Burkholderia pseudomallei: Liver Abscess in a Diabetic Patient from Western India
Dhruv Kamlesh Mamtora1, Anita Mathew Davis2, Mohan Koppikar3, Nikhil Cunha4, Pallavi Bhalekar5
1 Consultant and Head, Department of Microbiology and Infection Control, S.L. Raheja, A Fortis Associate Hospital, Mumbai, Maharashtra, India.
2 Consultant, Department of Infectious Diseases, S.L. Raheja, A Fortis Associate Hospital, Mumbai, Maharashtra, India.
3 Consultant, Department of Surgery, S.L. Raheja, A Fortis Associate Hospital, Mumbai, Maharashtra, India.
4 Consultant, Department of Radiology, S.L. Raheja, A Fortis Associate Hospital, Mumbai, Maharashtra, India.
5 Supervisor, Department of Microbiology, S.L. Raheja, A Fortis Associate Hospital, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dhruv Kamlesh Mamtora, Consultant and Head, Department of Microbiology and Infection Control, S.L. Raheja, A Fortis Associate Hospital, Mahim, Mumbai-400016, Maharashtra, India.
E-mail: dhruv_mamtora@yahoo.com
In Indian subcontinent, liver abscesses are often caused by amoebic and gram-negative organisms. Burkholderia pseudomallei (B. pseudomallei) is an emerging pathogen in India. The spectrum of disease caused by B. pseudomallei is variable and liver abscesses are an infrequent presentation. We report a case of isolated liver abscess caused by B. pseudomallei in a 72-year-old diabetic male patient, who was referred from Goa. Patient was treated with pigtail drainage of abscess and injection ceftazidime was given during stay in hospital. Patient was discharged on co-trimoxazole and doxycycline. The repeated culture after prolonged therapy showed markedly reduced colonies with similar antibiotic pattern and patient was treated successfully. It is important that pus aspirates from liver abscesses are worked up for microbiological culture and prompt treatment is initiated in case of melioidosis which is an emerging infection in India.
Ceftazidime, Co-trimoxazole, Doxycycline, Melioidosis
Case Report
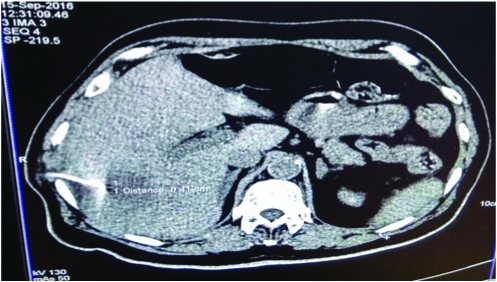
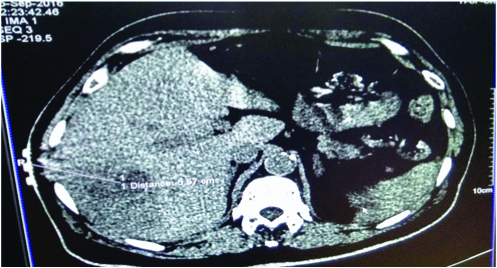
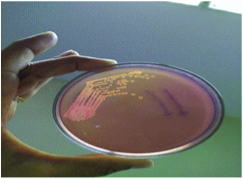
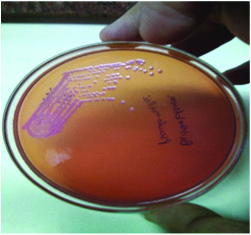
A 72-year-old male, Post Coronary Artery Bypass Graft (CABG), Post Percutaneous Transluminal Coronary Angioplasty (PTCA), a known case of diabetes since 25 years and hypertensive since 5 years hailing from Goa with history of repeated admission with similar complaints presented to emergency department with fever and chills since one month, dry cough since three week, mild breathlessness since two weeks. Patient had history of occasional alcohol consumption. Occupationally, patient was retired by profession. On general examination, there were no significant findings. On systemic examination, patient had soft non tender abdomen and no other significant systemic finding. Investigations done were: Complete Blood Count (CBC), Erythrocyte Sedimentation Rate (ESR), C-Reactive Protein (CRP), Computed Tomographic (CT) scan of chest, sputum for culture and GeneXpert, chest X-ray, blood culture, Ultrasonography (USG) abdomen etc. The imaging studies diagnosed it as a case of liver abscess and pigtail catheter was put [Table/Fig-1,2]. The pus sample was obtained by drainage and sent for routine examination, microscopy and automated aerobic culture and sensitivity testing. CBC showed leucocytosis with neutrophilia. Erythrocyte Sedimentation Rate (ESR) was 93 and 25 mm at end of one hour on day of admission and 11th day of hospitalisation, respectively. CRP levels were 125.75 mg/L, 98.35 mg/L and 0.16 mg/L on admission, eighth day and 11th day of hospitalisation. The pus routine and microscopy showed pus cells in sheets and no parasites (such as Entamoeba histolytica) were found. Indirect Haemagglutination (IHA) test was negative for Entamoeba histolytica. Cytology report showed acute suppurative inflammation. No amoebae or granulomas were seen. Liver function tests showed normal bilirubin level (Total: 0.7 mg/dL, Direct: 0.3 mg/dL), normal levels (20.8 and 25.08 IU/L) of serum Alanine Transaminase (ALT) and Aspartate Transaminase (AST) respectively, elevated alkaline phosphatase levels (170.42 U/L). Serum albumin was low (2.89 gm/dL), Serum globulin level was high (3.6 gm/dL) and Albumin:Globulin (A:G) ratio was low (0.92). Adenosine deaminase levels were normal (21.3 U/L). Clotting time was normal (4 minutes). Smear for acid fast bacilli, Tuberculosis (TB) culture by Mycobacterial Growth Indicator Tube (MGIT) and GeneXpert tests were negative ruling out tuberculosis. Blood culture showed no growth ruling out septicaemia. Pus culture from drainage grew non lactose fermenting colonies [Table/Fig-3]. On further incubation, colonies show classical metallic sheen [Table/Fig-4]. It was identified by VITEK® 2 compact system (bioMeriux, France) as B. pseudomallei. The isolate was sensitive to ceftazidime, chloramphenicol, co-trimoxazole, levofloxacin, meropenem and ticarcillin/clavulanic acid.
