Occupational health hazards have an upward trend among large number of workers employed in unorganised and informal industry. Beedi industry is a vital agro-industry in Indian National Economy, prevalent in economically backward households as the industry was outsourced long back. Beedi rolling is one of the most common and popular job to reach daily expenses, especially amongst women of India, inspite of it being a hazardous profession. In West Bengal, there are more than 19 lakh beedi workers and out of them nearly 15 lakh were issued identity card [1,2]. Poor working environment, occupational exposure, demographic factors and improper lifestyle greatly affect labour forces of this unorganised industry by exposure to hazardous substances [2,3]. According to Beedi and Cigar workers (Conditions of Employment) Act of 1966, the home workers and also those working under agreement with the employers are contract labourers, classified as beedi rollers and workers [4]. In India, estimated 55 lakh people are associated with this industry, spread over rural and semi-urban areas, in 16 states; five lakh people are in this profession in West Bengal. Overall 1.83 million people have occupational morbidities which is 20% of the global burden. Ironically, these women are not aware of this fact [4-6]. Published literature estimates that about 76% of the beedi making population is female providing half of the total family income [5,7]. The morbidities of beedi workers can be in form of physical, chemical, mechanical, psychosocial hazards leading to lung diseases, musculoskeletal injuries, eye and skin disorders due to exposure to tobacco dust, fumes that absorb via skin, mucous membrane [8,9]. The lung volumes decrease with an increase in the age and tenure of work [10,11]. Despite a hazardous profession, their health and working conditions have never been brought into limelight of public discussion and awareness. The main aim of the research was to determine the current health status with associated morbidities of the beedi workers of West Bengal, India. The sociodemographic and economic background, working condition and morbidity associated factors were also assessed to achieve the aim.
Materials and Methods
A descriptive, cross-sectional survey was conducted from November 2016 to January 2017 in different wards in Kalyani. It was done by the researchers of the College of Medicine and JNM Hospital, Nadia district, West Bengal, India. Ethical clearance was obtained from Institutional Ethics Committee (IEC) and the study was initiated after getting approval from the governing body of the institute. The participants were ensured about strict maintenance of anonymity, confidentiality and protection of all gathered information and use only for research. Kalyani, which is the sub-divisional headquarter of Nadia district was selected purposively out of 19 districts of West Bengal. In Nadia district, beedi work was one of the major occupations at the household level. Kalyani municipality was selected by simple random sampling. This municipality has 20 wards and caters a population of nearly one lakh [12,13]. In the absence of comprehensive nationwide database on the background information of either registered or unregistered beedi rollers, investigators used an incomplete database available from a local Non Government Organization (NGO). The present study was conducted in the four wards among all the resident beedi workers, available during the survey time. No sample size was determined as complete enumeration was done. The workers who had left the job, physically unwell, not in current occupation for at least one year and did not provide consent were excluded. More than 500 beedi workers were registered with the NGO as evident from an office copy. Data collection was done by the investigators by an interview and general examination with a predesigned data collection tool. The study was explained to each participant individually and a verbal informed consent was obtained. The interview and clinical examination was mostly conducted at their home while closely observing their working condition. Two weeks were allotted for each ward. Initially, one worker was identified in each ward to approach the ward to get help identify other workers. Body weight was measured using a standard portable weighing scale to the nearest 0.1 kg with minimum clothing and without shoes. Height was measured without shoes with help of a wooden stand with steel tape attached to the nearest 0.1 cm. BMI as (kg/m2) was calculated by dividing observed weight (in kg) by height (in square meters) [14]. BP was recorded with calibrated standardised sphygmomanometer in the sitting posture in right upper arm; two readings at five minutes intervals. If high BP (≥140/90 mmHg) was noted, a third reading was taken after 30 minutes; lowest reading was considered as final. All participants were advised to avoid tea, coffee, smoking, alcohol, and take rest at least 30 minutes before examination [15]. The total procedure for each individual involved 15-20 minutes and data from five to six participants was collected everyday. Adequate privacy was maintained during anthropometric measurements and examinations. A predesigned, semi structured proforma was used to collect data on sociodemographic profile, awareness of hazards, systemic symptoms along with general and anthropometric examination. The proforma was then translated into their local language. After face and content validation by experts, back translation and retranslation was done. During the survey, 125 workers were approached; seven did not give consent, 10 workers were in this occupation for less than one year so not included. The workers who left the job were also not included. Finally, 103 workers participated in the study. The social class, housing status in terms of overcrowding, inadequate lighting and ventilation, awareness of hazards were assessed as per the practical guide book of the concerned department that conducted the study [16]. The self-reported systematic hazards of musculoskeletal, eye, respiratory, cardiovascular system etc., along with presence of high BP and BMI were also assessed in the study. Updated BG Prasad classification (May 2016) was used to determine social class [17]. Overweight was considered with BMI 25 kg/m2 or more but less than 30 kg/m2 and obesity with BMI 30 kg/m2 or more [18]. Hypertension was defined as Systolic Blood Pressure (SBP) more than 140 mmHg and Diastolic Blood Pressure (DBP) more than 90 mmHg [19]. Awareness on hazards of beedi smoking and anyavailable health scheme was enquired. Workers were examined for presence of pallor, clubbing and abnormal gait. The skin of hands was inspected for sensation, tanning, hypopigmented patch.
