Root Coverage of Class III Recession using Free Gingival Graft using Novel Root Coverage Esthetic Score
Avita Rath1, Bennete A Fernandes2, Priyadarshini H Ramamurthy3, Preena Sidhu4, Shalini Saichandran5
1 Lecturer, Department of Faculty of Dentistry, SEGi University, Petaling Jaya, Selangor, Malaysia.
2 Senior Lecturer, Department of Faculty of Dentistry, SEGi University, Petaling Jaya, Selangor, Malaysia.
3 Lecturer, Department of Faculty of Dentistry, SEGi University, Petaling Jaya, Selangor, Malaysia.
4 Lecturer, Department of Faculty of Dentistry, SEGi University, Petaling Jaya, Selangor, Malaysia.
5 Senior Lecturer, Department of Conservative Dentistry and Endontics, Sathyabama University Dental College and Hospital, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Avita Rath, Lecturer, Faculty of Dentistry, Level 2, SEGi University, No. 9, Jalan Teknologi, PJU5, Kota Damansara, Petaling Jaya, Selangor-47810, Malaysia.
E-mail: drrathavita@yahoo.com
A variety of regenerative procedures has been used for the correction of gingival recession defects. However, root coverage can be quite challenging in cases of deep and wide Miller’s class III recession defects. Free Gingival Graft (FGG) technique has been the most preferred choice of treatment in cases of an inadequate width of attached gingiva. But currently, due to various drawbacks of FGG, and versatility of connective tissue grafts and other new techniques, FGG’s status as the most sought-after procedure in periodontal plastic surgeries has been eluded. The present case highlights a case of class III gingival recession which was successfully treated with this technique with postoperative evaluation using Root coverage Esthetic Score (RES) scores.
Gingival recession, Keratinised tissue, Periodontal plastic surgery
Case Report
A 29-year-old male patient reported to SEGi Oral Health Center with a chief complaint of an unaesthetic appearance of gums in the lower front tooth region associated with sensitivity from past one year. The patient had not visited any dentist before as the sensitivity was mild, but he complained that it had increased in the last two months. The patient was a non smoker, and no significant medical or family history was reported.
On clinical examination, the patient had the full complement of permanent teeth except for #31 which was congenitally missing. Oral hygiene was fair with mild calculus on the lingual surface of lower anterior teeth. Periodontal examination of the area of complaint showed Miller’s Class III gingival recession in relation to #41 with Clinical Attachment Loss (CAL) of 9 mm, Probing Pocket Depth (PPD) of 2 mm, Recession Height (RH) of 7 mm and Width (RW) at cervical region was 5 mm, at mid and apical region was 4 mm respectively, and the Width of Keratinised Tissue (WKT) was about 1mm [Table/Fig-1,2]. Additionally, there was CAL of 2 mm seen in relation to #44 and #45 which could be due to improper brushing technique by the patient. Hence, it was diagnosed as a case of chronic localised periodontitis in relation to #41.
Preoperative photograph showing Miller’s class III gingival recession in relation to #41.

Dental photograph of #41 region showing the clinical measurement of the gingival recession using William’s probe.
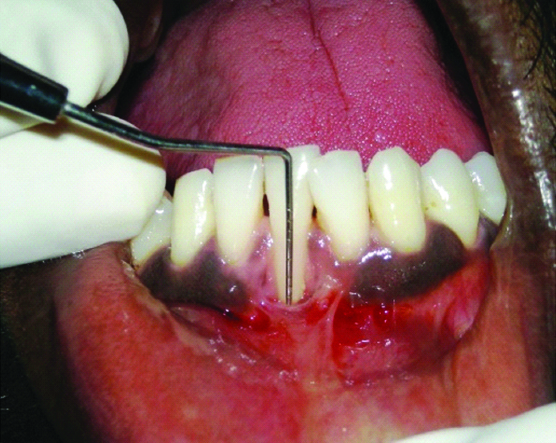
Considering that, it was in the lower anterior region with lack of keratinised tissue, we planned for vestibular deepening with FGG procedure. In the first visit, a thorough full mouth scaling was done, along with root debridement in relation to #41. The patient was given basic oral hygiene instructions with Charter’s method of brushing technique reinforced’ in that area and asked to report after one week. On the second visit, the site was examined and prepared for the surgery. Local anaesthesia was administered at the recipient site; the dimensions of the required graft were mapped using Williams’s periodontal probe and were simulated on a tin foil which was later cut in the shape of the graft to be procured. A horizontal partial thickness incision was placed using “15 number Bard-Parker® blade” at the mucogingival junction of the #41 to dissect the alveolar mucosa from the keratinised tissue, and extended to adjacent one tooth on each side to deepen the vestibule at the recipient site. The keratinised tissue was then de-epithelialised around the root of the lower right central incisor, leaving the interdental papillae intact on each side of the tooth, to expose the underlying connective tissue and to create a trapezoidal recipient bed [Table/Fig-3].
Dental photograph showing de-epithelialisation of the recipient bed around #41.