Computed tomographic guided percutaneous drainage of liver abscess.
Computed tomographic scan showing liver abscess. The distance from skin surface for drainage of abscess is 5.57 cm.
Non lactose fermenting colonies of B. pseudomallei after 48 hours of incubation.
Colonies showing aerobic oxidation (pink colour) and metallic sheen of B. pseudomallei on MacConkey’s agar after prolonged incubation of 72 hours.
After the culture report was obtained, the detailed reevaluation of patient from epidemiogical perspective was done. On further enquiry about the recreational activities, he mentioned about gardening which was his hobby. B. pseudomallei organism is a soil dwelling pathogen. This further reconfirms diagnosis. The antibiotic ceftazidime (40 mg/kg 8 hourly) was given intravenously for 14 days as per antibiotic sensitivity pattern; the patient was discharged on co-trimoxazole (sulfamethoxazole-trimethoprim 800 mg/160 mg) and doxycycline 100 mg twice a day for six months. Patient came for repeated scanning on bi monthly basis and every time scan was performed the pus sample was obtained and sent for culture. The repeat culture grew same pathogen with similar antibiotic sensitivity. Finally, after six months of complete therapy, lastly bloody discharge was obtained by assisted radiography was cultured and it showed no growth. It is important to give prolonged therapy for cure of disease and also repeated culture and radiographic examinations were done to assure complete cure of disease.
Discussion
Melioidosis disease spectrum can range from febrile illness to septicaemia. Focal presentation like abscess formation can occur in lungs, spleen and liver [1,2].
Diabetes is a known predisposing factor for melioidosis which was also present in the case [3]. B. pseudomallei is present in soil and fresh water hence occupational and outdoor work like agriculture, fishing, gardening and water sport increases likelihood of disease. Patient was long standing diabetic with poor glycaemic control and had hobby of gardening which increased likelihood of development of disease. Liver abscess brought about by melioidosis is clinically indistinguishable to other causes of pyogenic liver abscess. It similarly presents with prolonged high grade fever which is poorly responsive to usual empiric antibiotics and occasionally may present with right upper quadrant pain and jaundice. Consensus with regard to the management of liver abscess caused by B. pseudomallei has not yet been established due to the rarity of cases. Surgical intervention through either a percutaneous or open drainage has shown good outcomes compared to IV antibiotics alone [4]. Ceftazidimeis antibiotic of choice for meliodosis [5]. Effectiveness of ceftazidime is more than other third generation cephalosporins for Melioidosis [6]. Mortality associated with disease is high despite antibiotic therapy. Cases have been reported from Southeast Asia mainly Thailand, Malaysia, Vietnam, Taiwan etc., [7-11]. In India, few cases have been reported mainly from the southern and eastern part of the country [7-9]. Case of isolated liver abscess in young diabetic patient described in West Bengal was similar to present case [9]. Few cases of Melioidosis are reported from states of Kerala, Tripura, Orissa, Maharashtra and Tamil Nadu [7,9,12]. Three cases have been also reported from Mumbai however the presentation was musculoskeletal diseases [13]. This case is of epidemiological importance because of its unique presentation as isolated liver abscess as previously such presentations are few from literature in India [7-9]. Since, the patient is hailing from Goa, from where cases have been already reported, further detailed epidemiological enquiry is necessary [14].