Statistical Analysis
Data were coded and entered into SPSS Version 16.0 for analysis; descriptive statistics was used for independent variables. Chi-square and Fisher’s exact test was calculated to find statistical association between age group, education, social class and hypertension as well as obesity. Odds Ratio (OR), 95% Confidence Interval (CI) was measured by using StatCalc Epi Info version 6.0. An alpha level of 5% was considered significant.
Results
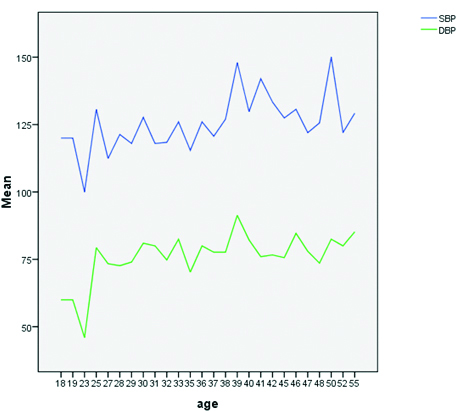
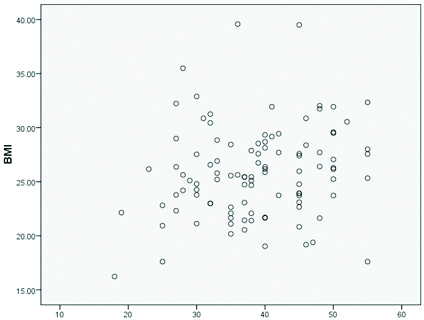
The study had 103 Hindu beedi workers. Mean (±SE) age of workers was 38.69 (±8.53) years. Nuclear family structure was more prevalent (n=60, 58.30%). The average (SE) monthly family income was Rs. 6177.67±270.90. More than half (57.28%) started beedi rolling in the age range 15 to 25 years [Table/Fig-1]. Nearly, one-third were in this job profile for more than 20 years. The women worked at home by sitting in uncomfortable posture for long hours. Overcrowding was noted in (n=36, 34.95%) houses, dampness and inadequate lighting was noticed nearly in one in every four houses, while inadequate ventilation was present in (n=21, 20.4%) houses. Regarding safety measures, only (n=30, 29.12%) workers washed their hand after beedi rolling while none ofthem wore any gloves or masks. The response to the awareness level on any benefitting laws was nil among the respondents. [Table/Fig-2] showed that eyes were most commonly affected followed by musculoskeletal system in majority of participants. Dull aching headache was the most common symptom followed by lower back pain, neck pain, difficulty invision, palpitation. Epigastric pain after taking food and hyperacidity was in (n=41, 39.81%) and (n=62, 60.19%) respectively. More than half workers had lower limb weakness (n=54, 52.4%) and vertigo (n=60, 58.20%), (n=23, 22.33%) had difficulty in hearing. Pallor was noted in 20 participants and clubbing was observed in (n=9, 8.74%) workers. Skin of the hands showed loss ofsensation among five workers. SBP ranged from 90-178 mmHg and DBP ranged from 46-110 mmHg. More than one-third was in pre hypertension stage. Isolated systolic and diastolic hypertension was recorded in (n=17, 16.50%) and (n=5, 4.85%) women respectively. Mean (±SE) body weight was 57.12 kg (10.68) and mean BMI (±SE) was 25.90 kg/m2 (±4.35); overweight and obesity as noted in (n=46, 44.66%) and (n=14, 13.59%) workers respectively. In bivariate analysis, both high BP (p-value <0.01) and BMI (p-value<0.05) were significantly associated with increasing age but lower education had strong association with high BP (70.9% vs. 41.2%). The variables considered were sociodemographic and economic attributes. The proportion of musculoskeletal symptoms was significantly more among workers who rolled more than 500 beedi per day. Eye problems were more among the workers who were in the profession for more then 20 years and had worked for more than six hours a day (p-value <0.05) [Table/Fig-3,4]. It was noted that both systolic and diastolic blood pressure of the respondents showed ups and downs with advancing age whereas in case of BMI, it was seen that many of the workers were overweight with increasing age [Table/Fig-5,6].
