Neuropathic Shoulder Joint Associated with Syrinx and Chiari Malformation Type I Clinically Masquerading as Malignancy-A Case Report
Ruchi Gupta1, Kishore Kunal2, Subhash Kumar4, Neetu Sinha4, Abhishek Anand5
1 Senior Resident, Department of Radiodiagnosis, All India Institute of Medical Sciences, Patna, Bihar, India.
2 Senior Resident, Department of Orthopaedics, All India Institute of Medical Sciences, Patna, Bihar, India.
3 Assistant Professor, Department of Radiodiagnosis, All India Institute of Medical Sciences, Patna, Bihar, India.
4 Senior Resident, Department of Radiodiagnosis, All India Institute of Medical Sciences, Patna, Bihar, India.
5 Senior Resident, Department of Ophthalmology, All India Institute of Medical Sciences, Patna, Bihar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ruchi Gupta, Room No-706, PG1 Hostel, All India Institute of Medical Sciences, Phulwari Sharif-801507, Patna, Bihar, India.
E-mail: drruchigupta28@gmail.com
We report a rare case of 40-years-old male patient who presented with right shoulder joint swelling and reduced range of motion since one and half month. Subsequent X-ray and Magnetic Resonance Imaging (MRI) revealed completely resorbed humeral head, extensive intra-articular debris, joint effusion and thickened synovium. MRI of whole spine showed long segment syrinx, pointed peg of tonsils with tonsillar ectopia and basilar invagination. Diagnosis of atrophic type of Neuropathic shoulder joint secondary to syrinx and Chiari malformation was made.
Chiari malformation, Chondrosarcoma, Neuropathic joint, Shoulder joint, Syrinx
Case Report
A 40-year-old male patient, labourer by profession, presented to Orthopaedics department with progressively increasing swelling of the right shoulder joint since one and a half month along with mild dull aching pain. He had no history of fever, trauma, cough, weight loss, discharge, other comorbidity or drug allergy. There was no history of similar illness in the past. No similar family history was present. No history of any spinal cord disease and no systemic symptoms were present. On examination, patient was fairly built with no signs of clubbing, cyanosis, icterus or pallor. On local joint examination, an ill defined soft swelling was present at right shoulder measuring about 6×6 inches and overlying skin was normal. No local rise of temperature was seen. Range of motion was Flexion 0-90°, Abduction 0-90°, internal rotation 0-90° and External rotation 0-10°, Franklin test was negative, abdominal push off and lift up test were positive. Right axillary lymph nodes were palpable. Routine blood tests were normal. Clinically, diagnosis of malignancy was made as primary provisional diagnosis. The patient was referred to the department of Radiodiagnosis for the investigations.
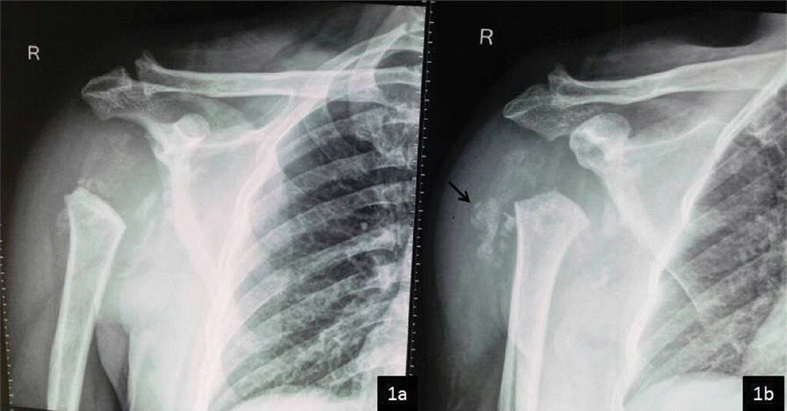
Plain radiography of right shoulder joint revealed destruction of entire head of humerus as well as multiple bony fragments surrounding the joint and overlying soft tissue swelling. The bone mineralisation of the uninvolved bones was normal [Table/Fig-1].
X-ray AP view of right shoulder joint a) and Oblique view b) shows complete destruction of humeral head, widening of gleno-humeral joint space, multiple osseous debris (black arrow) and overlying soft tissue swelling. Based on X-ray findings, diagnosis of Neuropathic joint was made.
