Knee is the largest synovial joint in the body. It consists of three distinct and partially separated compartments that collectively form a complex ‘hinge’ joint. This arrangement is important for proper functioning of the powerful extensor and flexor muscles during propulsion. A complex arrangement of intracapsular and extracapsular ligaments helps in stabilising the considerable biomechanical stress to which the joint is subjected. The important ligaments are the articular capsule which is the fibrous capsule enclosing the joint cavity and is lined by a synovial membrane which is the most extensive and complex in the body, the menisci (medial and lateral) which are composed of fibrocartilage and separate the joint cavity into upper meniscofemoral and lower meniscotibial compartments and the cruciate ligaments (anterior and posterior) which are present in the form of cross ‘X’ within the joint capsule binding the bones of the joint i.e., femur and tibia and prevent displacement of tibia over femur. A few other ligaments are also mentioned in relation to the knee joint namely collateral ligaments (tibial and fibular), oblique popliteal ligaments, arcuate ligament and meniscofemoral ligament [1]. Until recently the MFLs were considered to be the vestigial structures present in this joint. The two MFLs, ligament of Humphry/aMFL and ligament of Wrisberg/pMFL connect the posterior horn of the lateral meniscus to the inner (lateral) aspect of the medial femoral condyle. The aMFL passes anterior to the PCL whereas pMFL passes behind it and attaches proximal to the margin of attachment of the PCL [1]. Studies all over the world have shown that these ligaments act as secondary restraints, supporting the posterior cruciate ligament in minimising displacement caused by posteriorly directed forces on the tibia [1]. Gupte CM et al., have explained that because of their slanting arrangement from the posterior horn of the meniscus up to the femoral intercondylar notch, they are oriented so that they can help to withstand tibial posterior draw [2]. Clancy WG et al., in their follow up of patients with rupture of the PCL, noted that PCL deficient knees in which the MFLs are intact have a reduced posterior drawer and may have a better prognosis than for those in which the MFLs are not seen at arthroscopy [3]. They are also said to be involved in controlling the motion of the lateral meniscus in conjunction with the tendon of popliteus during flexion [1]. Gupte CM et al., have mentioned the conservative role of MFLs after isolated rupture of PCL, where MFLs are found to embrace ruptured PCL and act as splints while PCL heals [4]. Watanabe AT et al., stressed that on MRI the MFL could be mistaken for intra-articular loose bodies, and Vahey TN et al., showed that the appearance of the MFL could be mistaken for a pseudotear of the lateral meniscus [5-7].
Gupte CM et al., have mentioned 94% incidence of at least one MFL in the specimens examined, Han SH et al., found at least one MFL in 88 out of 100 cases examined and Nagasaki S et al., report it in 84.2% cases [8-10], whereas others from different countries have suggested the presence of at least one MFL in 100% of their specimens [11-13].
Materials and Methods
After obtaining ethical approval from the concerned authorities, an observational, descriptive study was conducted on 38 human cadaveric knees belonging to both sexes, age ranging from 40-65 years. Cadaveric knees were dissected in the Department of Anatomy, Institute of Postgradaute Medical Education and Research (IPGMER), Kolkata, West Bengal, India, over a period of two years (May 2015- April 2017). Of 38 dissected knees 22 were paired. After treating them with 10% formalin, skin and subcutaneous tissue was removed from each knee. Keeping knee in extended prone position, posterior capsulotomy was done to expose PCL. The pMFL could be seen on its posterior surface when present. Knee was then turned to supine position. Ligamentum patellae was cut at its tibial attachment, transverse incision was given to the capsule followed by longitudinal incisions on two sides of the joint. Anterior Cruciate Ligament (ACL) was exposed. It was then cut at its femoral attachment to expose PCL. The aMFL was identified anterior to PCL wherever present. Knees free of any obvious deformity or external injury were included, deformed and broken knees were excluded from the study. The frequency of occurrence, anatomical variations and variations in length and width (at lateral, middle and medial ends) of both anterior and posterior MFL were recorded. Length and width were measured using vernier slide calipers. The mean value of the three observations was taken in each case to avoid observational bias.