Background information of study population (n=103).
| Variables | Frequency (%) |
|---|
| Age group (years) |
| 18-27 | 11 (10.68) |
| 28-37 | 35 (33.98) |
| 38-47 | 38 (36.89) |
| ≥ 48 | 19 (18.44) |
| Education |
| Illiterate | 42 (40.77) |
| Primary/middle | 44 (42.71) |
| Secondary and above | 17 (16.52) |
| Social class as per modified BG Prasad’s Socioeconomic scale, 2016 |
| Class II | 1 (0.97) |
| Class III | 20 (19.41) |
| Class IV | 60 (58.25) |
| Class V | 22 (21.35) |
| Descriptive statistics of beedi rolling |
| Facts | Range (Maximum, minimum) | Mean (±SE) |
| Age of initiation (years) | 44 (50, 6) | 21.86 (0.784) |
| Working days/month | 27 (30, 3) | 20.04 (0.902) |
| Duration (months) | 420 (432, 12) | 184.87 (11.307) |
| Working hours/day | 5 (8, 3) | 4.91 (0.144) |
| Beedi rolled/day | 900 (1000, 100) | 571.36 (21.381) |
Profile of systematic morbidities reported by beedi workers (n=103).
| Morbidities | Age group (years) n (%) | Total n (%) |
|---|
| 18-27 | 28-37 | >37 |
|---|
| Respiratory | Hoarseness | 1 (5.00) | 6 (30.00) | 13 (65.00) | 20 (19.41) |
| Cough | 3 (7.89) | 10 (26.31) | 25 (65.78) | 38 (36.89) |
| Cardiovascular | Palpitation | 4 (7.01) | 16 (28.07) | 37 (64.91) | 57 (55.34) |
| Breathlessness | 0 (0.00) | 12 (37.50) | 20 (62.50) | 32 (31.06) |
| Gastrointestinal | Epigastric pain | 3 (7.31) | 13 (31.70) | 25 (60.97) | 41 (39.80) |
| Hyperacidity | 6 (9.67) | 17 (27.41) | 39 (62.90) | 62 (60.19) |
| Eye | Headache | 5 (7.14) | 20 (28.57) | 45 (64.28) | 70(67.96) |
| Difficulty in vision | 2 (3.22) | 12 (19.35) | 48 (77.41) | 62 (60.19) |
| Eye pain | 2 (5.55) | 10 (27.77) | 24 (66.66) | 36 (34.95) |
| Redness | 0 (0.00) | 10 (34.48) | 19 (65.51) | 29 (28.15) |
| ENT | Vertigo | 4 (6.66) | 18 (30.0) | 38 (63.33) | 60 (58.25) |
| Difficulty in hearing | 2 (8.69) | 4 (17.39) | 17 (73.91) | 23 (22.33) |
| Musculoskeletal | Low backache | 7 (10.29) | 18 (26.47) | 43 (63.23) | 68 (66.01) |
| Neckache | 5 (7.93) | 19 (30.15) | 39 (61.90) | 63 (61.16) |
| Lower limb weakness | 5 (9.25) | 14 (25.92) | 35 (64.81) | 54 (52.42) |
| Hand weakness | 7 (12.06) | 17 (29.31) | 34 (58.62) | 58 (56.31) |
| Pallor | Present | 1 (5.00) | 7 (35.00) | 12 (60.00) | 20 (19.41) |
| Skin condition | Tanning | 2 (6.66) | 11 (36.66) | 17 (56.66) | 30 (29.12) |
| Rough | 3 (15.78) | 2 (10.52) | 14 (73.68) | 19 (18.44) |
| Blood pressure | Normal | 7 (20.00) | 18 (51.42) | 10 (28.57) | 35 (34.00) |
| Pre hypertension | 3 (8.57) | 7 (20.00) | 25 (71.42) | 35 (34.00) |
| *Hypertension | 1 (.03) | 10 (30.30) | 22 (66.66) | 33 (32.00) |
| Obesity as per BMI | Normal | 5 (12.82) | 16 (41.02) | 18 (46.15) | 39 (37.86) |
| Overweight | 3 (6.52) | 13 (28.26) | 30 (65.21) | 46 (44.66) |
| Obesity | 1 (7.14) | 5 (35.71) | 8 (57.14) | 14 (13.59) |
*Isolated systolic and isolated diastolic hypertension, BMI-Body mass index, ENT-Ear, nose and throat
Association between socio-demographic variables and hypertension, overweight.