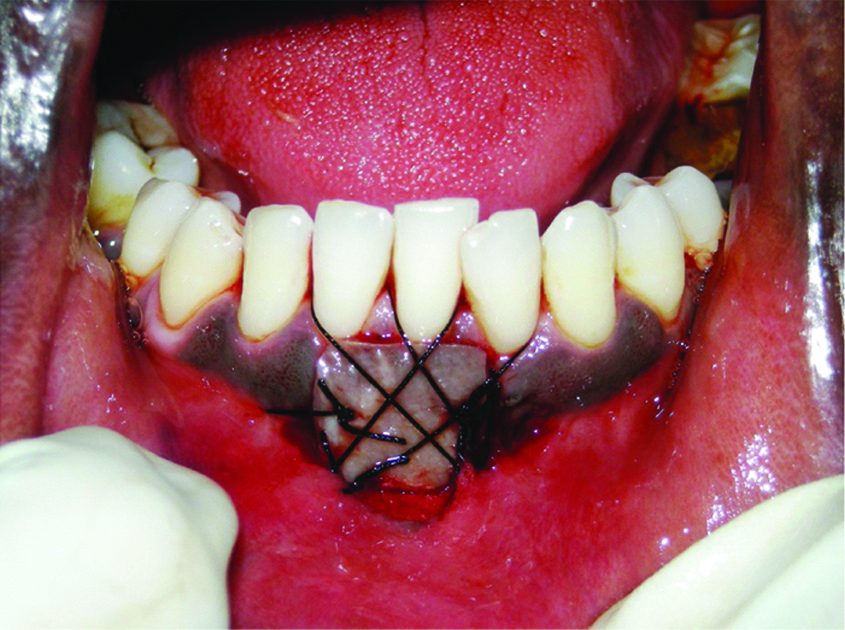
On the donor site, the FGG graft of 2 mm thickness was harvested from palate extending from the mesial aspect of #27 to the mesial aspect of #26 using the tin foil template prepared earlier [Table/Fig-4,5]. The graft thus obtained was trimmed, contoured, adapted, and sutured using 4-0 silk suture on to the recipient bed [Table/Fig-6]. Tin foil and the periodontal pack was placed over the recipient site, and postoperative instructions were given. The healing was uneventful at 10 days. The patient was also recalled at three months and six months postoperatively, and the parameters were recorded [Table/Fig-7].
Donor site of patient’s palate after the graft procurement.
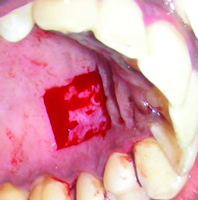
Photograph showing free gingival graft procured from the donor site.

Postoperative photograph showing graft sutured using 4-0 silk sutures at #41 region.
Six months postoperative photograph of #41 region.

Discussion
Obtaining predictable and aesthetic root coverage has become an integral part of periodontal therapy [1]. Various mucogingival surgical procedures are used to halt the progression of the gingival recession and to correct poor aesthetic appearance and to attain a broad band of keratinised gingiva, which is crucial for better plaque control, FGG is one of the treatment modality of choice [2,3]. It was introduced by Bjorn in 1963 and is a highly predictable in increasing the width of keratinised gingiva [4,5]. Later, in 1981 Caffesse RG and Espinel MC used this technique for root coverage as well. But currently, due to various drawbacks of FGG, and the versatility of connective tissue grafts, FGG’s status as the most sought after procedure in periodontal plastic surgeries has faded [6].
Studies done in the past using FGG technique have reported a coverage of 40-70% in Class I and II recessions but the relative inadequacy of interdental papilla, as well as the position of the tooth as seen in Class III recession, can result in incomplete root coverage [7,8,9]. However, in the present case, we could achieve a 100% root coverage. Postoperatively, three months after the surgery, there was 7 mm of root coverage that also lead to a gain of 7 mm of WKT which was the same even at the sixth month [Table/Fig-8]. To measure it in an objective way, we used RES, a standardised system for aesthetic evaluation after root coverage which was introduced by Cairo F et al., and has been used widely in many RCTs [10]. The RES scores for the present case were 100% at third and sixth months for all parameters except for gingival colour [Table/Fig-9]. These results resonated with studies done by Yucea BH et al., and Cortellini P et al., wherein the scores were favourable in terms of mucogingival alignment, soft tissue texture but unfavourable in terms of colour match [11,12]. Also, there was a significant reduction in dentinal hypersensitivity postoperatively as reported by the patient.