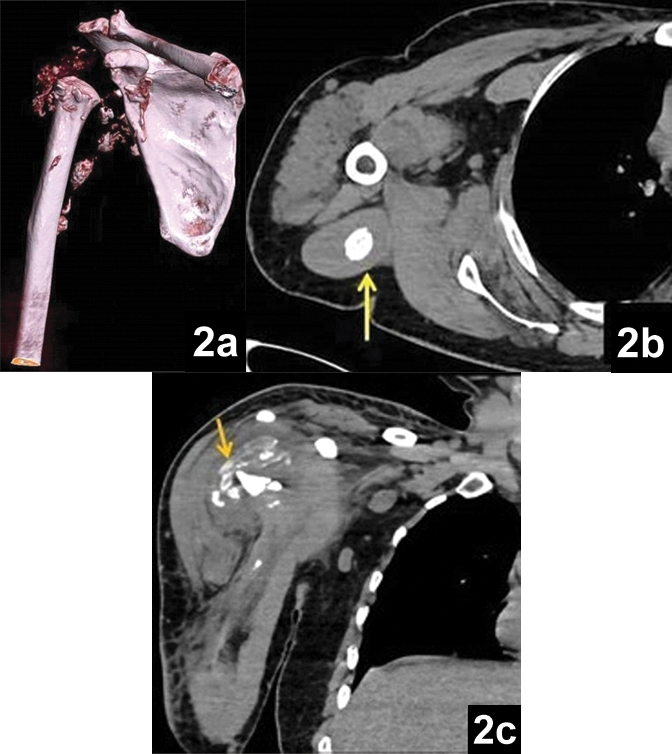
Subsequently, Computed Tomography (CT) and MRI were performed. Unenhanced CT and contrast enhanced MRI showed destruction of head of humerus and glenoid fossa with multiple bony debris within the joint cavity and adjacent muscles with markedly thickened and enhancing synovium and joint effusion [Table/Fig-2,3].
a) Volume rendered image (VRT) showing amputated articular end of humerus and glenoid fossa and multiple periarticular osseous debris; b) Axial soft tissue image showing bony fragment within the triceps muscle (yellow arrow); c) Coronal reformatted image showing fluid collection with multiple osseous fragments within.
a) Axial T1 image showing fatty infiltration of supraspinatus muscle (red arrow); b) Coronal T2 Fat Sat image showing gross joint effusion with thickened peripheral synovium (white arrow), destroyed humeral head and flattening of glenoid. Subchondral cyst seen within acromion process (yellow arrow); c) Post contrast Coronal T1 fat sat image showing peripherally enhancing synovium (blue arrow), enhancing synovium within acromioclavicular joint with articular surface irregularity (green arrow), hypointense bony debris (purple arrow) and enhancing supraspinatus muscle (red arrow).
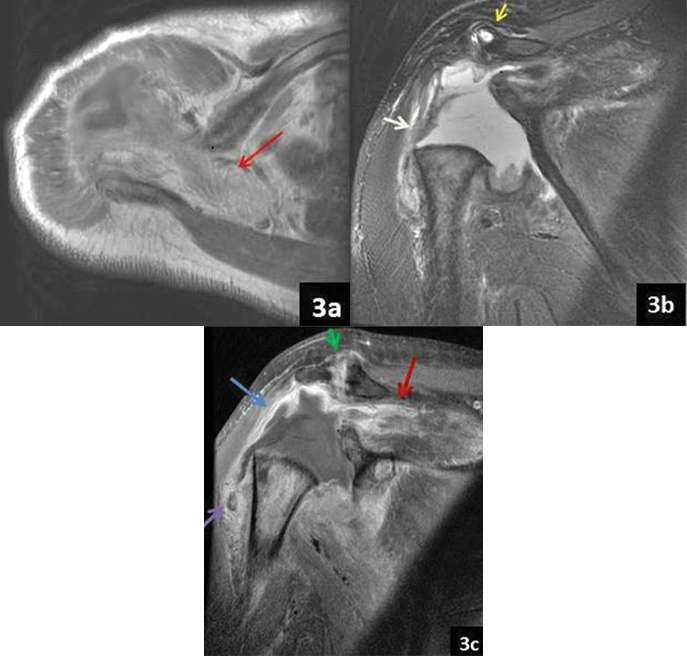
Multiple hypointense foci were seen within and surrounding the joint cavity and within triceps muscle on T2 weighted images to suggest bony debris. There was complete involvement with heterogeneous signal of rotator cuff tendons with heterogeneous enhancement of the muscle belly of supraspinatus, infraspinatus, subscapularis, teres minor, triceps and deltoid muscle. Marked fatty degeneration of supraspinatus muscle and mild fatty atrophy of subscapularis and infraspinatus tendon was seen. There was involvement of acromioclavicular joint with cortical irregularity and subchondral cyst in acromion process with joint effusion, thickened and enhancing synovium [Table/Fig-3].