| Sociodemographic variables | Overweight | Statistics | High BP | Statistics |
|---|
| No | Yes | Yes | No |
|---|
| Age group (years) |
| ≤=37 | 22 | 24 | *OR=2.57, **χ2=4.41, *p=0.03 *CI=1.06-6.26 | 25 | 21 | OR=5.60, χ2=13.77, p<0.001 CI=15.31-2.44 |
| >37 | 40 | 17 | 10 | 47 |
| Education |
| Illiteracy/Primary | 38 | 48 | OR=1.90, χ2=0.74, p=0.39 CI=0.56-7.46 | 25 | 61 | OR=0.29, χ2=4.35 p=0.03 CI=0.08-0.95 |
| Middle/Secondary/Higher | 5 | 12 | 10 | 7 |
| Social class as per BG Prasad’s SES |
| Class II/III | 8 | 13 | OR=0.76, χ2=0.09, p=0.75 CI=0.24-2.24 | 5 | 19 | OR=0.46, χ2=1.43, p=0.23 CI=0.12-1.45 |
| Class IV/V | 35 | 43 | 30 | 52 |
*OR=Odds ratio, BP=Blood pressure, CI=Confidence interval, p=significance value
**Chi square test was applied
Association of morbidities with various factors of beedi rolling.
| Variables | Morbidities (Frequency) | Overweight/obesity |
|---|
| Eye | Musculoskeletal | Hand | Blood pressure |
|---|
| Age (years) of initiation of beedi making (total number) |
| <15 (29) | 13 | 17 | 11 | 8 | 15 |
| 15-30 (52) | 29 | 36 | 26 | 16 | 31 |
| >30 (22) | 16 | 16 | 12 | 9 | 14 |
| Statistics | *χ2=3.97 p=0.137 | χ2=1.36p=0.506 | χ2=1.63 p=0.442 | χ2=2.27 p=.321 | χ2=0.81 p=0.666 |
| Duration (years) of work (total number) |
| 1-10 (42) | 21 | 27 | 21 | 10 | 24 |
| 11-20 (31) | 14 | 22 | 14 | 13 | 17 |
| >20 (30) | 23 | 20 | 14 | 10 | 19 |
| Statistics | χ2=7.29 **p=0.026 | χ2=0.36p=0.834 | χ2=0.18 p=0.913 | χ2=20.22 **p=0.027 | χ2=0.49 p=0.783 |
| Hours per day (total number) |
| 1-3 (24) | 18 | 18 | 15 | 5 | 11 |
| 4-6 (65) | 29 | 40 | 26 | 20 | 39 |
| >6 (14) | 11 | 11 | 8 | 8 | 10 |
| Statistics | χ2=9.84 **p=0.007 | χ2=2.41 p=0.298 | χ2=4.15 p=0.125 | χ2=5.48 p=0.061 | χ2=2.60 p=0.272 |
| Days/month (total number) |
| 1-10 (28) | 13 | 20 | 13 | 8 | 17 |
| 11-20 (21) | 14 | 15 | 8 | 7 | 13 |
| 21-30 (54) | 31 | 34 | 28 | 18 | 30 |
| Statistics | χ2=2.05 p=0.358 | χ2=0.833 p=0.659 | χ2=1.56 p=0.558 | χ2=5.48 p=0.899 | χ2=0.35 p=0.850 |
| Beedi rolled/day (total number) |
| 100-500 (61) | 34 | 35 | 25 | 17 | 31 |
| >500 (42) | 24 | 34 | 24 | 16 | 29 |
| Statistics | χ2=0.02 p=0.525 | χ2=6.25 **p=0.012 | χ2=2.60 p=0.107 | χ2=1.19 p=0.274 | χ2=3.40 p=0.065 |
*chi-square test was done, **p<0.05
Line diagram showing trends of blood pressure with age.
