymphocyte, with moderate granular cytoplasm with Auer rods (thin arrow), Giemsa stain (100X).
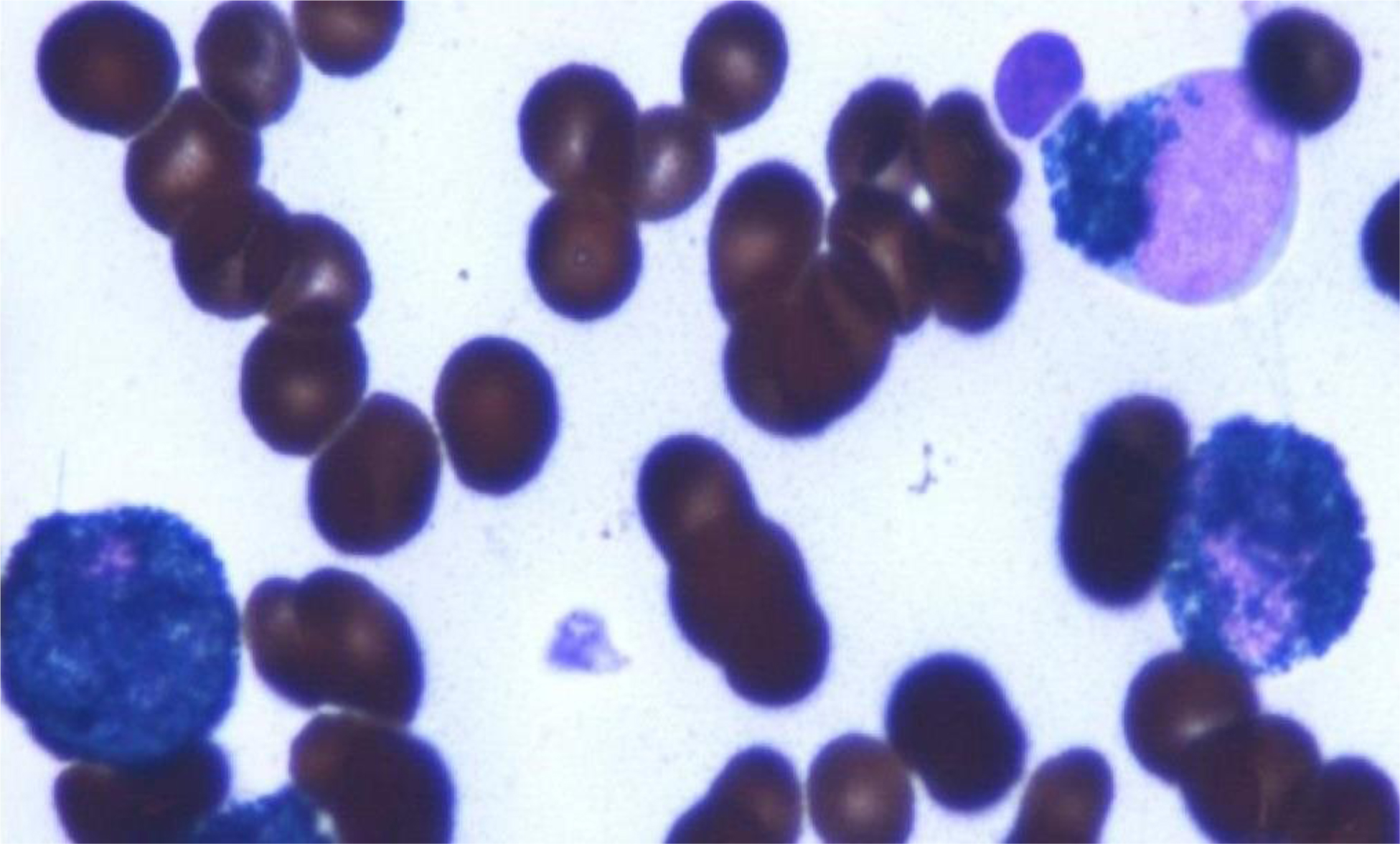
Light microscopy picture of Bone Marrow Aspirate showing Blasts with granular cytoplasm showing intense staining with Myeloperoxidase stain (100X).