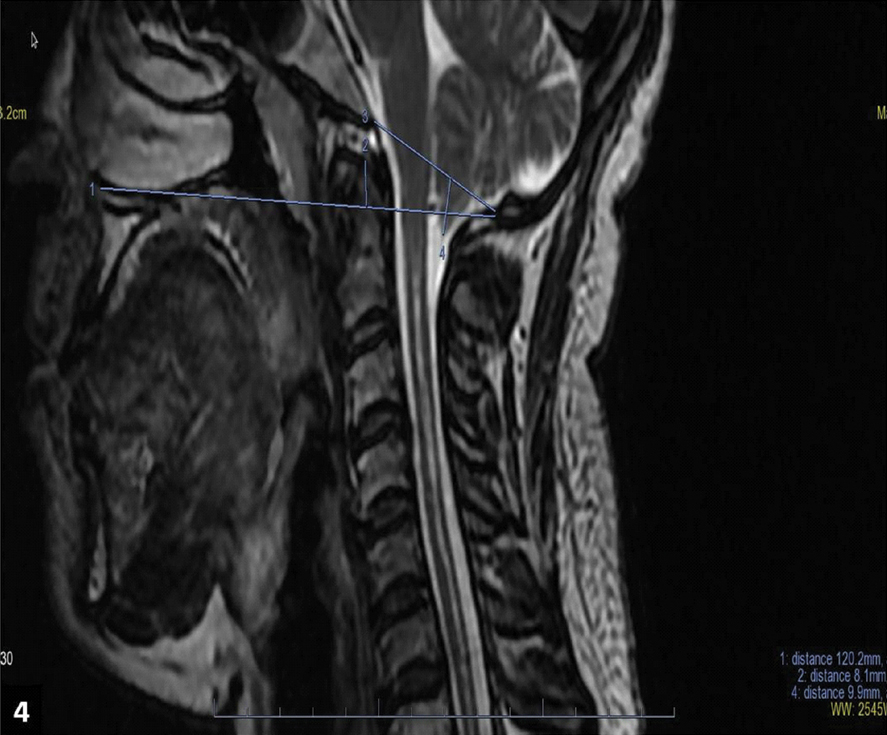
MRI of the spine revealed long segment syrinx from C2 to D4 vertebral body level. Tip of odontoid process was about 8 mm above Chamberlain’s line. Pointed peg of tonsil was about 9 mm below the foramen magnum [Table/Fig-4]. Based on above clinic radiological profile, diagnosis of neuropathic shoulder joint secondary to Chiari Malformation type I associated with syringohydromyelia was made. Patient was referred to Neurosurgery department for decompression of syrinx and was put on conservative management in the form of limb immobilisation and splinting of the joint. Later, patient was advised physiotherapy in the form of ultrasonic therapy, shoulder muscle strengthening and range of movement exercises. Patient gradually improved strength and range of movement following three months of treatment.
Sagittal T2 weighted image shows long segment syrinx, pointed peg of tonsils at foramen magnum and basilar invagination.
Discussion
Neuropathic osteoarthropathy is a disease entity that occurs secondary to loss or impairment of joint proprioception leading to severe destruction and instability of joint. Neuropathic joint is also known as Charcot’s joint which was first described by Jean-Martin Charcot in 1868 [1]. Less than 100 cases of Charcot’s shoulder have been reported in the literature [2].