Statistical Analysis
Data were analysed statistically using SPSS version 23.0.0.0, compared with that of previous studies and the conclusion was drawn. A p-value <0.05 is considered significant in all cases.
Results
At least one MFL was present in each of the 38 dissected knee joint with both the ligaments present in 10 (26.3%) joints [Table/Fig-1,2]. The frequency of occurrence of the ligaments and the gender based variations are shown in [Table/Fig-3]. An accessory band was found in 8 (21.05%) joints [Table/Fig-4]. Mean age of subjects with both MFLs is 45.40±3.14 years, those with either MFLs is 56.86±5.27 years. The dimensions of the MFL are shown in [Table/Fig-5]. Mean length of aMFL and pMFL is 25.74±1.98 mm and 31.63±4.87 mm respectively. Mean length of pMFL in males and females is 33.08±3.15 mm and 28.99±6.35 mm respectively. Mean width of pMFL at lateral end is 5.97±0.96 mm and 5.13±1.25 mm in males and females respectively.
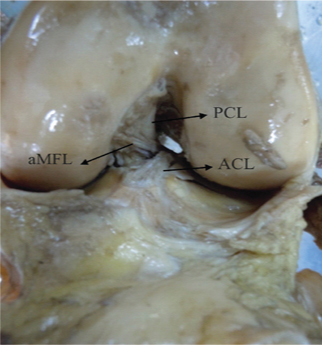
Anterior view of left knee joint showing aMFL passing in front of PCL.
aMFL- anterior Meniscofemoral Ligament; ACL- anterior Cruciate Ligament
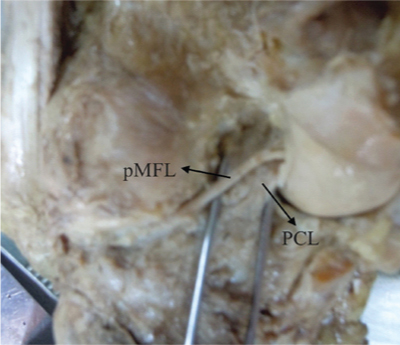
Posterior view of left knee joint showing pMFL passing behind PCL.
PCL- Posterior Cruciate Ligament; pMFL- posterior Meniscofemoral Ligament
Frequency of occurrence and gender variations.
| Parameters | Frequency of occurrence | Gender variations |
|---|
| Males | Females |
|---|
| Total knees | 38 | 24 | 14 |
| At least one MFL | 38 (100%) | 24 (100%) | 14 (100%) |
| Total aMFL (only aMFL+both aMFL and pMFL) | 14 (36.84%) | 8 (33.33%) | 6 (42.86 %) |
| aMFL only | 4 (10.53%) | 2 (8.33%) | 2 (14.28%) |