Discussion
Carcinomatous polyarthritis is used to describe development of arthritis in association with malignancy. Commonly it is explosive, has a temporal relation with onset of malignancy, asymmetrical, predominantly lower limb, and spares the small joints of the hand [1], though a symmetrical small joint polyarthritis, in pattern of classical RA has also been described [2,3]. However, these are mostly sero negative for ACPA. Polyarthritis can also be a manifestation of malignancies especially haematological malignancies, which are included in the differential diagnosis of polyarthritis. Rheumatic manifestations can be found in over 60% of cases of leukaemia, lymphoma and myelomas. They can also be associated with RF and ANA but usually lacks ACPA [4]. They may precede the diagnosis, occur during the disease or even be a complication of treatment [5]. The association of Immune Checkpoint Inhibitors (ICIs) used in treatment of malignancies with different rheumatologic entities has recently come into focus [6].
Recently however, few cases of malignancies presenting as RA like polyarthritis with ACPA positivity have been described, though their number remains in single digits. Handy CE et al., described three cases of such presentation [7]. Few other cases have been reported subsequently. One out of the two cases reported by Watson G et al., showed a case of breast malignancy which presented as oligoarthritis and ACPA positivity [8]. The case reported by Edavalath S et al., was that of a polyarthritis of RA pattern with ACPA positivity as presentation of multiple myeloma [9].
Our patient had symmetrical polyarthritis with early morning stiffness, anaemia, high titres of ACPA, no response to disease modifying anti rheumatic drugs (hydroxychloroquine) therapy and underlying promyelocytic leukaemia. The RA pattern along with the ACPA positivity which is the most specific marker of RA led to the initial diagnosis of RA. The red flag in our case were anaemia and fever and only when these were evaluated, was the underlying malignancy revealed. Also of interest is the presence of pericarditis evidenced by presence of a rub which prompted diagnosis of SLE initially. Pericarditis is a rare presentation of acute leukaemia with the very few cases reported in literature. This adds to the rarity of our case [10,11]. It needs to be mentioned that though specificity of ACPA is highest for RA, it is not only found in other rheumatologic disorders like psoriatic arthritis, SLE, juvenile idiopathic arthritis, systemic sclerosis, but also in infections like hepatitis B, and tuberculosis [12]. We predict that in future malignancy will also be added to the above list as clinicians become more sensitive and more cases similar to ours come to light. To the best of our knowledge, we are reporting only the sixth case of ACPA positivity in a malignancy with carcinomatous polyarthritis as its presentation. It also highlights the need to be vigilant about the well-known rheumatologic red flags even in cases where the diagnosis seems obvious clinically as well as serologically as lack of response to treatment may be the first indicator of an underlying malignancy thus providing an opportunity for earlier diagnosis and treatment of the underlying malignancy, which is also the treatment of CP [13,14].
Conclusion
We conclude that the clinician should be vigilant about the red flags when seeing any case with rheumatologic symptoms even though the serology may be consistent with the rheumatologic diagnosis. Red flags may develop subsequently and may be the only indicator of an underlying malignancy, as has been in our case. It is also imperative to keep in mind the response to treatment of a rheumatologic entity as lack of response may indicate an entity different from the original diagnosis. This assumes importance in the light of the fact that treatment of CP is the treatment of the underlying malignancy.