Radiographically neuropathic joint can have two patterns, hypertrophic and atrophic. Hypertrophic pattern is characterised by six Ds-joint distension, increased subchondral density, debris, dislocation, disorganisation and bone destruction. This is more commonly seen in weight bearing joints of lumbar spine, hip, knee and ankle. Atrophic pattern is characterised by amputation of articular ends of bones or tapering of bone towards joint space known as licked candy stick appearance. This is more commonly seen in non weight bearing joints of upper extremity like shoulder, elbow, wrist as well as hip joints [1]. However, joint disorganisation and large joint effusion are features of both atrophic and hypertrophic forms [3].
Two theories explain its pathogenesis. Neurotraumatic theory describes multiple episodes of microtrauma sustained by insensitive joint [4]. Neurovascular theory explains the active bone resorption by osteoclasts stimulated by sympathetic dysfunction [5]. Of all causes, diabetes is the most common and affects mainly the ankle [6]. Neuropathic joint is relatively uncommon in non weight bearing joints.
Amongst all causes, syrinx is the most common cause of neuropathic shoulder joint [3, 7]. Other rare causes are leprosy and diabetes mellitus. The other neurological causes include spinal cord tumors, extrinsic compression of cord, familial multiple sclerosis and peripheral nerve tumours [3]. Type I Chiari malformation is characterised by herniation of cerebellar tonsils through foramen magnum into the cervical canal. All forms of Chiari Malformation can be associated with Syrinx. Syrinx causes block of lateral spinothalamic tract, anterior horns of spinal cord, posterior columns and sympathetic tract which cause loss of pain, thermal and touch sensations which could be the cause of repeated microtrauma [6].
Usually, the disease has a variable progression which may range from few months to years. In our case, the symptoms were present for only one and half month and disease progressed rapidly [6]. Due to fast progression, chondrosarcoma and septic arthritis were the main differentials. However, patient did not have other systemic or local features of infection and the routine laboratory investigations were normal. There was no solid component except the enhancing synovium and malignancy usually do not cross the joint line as in this case there was destruction of glenoid fossa as well, ruling out the possibility of neoplasm. Other less common differentials of neuropathic joint are Idiopathic osteolysis and synovial chondromatosis [2].
Conclusion
In a patient presenting with reduced mobility and swelling of joint where pain is not the chief complaint, possibility of neuropathic joint should be considered. Radiologically, presence of destruction of articular ends of bone, periarticular bony debris, synovial thickening and joint effusion confirms the neuropathic nature of joint. In case of shoulder joint, syrinx is the most common etiological factor and cervical MRI should be included in the radiological workup.
[1]. Yochum TR, Rowe LJ, Essentials of Skeletal Radiology 2005 Third EditionUnited States of AmericaLippincott Williams and Wilkins [Google Scholar]
[2]. Belkin NS, Hung G, Lewullis GE, Neuropathic arthropathy of the glenohumeral joint as the presenting symptom of a cervical syrinx: university a case report of pennsylvaniaOrthopaedic Journal 2015 25:58-60. [Google Scholar]
[3]. Jones EA, Manaster BJ, May DA, Disler DG, Neuropathic osteoarthropathy: diagnostic dilemmas and differential diagnosisRadiographics 2000 20:279-93.10.1148/radiographics.20.suppl_1.g00oc22s27911046179 [Google Scholar] [CrossRef] [PubMed]
[4]. Johnson JT, Neuropathic fractures and joint injuries. Pathogenesis and rationale of prevention and treatmentJ Bone Joint Surg Am 1967 49(1):01-30.10.2106/00004623-196749010-00001 [Google Scholar] [CrossRef]
[5]. Allman RM, Brower AC, Kotlyarov EB, Neuropathic bone and joint diseaseRadiol Clin North Am 1988 26(6):1373-81. [Google Scholar]
[6]. Park J, Im T, Moon J, Lee Y, Neuropathic arthropathy of the shoulder associated with cervical syringomyelia: a case reportClinics in Shoulder and Elbow 2015 18(4):261-65.10.5397/cise.2015.18.4.261 [Google Scholar] [CrossRef]
[7]. Kenan S, Lewis MM, Main WK, Hermann G, Abdelwahab IF, Neuropathic arthropathy of the shoulder mimicking soft tissue sarcomaOrthopedics 1993 16(10):1133-36. [Google Scholar]