| Total pMFL (only pMFL+both aMFL and pMFL) | 34 (89.47%) | 22 (91.67%) | 12 (85.71%) |
| pMFL only | 24 (63.16%) | 16 (66.67%) | 8 (57.14%) |
| Both aMFL and pMFL | 10 (26.32%) | 6 (25%) | 4 (28.57%) |
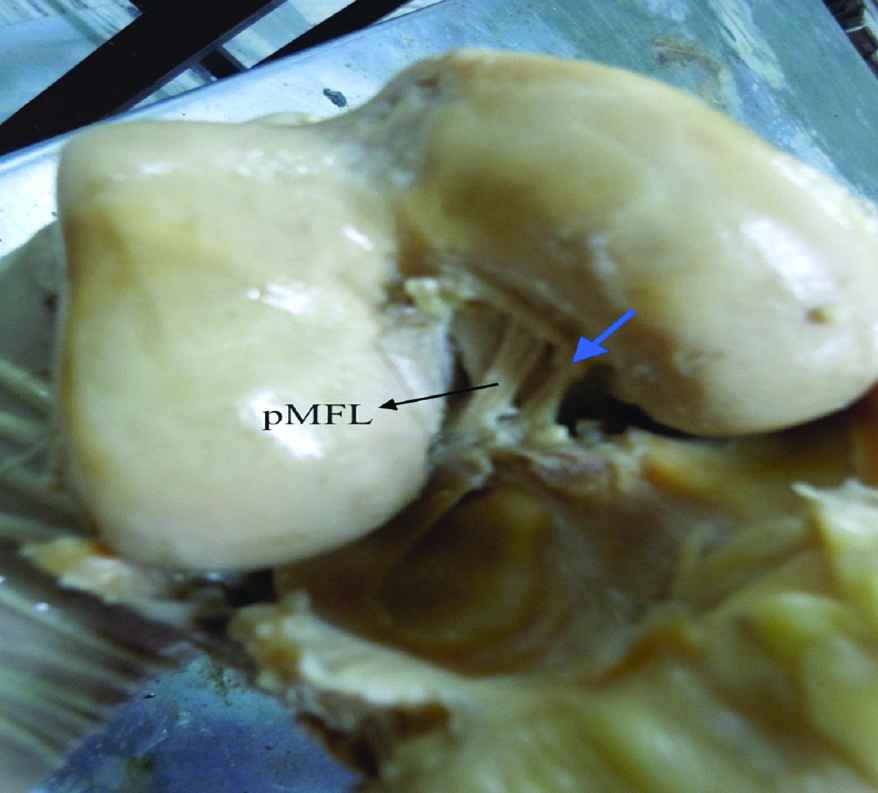
Accessory band (blue arrow) of pMFL seen in the anterior view of right knee joint.
pMFL- posterior Meniscofemoral Ligament
Dimensions of meniscofemoral ligaments.
| Parameters | Number | Length in mean±SD (mm) | Width in mean±SD (mm) |
|---|
| Lateral end | Midpoint | Medial end |
|---|
| Total aMFLs | 14 | 25.74±1.98 | 5.62±0.95 | 4.93±0.74 | 5.61±0.97 |
| Total pMFLs | 34 | 31.63±4.87 | 5.68±1.13 | 4.92±1.16 | 5.39±1.19 |
| aMFLs in females | 6 | 24.75±2.64 | 5.10±0.79 | 4.64±0.79 | 5.10±0.95 |
| aMFLs in males | 8 | 26.48±0.92 | 6.00±0.91 | 5.14±0.67 | 6.00±0.83 |
| pMFLs in females | 12 | 28.99±6.35 | 5.13±1.25 | 4.40±1.31 | 5.07±1.34 |
| pMFLs in males | 22 | 33.08±3.15 | 5.97±0.96 | 5.20±1.00 | 5.58±1.08 |
Mean length of pMFL >aMFL (p-value <0.0001)
Mean length of pMFL in males >females (p-value=0.0167).
Mean width of lateral end of pMFL in males >females. (p-value=0.0359)
Frequency of occurrence: Both aMFL and pMFL were present in 10 (26.3%) out of 38 dissected joints, only aMFL in 4 joints (10.5%) and only pMFL in 24 joints (63.2%) as shown in [Table/Fig-3]. Frequency of occurrence of pMFL was the highest 34 (89.47%). In subjects where both the ligaments were present, the aMFL and pMFL have common attachment on the posterior horn of the lateral meniscus but on femur aMFL was found attached distal to PCL and pMFL proximal to it.
Gender variations: No statistically significant gender variation was found [Table/Fig-3].