[1]. Chakravarty EF, Muskuloskeletal Syndromes in malignancy. In: Firestein GS, Budd RC, Gabriel SE, McInnes IB and O’Dell JR,(Editors)Kelly’s Textbook of Rheumatology 2013 Vol.29th edPhiladelphiaElsevier Saunders:1934-50. [Google Scholar]
[2]. Caldwell DS, Carcinoma polyarthritis manifestations and differential diagnosisMed Grand Rounds 1982 1:378 [Google Scholar]
[3]. Kurihara Y, Oku K, Suzuki A, Ohsone Y, Okano Y, A case of calcinomatous polyarthritis presenting rheumatoid arthritis-like polyarthritis as the initial symptom of gastric cancerJapanese J Clin Immunol 2012 35(5):439-45.10.2177/jsci.35.43923124087 [Google Scholar] [CrossRef] [PubMed]
[4]. Kamel S, Abdel-Nasser A, Mohamed M, Rheumatic manifestations of hematologic malignancies: correlation with laboratory markersJ Hematol Malignanc 2011 1(1):15-23.10.5430/jhm.v1n1p15 [Google Scholar] [CrossRef]
[5]. Bruzzese V, Hassan C, Zullo A, Zampa G, Rheumatoid arthritis: a complication of aromatase inhibitor therapy?Int J Immunopathol Pharmacol 2011 24(4):1099-101.10.1177/03946320110240043022230418 [Google Scholar] [CrossRef] [PubMed]
[6]. Cappelli L, Shah A, Bingham C, Cancer immunotherapy-induced rheumatic diseases emerge as new clinical entitiesRMD Open 2016 2(2):e00032110.1136/rmdopen-2016-00032127752360 [Google Scholar] [CrossRef] [PubMed]
[7]. Handy CE, Robles G, Haque U, Houston B, T cell ALL presenting as seropositive rheumatoid arthritis: case report and review of the literature on seropositive paraneoplastic arthritisClin Rheumatol 2014 34(9):1647-50.10.1007/s10067-014-2697-924889405 [Google Scholar] [CrossRef] [PubMed]
[8]. Watson G, O’Neill L, Law R, McCarthy G, Veale D, Migrating polyarthritis as a feature of occult malignancy: 2 case reports and a review of the literatureCase Rep Oncol Med 2015 2015:01-07.10.1155/2015/93403926558124 [Google Scholar] [CrossRef] [PubMed]
[9]. Edavalath S, Chowdhury A, Phatak S, Misra D, Verma R, Lawrence A, Multiple myeloma masquerading as severe seropositive rheumatoid arthritis with subcutaneous nodules and mononeuritis multiplexInt J Rheum Dis 2016 20(9):1297-302.10.1111/1756-185X.1293527515238 [Google Scholar] [CrossRef] [PubMed]
[10]. Chu J, Demello D, O’Connor D, Chen S, Gale G, Pericarditis as presenting manifestation of acute nonlymphocytic leukemia in a young childCancer 1983 52(2):322-24.10.1002/1097-0142(19830715)52:2<322::AID-CNCR2820520222<3.0.CO;2-U [Google Scholar] [CrossRef]
[11]. Battle C, Bonfiglio T, Miller D, Pericarditis as the initial manifestation of acute leukemia: Report of a caseJ Pediatr 1969 75(4):692-94.10.1016/S0022-3476(69)80468-3 [Google Scholar] [CrossRef]
[12]. Aggarwal R, Liao K, Nair R, Ringold S, Costenbander K, Anti-citrullinated peptide antibody assays and their role in the diagnosis of rheumatoid arthritisArthritis Care Res 2009 61(11):1472-83.10.1002/art.2482719877103 [Google Scholar] [CrossRef] [PubMed]
[13]. Sheon R, Kirsner A, Tangsintanapas P, Samad F, Garg M, Finkel R, Malignancy in rheumatic disease: interrelationshipsJ Am Geriatr Soc 1977 25(1):20-27.10.1111/j.1532-5415.1977.tb00918.x299749 [Google Scholar] [CrossRef] [PubMed]
[14]. Stummvoll GH, Aringer M, Machold KP, Smolen JS, Raderer M, Cancer polyarthritis resembling rheumatoid arthritis as a first sign of hidden neoplasms: Report of two cases and review of the literatureScand J Rheumatol 2001 30(1):40-44.10.1080/03009740175006531911252691 [Google Scholar] [CrossRef] [PubMed]