Pre and postoperative values of clinical parameters in mm in relation to #41.
| Clinical Parameters (mm) | Baseline | Three Months | Six Months |
|---|
| PPD | 2 | 2 | 2 |
| CAL | 9 | 0 | 0 |
| RH/RD | 7 | 0 | 0 |
| RW | 5 | 0 | 0 |
| WKT | 1 | 8 | 8 |
PPD: Probing Pocket depth, CAL: Clinical Attachment Loss, RH/RD: Recession height/depth, RW: Recession Width, WKT: Width of Keratinised gingival
Root coverage aesthetic score (RES) of #41 after the surgery.
| RES Score Criteria | Three monthsPostoperative | Six monthsPostoperative |
|---|
| GM | 6 | 6 |
| MTC | 1 | 1 |
| STT | 1 | 1 |
| MJJ | 1 | 1 |
| GC | 0 | 0 |
Level of GM-gingival margin, MTC: Marginal tissue contour, STT: Soft tissue texture, MJJ: Mucogingival junction alignment, GC: Gingival colour
Even though good colour match was unachievable, nevertheless, the patient was rationally happy, as the aesthetic discrepancy was considerably reduced. The main reason for the mismatch in colour could be deep melanin pigmentation in gingiva in the present patient, where race factor plays a pivotal role. Some studies have reported that grafted tissue might retain a few characteristics of the donor site and the melanisation might reappear after six months [13]. However, the patient did not turn up after the follow up at six months, so we could not draw any conclusion regarding the colour match as well as photographic evidence of the operative site.
Conclusion
Inspite of the limited colour match, FGG may still be the best treatment choice for gingival recession in lower anterior teeth region, with an inadequate amount of keratinised gingiva to increase the apical-coronal amount of the keratinised gingival tissue is the desired outcome in these cases.
PPD: Probing Pocket depth, CAL: Clinical Attachment Loss, RH/RD: Recession height/depth, RW: Recession Width, WKT: Width of Keratinised gingival
Level of GM-gingival margin, MTC: Marginal tissue contour, STT: Soft tissue texture, MJJ: Mucogingival junction alignment, GC: Gingival colour
[1]. Purushotham S, Manjunath N, D’souza ML, Shetty R, An interdisciplinary approach for the management of noncarious lesionsJ Indian Soc Periodontol 2016 20(2):211-15. [Google Scholar]
[2]. Richardson CR, Allen EP, Chambrone L, Langer B, McGuire MK, Zabalegui I, Periodontal soft tissue root coverage procedures: practical applications from the AAP regeneration WorkshopClin Adv Periodontics 2015 5:02-10.10.1902/cap.2015.140059 [Google Scholar] [CrossRef]
[3]. George AM, Rajesh KS, Hegde S, Kumar A, Two stage surgical procedure for root coverageJ Indian Soc Periodontol 2012 16(3):436-41.10.4103/0972-124X.10092623162343 [Google Scholar] [CrossRef] [PubMed]
[4]. Bjorn H, Free transplantation of gingiva propriaSwed Dent J 1963 22:684-89. [Google Scholar]
[5]. Shah R, Thomas R, Mehta DS, Recent modifications of free gingival graft: A case seriesContemporary Clinical Dentistry 2015 6(3):425-27.10.4103/0976-237X.16191026321849 [Google Scholar] [CrossRef] [PubMed]
[6]. Caffesse RG, Espinel MC, Lateral sliding flap with a free gingival graft technique in the treatment of localized gingival recessionsInt J Periodontics Restorative Dent 1981 1(6):22-29. [Google Scholar]
[7]. Borghetti A, Gardella JP, Thick gingival autograft for the coverage of gingival recession: A clinical evaluationInt J Periodontics Restorative Dent 1990 10(3):216-29. [Google Scholar]
[8]. Remya V, Kishore Kumar K, Sudharsan S, Arun KV, Free gingival graft in the treatment of class III gingival recessionIndian J Dent Res 2008 19(3):247-52.10.4103/0970-9290.4295918797103 [Google Scholar] [CrossRef] [PubMed]
[9]. Biswas S, Nair SK, Kotha M, Kumar RV, Shivaprasad BM, Free gingival graft: A surgical boon for receding gumsJ Health Sci Res 2014 5(2):25-28.10.5005/jp-journals-10042-1006 [Google Scholar] [CrossRef]
[10]. Cairo F, Rotundo R, Miller PD, Pini Prato GP, Root coverage aesthetic score: A system to evaluate the aesthetic outcome of the treatment of gingival recession through evaluation of clinical casesJ Periodontol 2009 80(4):705-10.10.1902/jop.2009.08056519335093 [Google Scholar] [CrossRef] [PubMed]
[11]. Yucea BH, Turkala HA, Karatasa O, Altıntepeb SS, Root aesthetic score (RES) comparisons of FGG and PE-FGG procedures in miller class II and III recessions in mandibular anterior teethCumhuriyet Dent J 2015 18(2):148-55. [Google Scholar]
[12]. Cortellini P, Tonetti M, Prato GP, The partly epithelialized free gingival graft (pe-fgg) at lower incisors. A pilot study with implications for alignment of the mucogingival junctionJ Clin Periodontol 2012 39(7):674-80.10.1111/j.1600-051X.2012.01896.x22587305 [Google Scholar] [CrossRef] [PubMed]
[13]. Spinell T, Tarnow D, Restoring lost gingival pigmentation in the aesthetic zone: A case reportJ Am Dent Assoc 2015 146(6):402-05.10.1016/j.adaj.2014.12.02126025828 [Google Scholar] [CrossRef] [PubMed]