Scatter diagram of BMI variation with age.
Discussion
Occupational health hazards are showing an upward trend throughout the world and India is no exception [1,2]. There is a huge impact on their health due to long hours of sitting in uncomfortable posture and regular, consistent exposure to tobacco dust and fumes. Despite a hazardous profession, their health and working conditions have rarely been brought into limelight of public discussion and awareness.
Socioeconomic, Demographic and Environmental Variables
The mean (SE) age of workers 38.69 (±8.53) years was comparable with coastal Karnataka Study 40.8 (±11.3) years, while the mean age was more in some other studies [20-24]. Publication from West Bengal and south India reported nearly similar proportion of marriage (91% and 88% vs. 97%) [7,22]. Majority of respondents lived in nuclear family comparable to South Indian studies, though Murshidabad study reported difference in family type with more in favour of joint one and this may be due to geographical difference [7,20,22]. In our study, hypertension was significantly more in respondents with lesser education maybe due to less awareness about the lifestyle correlates. The illiteracy rate in present study found to be quite similar with South India and Mumbai study [20,23]. The illiteracy rate of Murshidabad study was less (6.7%), the difference might be due to the difference in the eligibility criteria of an illiterate, as we included those women who can read or read and write only, in addition to those without any letter introduction [7]. There was wide variation in age group distribution in their study population [Table/Fig-7]. Mumbai slum study using BG Prasad’s scale had revealed similar social class structure as present study [Table/Fig-8] [23]. Overcrowding was present in almost all the houses in the south Indian study [22].
Discussion on variables of a West Bengal study vs. present study.
| Demographic variables | Previous West Bengal study (n=120),% | Our study (n=103),% | Health profile | Previous West Bengal study | Present study |
|---|
| Age group | Chronic cough |
| <20 years | 13.30 | 1.90 | Yes | 76.70 | 36.90 |
| 20-60 years | 40.00 | 98.10 | No | 23.30 | 63.10 |
| >60 years | 46.70 | 0.00 | Sore throat, hoarseness |
| Type of family | Yes | 64.20 | 19.40 |
| Nuclear | 39.20 | 58.30 | No | 35.80 | 80.60 |
| Joint | 60.80 | 48.70 | Headache |
| Education | Yes | 72.50 | 68.00 |
| Illiterate | 36.70 | 40.77 | No | 27.50 | 32.00 |
| Primary, middle | 50.00 | 42.71 | Weakness in hand |
| Secondary and above | 13.30 | 16.52 | Yes | 55.80 | 29.10 |
| Marital status | No | 44.20 | 70.90 |
| Unmarried | 6.70 | 1.90 | Fatigue/irritation in arm, hand |
| Married | 91.70 | 97.10 | Yes | 59.20 | 56.30 |
| Divorce/widow | 1.70 | 1.00 | No | 40.20 | 43.70 |
| Family size | Blood pressure |
| Up to 5 members | 29.20 | 74.70 | Normal, low | 34.10 | 34.00 |
| >5 members | 70.80 | 25.30 | High | 65.80 | 66.00 |
Discussion on background information of beedi workers with factors of beedi rolling in previous studies with present study.
| Variables | Coastal Karnatakastudy (n=439) | Mangalorestudy (n=100) | Mumbaistudy(n=52) | Present study (n=103) |
|---|
| Prevalent age group (year) | 35-44(32%) | 35-44(32%) | 40-50(26.9%) | 38-47(33.9%) |
| Mean age (year) | 40.8 | 36 | 45 | 38.6 |
| Gender |
| Female | 98.2% | 100.0% | 100.0% | 100.0% |
| Male | 1.8% | 0.0% | 0.0% | 0.0% |
| Variables (Misc.) |
| Hindu | | 96.0% | 100.0% | 100.0% |
| Muslim/Christian | | 3.0% | 0.0% | 0.0% |
| Illiterate | 22.0% | 57.0% | 42.3% | 40.7% |
| Married | 75.0% | | 88.0% | 97.0% |
| Social status |
| *Higher PCI | 40.3% | 0.0% | **Class III (25.0%)Class IV(42.3%) | 20.3% |
| Lower PCI | 50.7% | 100.0% | | 79.7% |
| Duration of beedi rolling (in years) |
| 1-10 | 24.0% | 31.0% | | 31.1% |
| 11-20 | 32.0% | 30.0% | | 36.0% |
| >20 | 44.0% | 39.0% | 26.9% | 32.9% |
| Average working day/(month) | 5.24 | 5 | | 20.0 |
| Average working hours/(day) | 5.6 | 5 | 8 | 4.9 |
| No. of beedi rolled/(day) | 300-800 | 300-500 | 500-1000 | 100-1000 |
*PCI=Per capita income, ** BG Prasad’s scale
Mean duration of work, average working hours and rolled beedi per day was quite similar to our study. Most of the women joined this job due to financial burden and family tradition [20,22-25]. The starting age of beedi rolling was similar to previous studies. Women worked on daily wages like in the previous studies [22,23].