Anatomical variations: Of the 28 knees with either of the ligaments, 8 (21.05%) showed the presence of an accessory band {2 (5.26%) with aMFLs and 6 (15.79%) with pMFL}. The band which extended from the lateral meniscus to the medial aspect of medial femoral condyle was taken as the main band. The accessory band was found blending with PCL at its femoral attachment in all the cases (aMFL/pMFL). Accessory band was narrow as compared to the main band as shown in [Table/Fig-4].
Variation with age: The mean age of subjects with both aMFL and pMFL (45.40±3.14 years) was significantly lower than those with either only aMFL or only pMFL (57.57±4.95 years), p-value <0.001.
Variation in the size of MFL: The pMFL was found longer than aMFL in the whole cohort. The pMFL in males was longer than that in females. Mean width of both the ligaments was comparable between the groups (aMFL and pMFL), only the lateral end of pMFL was broader in males than in females [Table/Fig-5].
Discussion
We have found at least one MFL in 100% knees dissected as is reported in some previous studies [11-13]. Few others report at least one MFL in 80-92.86% of their cases [8,14,15]. Some studies mention greater prevalence of pMFL as is found in the present study whereas a few others mention more of aMFL in their study subjects [Table/Fig-6] [8,9,11-13]. A recent study from Karnataka shows more subjects with both types of MFLs [Table/Fig-6] [15]. These variations can be explained by the different ethnic groups to which the study subjects belong. Gupte CM et al., have also suggested that higher prevalence of pMFL than others may result from misidentification of posterior oblique fibres of PCL [8].
Frequency of occurrence of MFLs as found in different studies [8,11-15].
| Parameters | Present study | Poynton AR et al., [11] | Wan AC and Felle P, [12] | Kusayama T et al., [13] | Cho JM et al., [14] | Gupte CM et al., [8] | Geetharani BG et al., [15] |
|---|
| Total knees | 38 | 42 | 60 | 26 | 28 | 84 | 40 |
| At least one MFL | 38 (100%) | 42 (100%) | 60 (100%) | 26 (100%) | 25 (89.28%) | 78 (92.86%) | |
| Total aMFL | 14 (36.84%) | 35 (83.33%) | 20 (33.33%) | 18 (69.23%) | 0 | 62 (73.81%) | |
| aMFL only | 4 (10.53%) | 8 (19.05%) | 6 (10%) | 6 (23.07%) | 0 | 20 (23.81%) | 5 (12.5%) |
| Total pMFL | 34 (89.47%) | 38 (90.48%) | 56 (93.33%) | 20 (76.92%) | 25 (89.28%) | 58 (69.05%) | |
| pMFL only | 24 (63.16%) | 11 (26.19%) | 42 (70%) | 8 (30.67%) | 25 (89.28%) | 16 (19.05%) | 12 (30%) |
| Both aMFL and pMFL | 10 (26.32%) | 27 (64.28%) | 14 (23.33%) | 12 (46.15%) | 0 | 42 (50%) | 15 (37.5%) |
Presence of accessory band has also been mentioned by Gupte CM et al., and Poynton AR et al., as found in the present study [Table/Fig-7] [8,11].
Frequency of occurrence of accessory bands in different studies [8,11].
| Parameters | Present study | Poynton AR et al., [11] | Gupte CM et al., [8] |
|---|
| Total knees | 38 | 42 | 84 |
| Knees with accessory bands | 8 (21.05%) | 16 (38.09%) | 2 (2.38%) |
| aMFL with accessory bands | 2 (5.26%) | 3 (7.14%) | 2 (2.38%) |
| pMFL with accessory bands | 6 (15.79%) | 13 (30.95%) | 0 |
Variations are also seen in size, with pMFL longer than aMFL, longer pMFL with broader lateral end in males as compared to females. Longer pMFL in males than in females is also reported in a Korean study by Han SH et al., [9]. No statistically significant difference was found between the lengths of aMFL in males and females, the widths of ligaments in males and females or between the widths of anterior and posterior MFLs in the present study as is found in some previous studies [Table/Fig-8] [8,11,15].