Cost of recurrent disease is more than cost of prolonged and appropriate treatment as far as the B. pseudomallei is concerned. Hence, important learning lesson is appropriate diagnosis and prompt therapy as per antibiotic sensitivity pattern. We successfully treated patient with intravenous ceftazidime for 14 days followed by cotrimoxazole and doxycycline orally for six months.
Conclusion
Melioidosis can present as isolated liver abscess. It is important to promptly diagnose condition as early as possible and initiate appropriate prolonged therapy for curing the disease. Also, detailed history and communication between clinician and microbiologist is important in cases with unusual presentations of rare disease.
[1]. Vatcharapreechasakul T, Suputtamongkol Y, Dance DA, Chaowagul W, White NJ, Pseudomonas pseudomallei liver abscesses: a clinical, laboratory, and ultrasonographic studyClin Infect Dis 1992 14(2):412-17.10.1093/clinids/14.2.4121554825 [Google Scholar] [CrossRef] [PubMed]
[2]. White NJ, MelioidosisLancet 2003 361(9370):1715-22.10.1016/S0140-6736(03)13374-0 [Google Scholar] [CrossRef]
[3]. Jesudason MV, Anbarasu A, John TJ, Septicaemic melioidosis in a tertiary care hospital in south IndiaIndian J Med Res 2003 117:119-21. [Google Scholar]
[4]. Martin PF, Teh CS, Casupang MA, Melioidosis: a rare cause of liver abscessCase Rep Hepatol 2016 2016:591037510.1155/2016/591037527529039 [Google Scholar] [CrossRef] [PubMed]
[5]. White NJ, Chaowagul W, Wuthiekanun V, Dance DA, Wattanagoon Y, Pitakwatchara N, Halving of mortality of severe melioidosis by ceftazidimeLancet 1989 2(8665):697-701.10.1016/S0140-6736(89)90768-X [Google Scholar] [CrossRef]
[6]. Thibault FM, Hernandez E, Vidal DR, Girardet M, Cavallo JD, Antibiotic susceptibility of 65 isolates of Burkholderia pseudomallei and Burkholderia mallei to 35 antimicrobial agentsJ Antimicrob Chemother 2004 54(6):1134-38.10.1093/jac/dkh47115509614 [Google Scholar] [CrossRef] [PubMed]
[7]. Mukhopadhya A, Balaji V, Jesudason MV, Amte A, Jeyamani R, Kurian G, Isolated liver abscesses in melioidosisIndian J Med Microbiol 2007 25(2):150-51.10.4103/0255-0857.3272417582188 [Google Scholar] [CrossRef] [PubMed]
[8]. Barman P, Sidhwa H, Shirkhande PA, Melioidosis: a case reportJ Glob Infect Dis 2011 3(2):183-86.10.4103/0974-777X.8169721731307 [Google Scholar] [CrossRef] [PubMed]
[9]. Pal P, Ray S, Moulick A, Dey S, Jana A, Banerjee K, Liver abscess caused by Burkholderia pseudomallei in a young man: a case report and review of literatureWorld J Clin Cases 2014 2(10):604-07.10.12998/wjcc.v2.i10.60425325075 [Google Scholar] [CrossRef] [PubMed]
[10]. Ben RJ, Tsai YY, Chen JC, Feng NH, Non-septicemic Burkholderia pseudomallei liver abscess in a young manJ Microbiol Immunol Infect 2004 37(4):254-57. [Google Scholar]
[11]. Lee YL, Lee SS, Tsai HC, Chen YS, Wann SR, Kao CH, Pyogenic liver abscess caused by Burkhoderia pseudomallei in TaiwanJ Formos Med Assoc 2006 105(8):689-93.10.1016/S0929-6646(09)60171-6 [Google Scholar] [CrossRef]
[12]. Ramamoorthi K, Saravu K, Mukhyopadhyaya C, Barakur AS, Brief communication (original). Melioidosis: an underdiagnosed disease in India (epidemiology, clinical features, and outcomes)Asian Biomedicine 2013 7(2):249-56. [Google Scholar]
[13]. Patil HG, Gundavda M, Shetty V, Soman R, Rodriques C, Agashe VM, Musculoskeletal melioidosis: an under-diagnosed entity in developing countriesJ Orthop 2016 13(1):40-42.10.1016/j.jor.2015.08.00126955222 [Google Scholar] [CrossRef] [PubMed]
[14]. Saravu K, Mukhopadhyay C, Vishwanath S, Valsalan R, Docherla M, Vandana KE, Melioidosis in southern India: epidemiological and clinical profileSoutheast Asian J Trop Med Public Health 2010 41(2):401-09. [Google Scholar]