Morbidity profile: Beedi rolling is an important cause of significant health hazards as cited by the International Labour Organisation that there is exacerbation of different health hazards like asthma, anaemia, giddiness, vertigo, postural problems, eye problems among beedi workers [23]. Mangalore study reported less prevalence of breathlessness and palpitation than our study [26]. Other research groups also found breathlessness and ischaemic heart disease [20-22]. Cough, common cold, sore throat, sneezing were reported in earlier studies with variable proportions (9-76% vs. 30%) [7,20,22,26-28]. Previous studies reported wide variety of eye symptomsas found in our study [21-23,25]. Mittal S et al., study also reported similar eye problems [25]. Musculoskeletal system was the most commonly involved system in addition to eye. Earlier studies also supported the findings [7,21-24,26]. The study of Murshidabad district showed that some symptoms were more among their workers while the proportion of some morbidity corroborated with our findings. The improvement of respiratory symptoms in workers of present study might be as a result of less pollution and better housing condition than the reference study [Table/Fig-8]. The prevalence of pallor reported was less than the South India study (19.41% vs. 40%). The difference was attributed to the gap between laboratory findings and observation [Table/Fig-9] [20]. Skin diseases like allergy, callosities, tanning was also reported from other studies [24,25,27]. The mean height (1.50 mm vs.1.48 mm) of the workers was close to present study, but the weight was more in current one (51.82 kg vs. 57.12 kg) [21]. The proportion of beedi workers with high BP in a study from West Bengal was similar to current study (65.80% vs. 66%) [7]. Age, education status, social class, number of working hours, duration of work was associated with different health hazards. The present study also revealed similar results [21,25, 27].
Discussion on morbidity profile of beedi workers of present study with previous studies.
| Morbidities | Mangalore study | Mumbai study | Present study |
|---|
| Cough | 32.0% | 13.5% | 36.8% |
| Breathlessness | 14.0% | 21.2% | 31.0% |
| Palpitation | | 36.5% | 55.3% |
| Headache | 36.4% | 32.7% | 67.9% |
| Blurring of vision | 13.0% | 26.9% | 60.1% |
| Double vision | | 23.5% | 18.4% |
| Low back pain | 35.0% | 78.8% | 66.0% |
| Weakness of hand | 13.0% | 7.7% | 29.1% |
| Pallor | 15.0% | 75.0% | 19.4% |
| Hyperacidity/Epigastric pain | 39.0% | 23.1% | 39.8% |
The present study revealed that more than one third respondents are not literate and the living condition is inadequate. The workers rarely practiced any safety measures and were completely unaware of any laws benefitting them. Some morbidity are significantly more with increasing working hours cum years, age of workers and also with more number of beedi rolling. Many workers of the unorganised sectors still lived with morbidities without self concern.
Limitation
The study would be more appreciable if some aspects on the social security measures could be included. As the study was a self-financed study within stipulated time, therefore, the subclinical cases could not be identified. The recall bias of the participants may not reveal the actual morbidity scenario. Therefore, a multi-centric elaborative study can be done in future including integrating laws and policies. Qualitative research will be the best kind of research for exploring the specific issues.
Conclusion
The present research highlighted the role of women in household finance. The most common system involved was musculoskeletal followed by eye, respiratory system. Awareness regarding adverse effects of beedi rolling and safety measures were very poor among the workers.
*Isolated systolic and isolated diastolic hypertension, BMI-Body mass index, ENT-Ear, nose and throat
*OR=Odds ratio, BP=Blood pressure, CI=Confidence interval, p=significance value
**Chi square test was applied
*chi-square test was done, **p<0.05