Dimensions of meniscofemoral ligaments in mean±SD (mm) in different studies [8,11,15].
| Parameters | Mean Lengths | Mean of Midpoint widths |
|---|
| Present study mean±SD (mm) | Poynton AR et al., [11] mean±SD (mm) | Gupte CM et al., [8] mean±SD (mm) | Geetharani BG et al., [15] | Present study mean±SD (mm) | Poynton AR et al., [11] mean±SD (mm) |
|---|
| Total aMFLs | 25.74±1.98 | | 20.7±3.9 | 20.2 | 4.93±0.74 | |
| Total pMFLs | 31.63±4.87 | | 23±4.2 | 27.9 | 4.92±1.16 | |
| aMFLs in females | 24.75±2.64 | 24.4±3.4 | | | 4.64±0.79 | 2.9±1.3 |
| aMFLs in males | 26.48±0.92 | 27.10±3.4 | | | 5.14±0.67 | 5.1±1.4 |
| pMFLs in females | 28.99±6.35 | 27.60±3.7 | | | 4.40±1.31 | 4.7±2.4 |
| pMFLs in males | 33.08±3.15 | 31.10±2.5 | | | 5.20±1.00 | 5.5±2.1 |
Le Minor JM, has given an evolutionary perspective of these variations. He noted that while pMFL is always present in animals like sheep, horse and dog, it is sometimes absent in man whereas there is no reported description of the aMFL in animals. So, he proposed that pMFL is a regressive structure, whereas aMFL is progressive in man [16]. This is not supported by present observations as we have found predominance of pMFL both in frequency and size.
Gupte CM et al., have mentioned that aMFL is slack in the extended knee and tighten with knee flexion. Conversely pMFL slackens with knee flexion and tightens in the extended knee as their femoral attachments are distal and proximal to the PCL attachment respectively. This explains their differential functions in stabilising the knee along with PCL, particularly against tibial posterior draw at different angles of flexion [4]. This can explain the difference in size of aMFL and pMFL, but functional importance of longer pMFL than aMFL and longer pMFL with broader lateral end in males as found in the present study needs to be further investigated.
We have found in the present study that the aMFL and pMFL have common attachment on the posterior end of lateral meniscus but separate attachments on femur. This can be due to splitting of a single ligament into two parts by PCL. Gupte CM et al., have opposed this as they found that the two MFLs have separate attachments on the posterior horn of lateral meniscus and on femur, the two are therefore separate entities.
Presence of either MFLs in older subjects and both in younger subjects suggests that there maybe degeneration of these ligaments with advancement of the age as is suggested by Gupte CM et al., [8].
Limitation
The number of knees dissected in the study was less as compared to studies done by Gupte CM, Han SH et al., Nagasaki S et al., Poynton AR et al., Wan AC and Felle P [8-12]. Better results are expected by including more number of cadavers in the study. There was no parity in the number of male and female cadavers taken up for the study. In addition to anatomy, radiological and arthroscopic evaluation of the meniscofemoral ligaments can give a better perspective and understanding about their occurrence and variations.
Conclusion
Variations in frequency of occurrence, anatomy and size of MFLs are found between the two genders and different age groups within the study group. A wide range of variations is also found between different ethnic groups when compared with previous studies. These variations could be explained on the basis of development and the differential functions of the two types of MFLs. Presence of either MFLs in older subjects and both in younger subjects suggests degeneration of these ligaments with the advancement of age. Hence, MFLs cannot be ignored as unimportant structures during knee joint radiological and arthroscopic examination. Moreover, correct identification and conservation of these ligaments has become important for proper diagnosis and treatment of some knee pathologies like PCL rupture.
Mean length of pMFL >aMFL (p-value <0.0001)
Mean length of pMFL in males >females (p-value=0.0167).
Mean width of lateral end of pMFL in males >females. (p-value=0.0359)